

Original Article - Year 2016 - Volume 31 -
Lower eyelid blepharoplasty with lateral canthal support
Blefaroplastia inferior com suporte cantal lateral
ABSTRACT
INTRODUCTION: The transcutaneous approach in lower eyelid rejuvenation is a versatile technique allowing broad access to all periorbital structures. Nevertheless, many surgeons opt to use different access routes such as the transconjunctival approach, to avoid the increased risk of eyelid malposition. However, the use of a routine lateral canthal support was shown to consistently minimize this risk. This study reviewed 136 cases of patients who were operated on using the transcutaneous approach and canthal support with canthopexy and orbicularis suspension.
METHOD: Our study used a retrospective design to investigate patients undergoing primary transcutaneous lower blepharoplasties performed with canthopexy, between January 2008 and January 2014. We assessed the presence of dermatochalasis, eyelid bags and tarsal sagging by analyzing patients' images and medical records. We used surgical descriptions and clinical notes to study the surgical technique used and the rate of complications associated with the same.
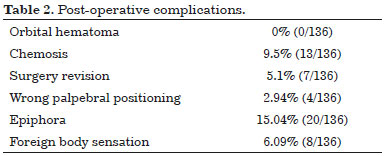
RESULTS: Our study involved monitoring the post-operative condition of 136 patients for approximately 180 days after they underwent surgery. The occurrence of any of the following was considered a postoperative complication: epiphora (15%), eyelid malposition (2.94%), orbital hematoma (0%), chemosis (9.5%), and foreign body sensation (6%). Seven patients (5.1%) required surgical revision.
CONCLUSION: Our assessment revealed that canthal support must be considered as an integral part of transcutaneous lower blepharoplasty. The authors believe that canthopexy is a good option in primary cases owing to its easy implementation, low morbidity, and efficacy in preventing apparent sclera, round eye lateral corner, and ectropion.
Keywords: Blepharoplasty; Eyelid surgery; Ectropion.
RESUMO
INTRODUÇÃO: A abordagem transcutânea no rejuvenescimento palpebral inferior é uma técnica versátil e que permite amplo acesso a todas as estruturas periorbitárias. Apesar disso, muitos têm optado por outras vias de acesso, como a transconjuntival, devido ao risco aumentado de mal posicionamento palpebral. A utilização de suporte cantal lateral de rotina tem sido indicada sistematicamente para minimizar este risco. O presente trabalho revisou 136 casos operados com acesso transcutâneo e reforço cantal com cantopexia e suspensão orbicular.
MÉTODO: Estudo retrospectivo de casos de blefaroplastia inferior primária transcutânea com cantopexia operados entre janeiro de 2008 e janeiro de 2014. Foram avaliados, por meio de fotos e registro de prontuários, a presença de dermatocalasio, bolsas palpebrais e flacidez tarsal. A técnica cirúrgica e o índice de complicações foram obtidos a partir da descrição cirúrgica e anotações clínicas.
RESULTADOS: Foram operados 136 pacientes, com follow-up pós-operatório médio de 180 dias. Consideramos como complicações pós-operatórias epífora (15%), mal posicionamento palpebral (2,94%), hematoma orbital (0%), quemose (9,5%) e sensação de corpo estranho (6%). Sete pacientes (5,1%) precisaram de revisão cirúrgica.
CONCLUSÃO: A realização de suporte cantal deveria ser considerada como parte integrante da blefaroplastia inferior transcutânea. Os autores acreditam que a cantopexia seja uma boa opção nos casos primários por sua fácil execução, baixa morbidade e eficácia comprovada na prevenção da esclera aparente, do arredondamento do canto lateral do olho e ectrópio.
Palavras-chave: Blefaroplastia; Pálpebras/cirurgia; Ectrópio.
Lower blepharoplasty is one of the most challenging and widely performed procedures in plastic surgery. Noel was the first to describe this technique, carried out using a subciliary incision. Subsequently, Castanares described a modern blepharoplasty performed using a subseptal space approach. In 1967, McIndoe introduced the myocutaneous flap technique, which was rendered popular by Rees in 19701.
The procedure is similar to the technique described by other contemporary authors2,3 and became the "traditional surgery" carried out when lower blepharoplasty is indicated4. Since then, the techniques evolved considerably and several procedures have been described to aesthetically improve the eyelids and decrease the rate of complications4-8. Patients with tarsal sagging, negative intercanthal fissure inclination ('canthal tilt') and prominent eyes show a higher risk to develop complications such as scleral show and ectropion9, thus there is a need for surgical revision10.
