ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Reconstruction of the Burnt Neck in the Acute Phase
Reconstrução do Pescoço Queimado na Fase Aguda
Articles -
Year2003 -
Volume18 -
Issue
3
Roberto Cammarota Jr
ABSTRACT
Deep burns to the anterior portion of the neck frequently cause significant deformities. The objective of this study is to describe a new surgical procedure for deep cervical burns, which tries to reduce the incidence of cervical retraction and improve the cervico mandibular angle. Over 5 years, 24 victims of deep cervical burns were treated surgically with the same technique, which consisted in debriding necrosed tissues, incising the platysma muscle at the laryngeal prominence from one angle to the other of the mandible and grafting with thicle skin according to the position of normal skin. The author concluded that this is a simple and safe procedure that provides good functional and esthetical results, is not costly, and prevents retracting sequelae.
Keywords:
Burns; neck burns; cervical reconstruction in the acute phase
RESUMO
Queimaduras profundas na face anterior do pescoço freqüentemente causam significantes deformidades. O objetivo do presente estudo é descrever um novo procedimento cirúrgico diante de queimaduras cervicais profundas, o qual procura diminuir a incidência de retrações cervicais e melhorar o ângulo cervicomandibular.
Durante 5 anos, 24 pacientes vítimas de queimaduras cervicais profundas foram tratados cirurgicamente com a mesma técnica, que consistiu em debridar precocemente os tecidos necrosados, incisar o músculo platisma na altura da proeminência laríngea de um ângulo a outro da mandíbula e enxertar com pele espessa conforme a disposição de pele íntegra.
O autor conclui ser um procedimento simples e seguro, de bons resultados funcionais e estéticos, pouco oneroso ao serviço e que previne seqüelas retrácteis.
Palavras-chave:
Queimaduras; queimaduras de pescoço; reconstrução cervical na fase aguda
INTRODUCTION
The cervical region is an exposed body structure; for that reason, its retraction processes are stigmatizing for patients, who frequently walk with their heads bowed; their self-esteem is also affected, in addition to poor functional performance, as it often impairs facial expression and phonation.
The neck follows the angle of the spine and, depending on the biotype and age, it may flex up to 40 degrees and stretch up to 75 degrees(1), considering that the cervico mandibular angle, in a neutral position will look more harmonious the closer it is to a right angle. When total extensive skin burns in the cervical region, heal by second intention, they inevitably evolve into mentothoracic bridles. When deep dermal burns reepithelize, they often suffer retractions, hypertrophies, and dyschromias. Burnt cervical tissues, debrided and grafted, especially with the use of thin skin, tend to evolve with loss of extension and increase of the cervicomandibular angle(2).
The neck has a superficial muscular structure called platysma, which often suffers the aggressions of cervical burns directty or indirectty. The platysma is a voluntary accessory muscle of the oral fissure, innervated by the facial nerve and irrigated by two main arterial pedicles-the mandibular branch of the facial artery and a branch of the thyroid artery. It is located on the anterolateral tela subcutanea of the neck, on the lower border of the mandible and on the mouth angle, and comprises the Superficial Musculoaponeurotic System of the face, going down through the subcutaneous tissue until its insertion in the skin that covers the clavicle and shoulder(3,4).
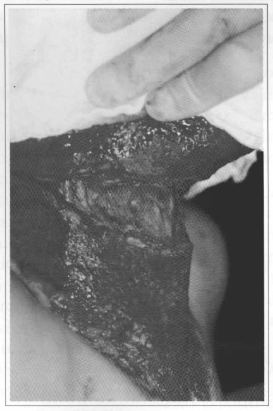
The surgery proposed for the acute phase is based on the histological study conducted after the debridement of burnt cervical skin. The remaining tissue underwent biopsy and the histological examination showed an intense chronic inflammatory process with capillary proliferation, lymphocyte invasion and septal fibrosis, involving fat and the platysma muscle (Fig. 1).

Fig. 1 - Biopsy performed 10 days after the burn and 5 days after debridement of the necrosis. The histological section shows muscle and adipose tissue with intense chronic inflammatory reaction (lymphocytes), capillary proliferation and septal fibrosis.
The surgical intervention in the cervical burns under consideration, with the section of the platysma muscle, would prevent the retraction of the superficial muscular fibrosis affecting the cervicomandibular angle and cervical extension.