Since several of these complications mainly result from the lack of eyelid support, many surgeons began repositioning of the orbicularis muscle by performing canthoplasty/canthopexy as adjuvant procedures to lower blepharoplasty1,2,10-12.
Semantically, canthopexy can be defined as the suspension of the lateral retinaculum that can be performed without cantholysis, while canthoplasty refers to similar procedures that require performing cantholysis. Consequently, canthopexy is indicated in cases of mild tarsal sagging, whereas canthoplasty is recommended when patients present with dystopia or scleral show11.
There are several techniques to reposition the eyelid in order to create tension on its outside corner. In this study, we used a form of minimally invasive canthal support, which is easily reproducible, presents a low rate of complications and is very similar to the earlier techniques described by Rizvi et al.11 and Lessa & Nanci13.
OBJECTIVE
The primary objective of this retrospective study was to assess the outcomes and rate of complications in cases of transcutaneous lower blepharoplasty with lateral canthopexy and traction of the orbicularis muscle, performed by the senior author in the study, and comparing these with previous literature.
METHOD
We carried out a retrospective study of primary lower eyelid blepharoplasty surgeries with canthal support, performed by the author from January 2008 to January 2014, in the municipality hospital of Criciúma, SC. Secondary cases, post-traumatic patients and individuals presenting with ophthalmopathy were excluded from the study. The study followed the principles of Helsinki.
All patients were evaluated using their preoperative medical records and patients' images, as well as by collecting data from evaluations and measurements taken during the preoperative and intra-operative period. These refer to the following:
- Presence of dermatochalasis and eyelid bags;
- Intercanthal fissure inclination or Canthal Tilt, considered positive when the side corner is positioned above the medial corner, neutral when positioned at the same level and negative when positioned inferiorly (Figure 1);
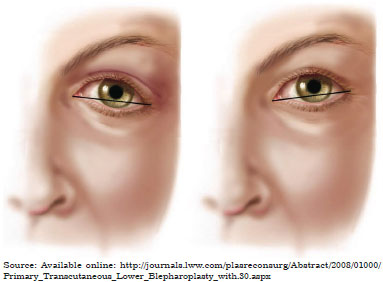
Figure 1. Canthal Tilt, defined by the line from the inner to the outer corner of the eye: (left) negative, the lateral corner remains below the medial corner; (right) positive, the lateral corner remains above the medial corner.
- Evaluation of the ciliary margin tonus, through the eyelid distraction test and Snap back test. In the distraction test, the lower lid is pulled anteriorly and the distance from the eyeball is measured. When the tarsal distance is lower than 6 mm from the eyeball, the sagging is considered mild and canthopexy is performed, while a distance of more than 6 mm indicates severe sagging and requires canthoplasty.Cases with an indication of canthotomy along with canthoplasty, release of the lower limb of the canthal ligament, and/or resection of 2-3 mm of the lateral tarsal and periosteal fixation, were excluded from the study. In the Snap back test, the eyelid is pulled inferiorly and then released; the delay in returning to the resting point indicates tarsal sagging (Figures 2 and 3).

Figure 2. Snap back test.

Figure 3. Distraction test.
Surgical complications were reviewed from the medical records and divided into the following categories: orbital hematoma, chemosis, palpebral malpositioning, epiphora, and foreign body sensation. The average follow-up period was 6 months, varying from 2 to 18 months. Photographic documentation was collected at 3 months, 6 months and 1 year.
Surgical technique
The surgery is divided into three stages: production of the myocutaneous flap, canthopexy, and traction of the orbicularis flap. The procedure was performed under local anesthesia and sedation, administered through the infiltration of an anesthetic vasoconstrictor solution (1:100,000). A cold blade, positioned in a pre-existing rhytid, was used to create a lateral incision in the outer corner, while its infraciliary portion was cut with scissors, preserving 4-5 mm of supratarsal orbicular muscle.
The myocutaneous flap was dissected into a supraseptal plane up to the level of the orbital rim, using a colored tip. The fat bags of all three compartments were treated conservatively, with minimum opening of the orbital septum and slight eyeball pressure. In cases of tear trough, the orbitomalar ligament and medial origin of the orbicularis muscle were released from the jaw, in a supraperiosteal plane.
Canthopexy was performed as described: following a classical upper blepharoplasty, a 10-mm resection of the orbicularis muscle was performed at the level of the superolateral edge of the orbit, to access the periosteum and fix the lateral eyelid corner. A 4-0 PDS thread was passed from the bottom to the top through the lower blepharoplasty incision, transfixing the superficial lateral canthal ligament and a lateral segment of the lower tarsal plate, as described in the classic work published by Knize7.
Finally, the suture was returned to the entry point, i.e. the superolateral edge of the orbit, suturing it in the periosteum at the level of the pupil, using a needle. It is very important that the traction exerted to lift the lateral corner stays on a plane below the orbicularis muscle and follows the lower eyelid curvature. This allows avoiding the removal of the eyelid edge from the eyeball. Therefore, about 1 to 2 millimeters of the lower limb was covered (Figure 4).
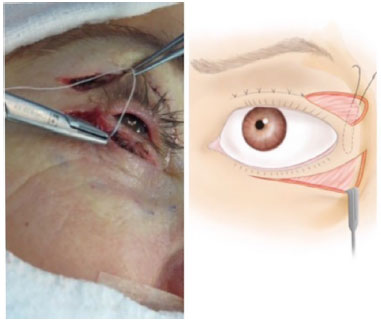
Figure 4. Canthopexy.
Traction of the orbicularis muscle
A muscle strip of 4 mm height was dissected from the myocutaneous flap and fixed to the periosteum of the lateral edge of the orbit with a 4-0 PDS thread. The slight horizontal traction and muscle strap effect promoted the traction and repositioning of the entire myocutaneous flap. Excess muscle was then resected (Figure 5).
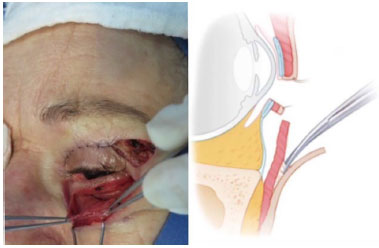
Figure 5. Orbicularis muscle flap.
RESULTS
The author performed 136 lower blepharoplasties with canthopexy. Majority of the patients were females (87.5%), with an average age of 52 years (37-72 years). The epidemiological and morphological information collected from preoperative images are shown in Table 1.
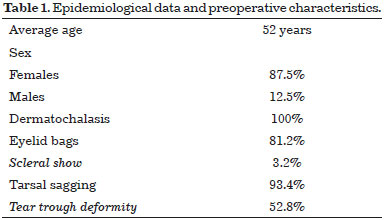
Associated complications are described in Table 2. The occurrence of subcutaneous hematoma, observed in hypertensive patients, was not considered as a complication. Poor outcome (n = 3), ectropion (n = 2), and scleral show (n = 2) were indications for surgical revision. When no results were obtained, a non-surgical complementary treatment was performed (n = 1) with a CO2 laser. A new bags resection using a transconjunctival approach, was performed in two cases.
Chemosis is defined as the visible swelling of the bulbar sclera. This occurred in 9.5% of the cases, none of which required surgical treatment. Three patients required transient palpebral occlusion, performed with frost point.
Wrong eyelid position was classified as mild when there was only one round corner; moderate in cases of apparent sclera or scleral show (appearance of 1 or more millimeters of sclera, inferiorly to the limb), and severe when accompanied by ectropion (removal or eversion of the ciliary margin in a direction opposite to the eyeball).
Based on the description of the techniques used, the images from the pre- and postoperative period of three patients have been shown (Figures 6 to 8).

Figure 6. A 53-year-old patient who underwent blepharoplasty and face lipofilling (pre- to post-operative period, 1 year).
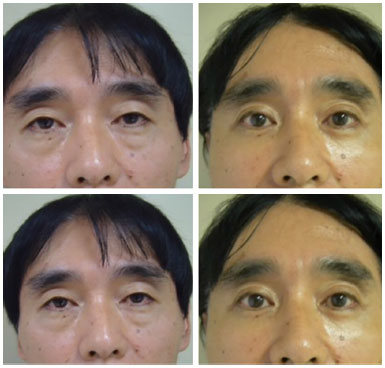
Figure 7. A 63-year-old Asian patient who underwent lower and upper blepharoplasty (pre- to post-operative period, 9 months).