MATERIAL AND METHOD
Between 1997 and 2002, 24 patients with deep burns in the cervical region were treated with the same surgical method in the acute phase. Eleven of the biopsies showed incipient fibrosis of the platysma muscle in the histological examination. Ages ranged from 6 to 52 years (average 32 years); 20 patients were female and 4 male; 1 was black, 13 were white and 10 were mixed race. The extension of the burnt areas ranged from 4 to 51% (average 24%). Eighteen of the burns had been caused by fire, and 6, by hot water, with bilateral neck injuries in 100% of the cases.
TREATMENT
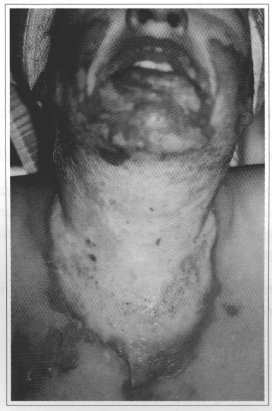
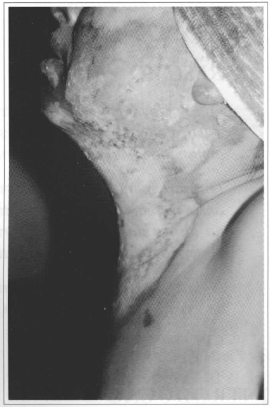
Burns were initially cleaned and treated daily with a 0.9% saline solution and silver sulfadiazine. About 4 to 7 days after the burn, with the delimitation of the necrosis - either through the formation of a dark and dry eschar, or by the fixed reddish or whitish aspect(5)(Figs. 2 and 3) - surgical debridement was performed with patients anesthetized by nasal or orotracheal intubation. The necrosed tissue was tangentially resected with a Blair knife until a viable bleeding bed was found. The surgeon then proceeded with hemostasis with an electric scalpel and/or ligature and pads soaked in a 1:250,000 adrenaline solution. A further operation was then scheduled for 2 to 7 days later, after good hemodynamic and clinical control was achieved, especially in the cases of extensive associated debridements in other regions of the body(6,7,8 and 9) (Figs. 4,5 and 6).
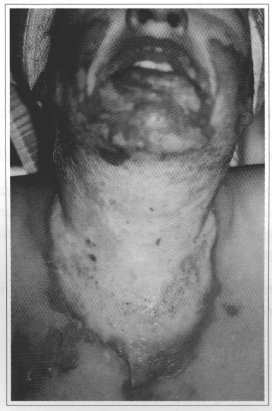
Fig. 2 - Front view 5 days after alcohol burn. Note the delimitation of necrosis with whitish and ischemic skin.
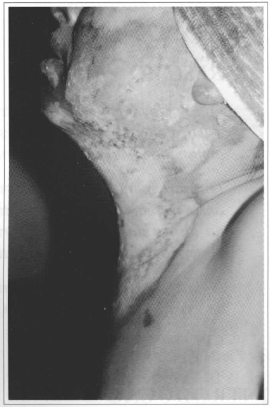
Fig. 3 - Profile view, with necrotic eschar impeding full cervical extension.
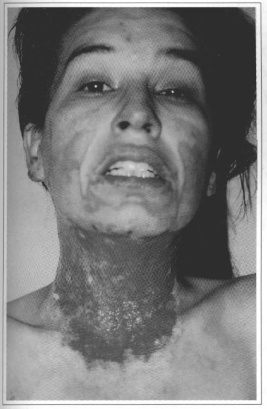
Fig. 4 - Front view 10 days after burn and 5 days after debridement of the necrosed tissue. Note the re-epithelization of the facial skin and the formation of active granulation tissue.
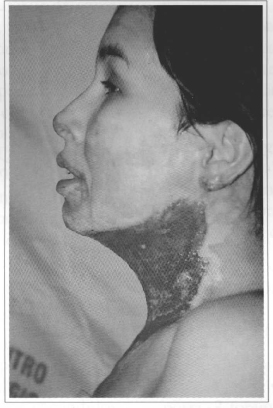
Fig. 5 - Profile vicw, 5 days after debridement of the tissue, with neck in neutral position. Note the poor definition of the cervicomandibular angle.