Figure 8. A 55-year-old patient who underwent laparoscopic surgery of the forehead, blepharoplasty and face lipofilling (pre- to post-operative period, 7 months).
DISCUSSION
Blepharoplasty is one of the most common cosmetic surgical procedures performed in Brazil. Despite being a widely performed surgery, there is still great controversy between the procedures that are used, due to the high likelihood of postoperative complications and suboptimal results8.
The transcutaneous approach allows wide access to the infrapalpebral region and other structures located in that area. Although this procedure has excellent surgical outcomes, the complications related to eyelid malpositions are still of great concern14,18.
According to previous literature, this change occurs between 5 and 30% of the cases14-17. Codner et al.1 and Jelks et al.16 have indicated that only patients with severe tarsal sagging should be given lateral canthal support. In contrast, Flowers19, Macêdo et al.2, and Basile18 recommend some type of reinforcement or routine canthal support for all patients. In keeping with these recommendations, Rohrich et al.8 recently proposed a five-step surgical lower blepharoplasty approach, one of the steps being lateral canthal support.
In this work, the incidence of wrong eyelid position was only 2.94% when routine canthopexy was used in blepharoplasty procedures, far below the rate reported in previous studies14-17. Ectropion, scleral show, and palpebral retraction suggest the occurrence of eyelid malposition. The main etiological factors for these complications include anterior and/or posterior lamella deficiency and tarsal-ligament sagging1. Therefore, it is very important to correct posterior lamella sagging with canthopexy, as well as to support the anterior lamella and improve its muscle tone by performing a myotomy procedure with lateral suspension of the orbicularis20.
Lateral canthopexy was originally used in reconstructive surgeries. In 1983, however, McCord began using it in cosmetic blepharoplasty. Modern canthopexy techniques are less destructive and complex, and can be performed with or without cantholysis techniques21-22. Lateral temporary tarsorrhaphy with frost point is another alternative for palpebral support that is simple and very useful in elderly patients requiring cutaneous resection and other selected cases to control/contain the development of chemosis and early eyelid malposition5.
Besides rejuvenating the lateral corner and leaving it with an almond shape, canthopexy also improves the tone of the pre-tarsal portion of the orbicularis muscle. Therefore, canthopexy might also have an aesthetic effect, especially in patients with early and subtle dystopia of the lower eyelid4.
A well-known cause of canthal dystopia and eyelid retraction is excessive resection of the skin. The need to be conservative in this resection is therefore, widely emphasized in the literature on eyelid surgery1,8,18.
Another important consideration while performing blepharoplasty with myocutaneous access is the incision in the orbicularis, which must be made 4 to 5 mm below its insertion, leaving the dynamic pre-tarsal portion intact. Preserving this region confers stability on the eyelid, which not only maintains its pump function but also does not the eyelid to undergo further inferior displacements due to muscle weakness18.
Several authors still believe that orbicularis myotomy triggers denervation and worsens the occurrence of eyelid malposition3,9. However, several anatomical and electromyography studies have demonstrated the dual innervation of the orbicularis3,5,17,23. The internal canthal portion, responsible for eyelid tone, blinking and tear pumping mechanisms, is innervated by the buccal branch of the facial nerve and the extracanthal portion, responsible for the forced closure of the eyes and eyelid mimicry, is innervated by the zygomatic branch.
The classic eyelid incision performed in lower blepharoplasty divides the extracanthal portion of the orbicularis without changing its function or palpebral tone3,5,17,23. The study by DiFrancesco et al.17 showed, through electromyography and videographic investigations, that abnormal position function of the lower eyelid upon transcutaneous blepharoplasty, cannot be attributed to the denervation of the orbicularis. Indeed, 94% of patients that presented with an eyelid malposition in the video, showed no evidence of acute denervation when submitted to electromyography.
Another fact supporting the theory that orbicularis myotomy is not the cause of eyelid malposition, is that even patients operated on using the transconjunctival approach2 present with a post-operative apparent sclera and/or round corner. Even non-surgical procedures involving CO2 lasers or fillings with hyaluronic acid can cause canthal dystopia, due to a local inflammatory reaction and/or septal retraction3,6,18.
Taking this into account, guaranteeing good tarsal support is more important than the access chosen for the surgery, especially in patients already at risk for eyelid malposition, such as those presenting with prominent eyes and negative canthal tilt 15.
In patients developing ectropion, a tarsal strip and/or a skin graft was used to correct the ectropion; we believe there is probably an error in evaluating the preoperative status in these cases. These patients present with significant tarsal sagging and a palpebral distraction of more than 6 mm. Therefore, tarsal shortening is indicated in these cases to improve the support of the posterior lamella. The apparent sclera was treated conservatively with massage and tarsorrhaphy. In refractory cases, retraction release was carried out in the anterior lamella along with a skin graft. We were not required to correct the retraction in the posterior lamella or to use cartilage grafts in the tarsus in any of the patients.
Chemosis is defined as the visible swelling of the bulbar conjunctiva15,16. It has a multifactorial etiology and is a minor, although more common complication of lower blepharoplasties. According to previous studies, the incidence of chemosis is up to 11.5%23-25. In our cohort, this was the second most common complication. The cause of chemosis, while poorly understood, is multifactorial. It is believed that surgical dissection causes conjunctival edema due to increased vascular permeability, and damages the lymphatic channels5.
The systematic use of corneal shields and ophthalmic lubricants, in addition to tarsorrhaphy with frost point in select cases, greatly diminished its occurrence. Topical and oral corticosteroids and night eye occlusion were efficiently used in the conservative treatment. No patient required surgical treatment with conjunctivectomy20.
The most common postoperative complaint was epiphora, which was seen in 15% of the cases. Only half the number of these patients reported this complaint on their own; its occurrence in the other half was detected by the surgeon. Tearing, which presented as a benign complaint in almost all cases, spontaneously resolved itself at the end of the first month.
Canthal support, classified by its several approaches, should be included in current blepharoplasty procedures. We believe that, with the techniques available at present, canthopexy must be considered along with the most appropriate type of canthal support in each case.
Recently, Tepper et al.15 reviewed the indication of various techniques of lateral canthoplasty according to a check list of seven pre-operative findings: (1) prominent eyes revealed by vector analysis, (2) tarso-ligamentous sagging, (3) apparent sclera, (4) negative canthal tilt, (5) lateral distance corner-orbit, (6) position of the middle third and (7) vertical restraints.
CONCLUSION
Although retrospective, our study describes lower transcutaneous blepharoplasty as a reproducible surgical technique with low complication rates. Canthal support should be considered as an integral part of lower blepharoplasty in all patients. The authors believe that canthopexy is a good course of treatment in primary cases, owing to its easy implementation, low morbidity and proven effectiveness in preventing apparent sclera, round eye lateral corner, and ectropion.
COLLABORATIONS
GJSAF Final approval of the manuscript, study elaboration and design, implementation of the procedures and/or realization of the experiments, writing of the manuscript, and/or critical reviewing of its content.
EF Writing of the manuscript and/or critical reviewing of its content.
LPSR Writing of the manuscript and/or critical reviewing of its content.
CH Writing of the manuscript and/or critical reviewing of its content.
REFERENCES
1. Codner MA, Wolfli JN, Anzarut A. Primary transcutaneous lower blepharoplasty with routine lateral canthal support: a comprehensive 10-year review. Plast Reconstr Surg. 2008;121(1):241-50.
2. Macêdo JE, Pessoa SGP, Pessoa BBGP, Almeida GS, Oliveira NGS, Gomes AAR. Cantopexia lateral como procedimento primário em blefaroplastia inferior. Rev Bras Cir Plást. 2009;24(1):30-5.
3. McCord S, Codner M, Nahai F, Hester R. Analysis of the nerve branches to the orbicularis oculi muscle of the lower eyelid in fresh cadavers. Plast Reconstr Surg. 2006;118(2):556-7.
4. Hidalgo DA. Discussion: Traditional lower blepharoplasty: is additional support necessary? A 30-year review. Plast Reconstr Surg. 2011;128(1):278-9.
5. Hidalgo DA. An integrated approach to lower blepharoplasty. Plast Reconstr Surg. 2011;127(1):386-95.
6. Pacella SJ, Nahai FR, Nahai F. Transconjunctival blepharoplasty for upper and lower eyelids. Plast Reconstr Surg. 2010;125(1):384-92.
7. Knize DM. The superficial lateral canthal tendon: anatomic study and clinical application to lateral canthopexy. Plast Reconstr Surg. 2002;109(3):1149-57.