Fig. 6 - Profile view, 5 days after debridement, with difficult cervical extension.
After accommodating patients in hypercervical extension, the platysma muscle was sectioned, right above the laryngeal prominence, from one condyle to the other in the mandible, limited by the border of the sternocleidomastoid muscle. There was immediate gain in cervical extension. By blunt dissection, traction was exerted on the borders of the newly performed incision, in the cranial and caudal direction with pads; the plane was that of the cervical fascia with little bleeding, except for the branches of the thyroid artery. Approximately 10 to 15 centimeters were gained, the caudal gain being the most interesting, where the platysma muscle surfaces, and which would have greater potential for retraction over the newly grafted skin. The surgeon then continued by trimming or resecting this detached tissue with scissors, so as to level the region (Fig. 7), and the tissue was then sem for histological examination.
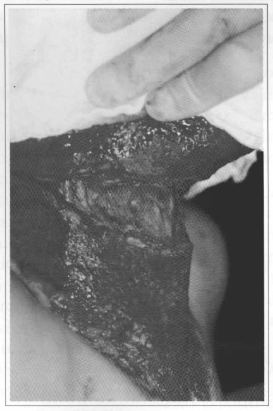
Fig. 7 - Intra-operative profile with incision only in the platysma muscle.
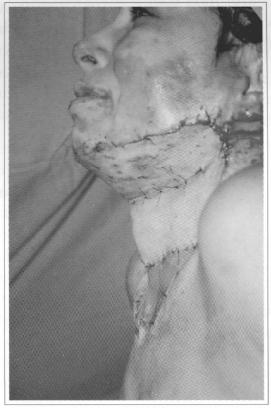
If there was normal skin in one of the thighs, partial skin, thick enough to cover the bloody cervical area, was removed with a Blair knife or dermatome. The skin removed for the graft was randomly punctured so as to prevem major hematomas, and then fixed with 4-0 nylon sutures and with exposure dressings (Fig. 8). The only child that was operated on received a large Brown occlusive dressing.
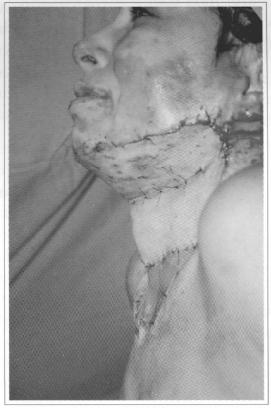
Fig. 8 - Immediate post-operative, patient with exposed graft in hypercervical extension.
Patients were kept in hyperextension on a wedgeshaped cushion (from waist to shoulder), under a Protection Arch, for 7 to 10 days. They were prescribed a light and/or liquid diet for two days. Slow head movements were allowed and the headrest was raised after the third post-operative day.
Neck grafts were examined on a daily basis and occasional hematomas were promptly drained. After about 7 to 10 days, time for the donor site to re-epithelize, the neck being the only lesion, and in the absence of graft losses, patients were discharged with a temporary cervical collar.
Hospitalization times varied from 3 to 15 weeks (average 8.3 weeks). There was one death, and outpatient follow-up varied from 15 days to 4 years.
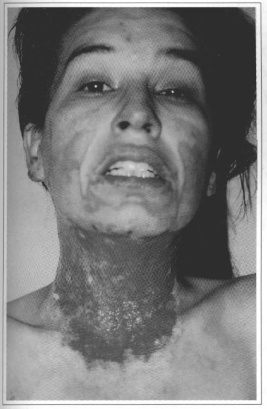
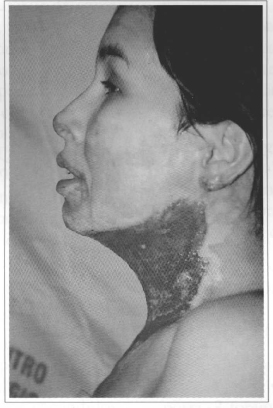
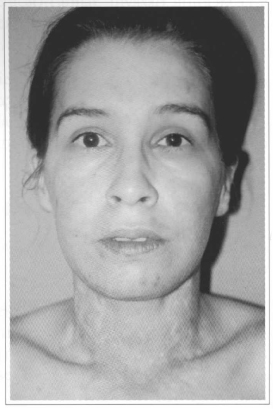