8. Rohrich RJ, Ghavami A, Mojallal A. The five-step lower blepharoplasty: blending the eyelid-cheek junction. Plast Reconstr Surg. 2011;128(3):775-83.
9. Jindal K, Sarcia M, Codner MA. Functional considerations in aesthetic eyelid surgery. Plast Reconstr Surg. 2014;134(6):1154-70.
10. Stuzin JM. Endoscopic brow lift, upper and lower blepharoplasty, retinacular canthopexy: personal approach. Plast Reconstr Surg. 2007;120(6):1697-8.
11. Rizvi M, Lypka M, Gaon M, Eisemann B, Eisemann M, Lypka M. A simplified lateral canthopexy technique. Plast Reconstr Surg. 2010;125(6):248e-9e.
12. Marcellius BW, Nigro VAS, Dalcumune F, Netto RFB, Freitas EDT. Retalho de músculo orbicular nas blefaroplastias inferiores. Rev Bras Cir Plást. 2010;25(Supl):1-102.
13. Lessa S, Nanci M. Simple canthopexy used in transconjunctival blepharoplasty. Ophthal Plast Reconstr Surg. 2009;25(4):284-8.
14. Jacobs SW. Prophylactic lateral canthopexy in lower blepharoplasties. Arch Facial Plast Surg. 2003;5(3):267-71.
15. Tepper OM, Steinbrech D, Howell MH, Jelks EB, Jelks GW. A retrospective review of patients undergoing lateral canthoplasty techniques to manage existing or potential lower eyelid malposition: identification of seven key preoperative findings. Plast Reconstr Surg. 2015;136(1):40-9.
16. Jelks GW, Jelks E, Steinbrech DS. When must a lateral canthoplasty be done? a precise evaluation of the lower eyelid for an algorithm to select the most appropriate canthoplasty technique. Plast Reconstr Surg. 2006;118(Suppl 4):178-9.
17. DiFrancesco LM, Anjema CM, Codner MA, McCord CD, English J. Evaluation of conventional subciliary incision used in blepharoplasty: preoperative and postoperative videography and electromyography findings. Plast Reconstr Surg. 2005;116(2):632-9.
18.. Basile FVA. Correção das retrações palpebrais secundárias à blefaroplastia. Rev Bras Cir Plást. 2011;26(2):228-42.
19. Flowers RS. Canthopexy as a routine blepharoplasty component. Clin Plast Surg. 1993;20(2):351-65.
20. Couch SM, Buchanan AG, Holds JB. Orbicularis muscle position during lower blepharoplasty with fat repositioning. Arch Facial Plast Surg. 2011;13(6):387-91.
21. Jelks GW, Glat PM, Jelks EB, Longaker MT. The inferior retinacular lateral canthoplasty: a new technique. Plast Reconstr Surg. 1997;100(5):1262-70.
22. Fagien S. Algorithm for canthoplasty: the lateral retinacular suspension: a simplified suture canthopexy. Plast Reconstr Surg. 1999;103(7):2042-53.
23. Pacella SJ, Codner MA. Minor complications after blepharoplasty: dry eyes, chemosis, granulomas, ptosis, and scleral show. Plast Reconstr Surg. 2010;125(2):709-18.
24. Maffi TR, Chang S, Friedland JA. Traditional Lower Blepharoplasty: Is Additional Support Necessary? A 30-Year Review. Plast Reconstr Surg. 2011;128(1):265-73.
25. Enzer YR, Shorr N. Medical and surgical management of chemosis after blepharoplasty. Ophthal Plast Reconstr Surg. 1994;10(1):57-63.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade do Extremo Sul Catarinense, Criciúma, SC, Brazil
3. Escola Paulista de Medicina, Universidade Federal de São Paulo, SP, Brazil
4. Clínica Belvivere de Cirurgia Plástica e Laser, Criciúma, SC, Brazil
Institution: Clinica Belvivere de Cirurgia Plástica e Laser, Criciúma, SC, Brazil.
Corresponding author:
Glayse June Sasaki Acacio Favarin
Rua Coronel Pedro Benedet, 505, sala 10 - Centro
Criciúma, SC, Brazil Zip Code 88801-250
E-mail: glaysejune@yahoo.com.br
Article received: July 26, 2015.
Article accepted: September 29, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter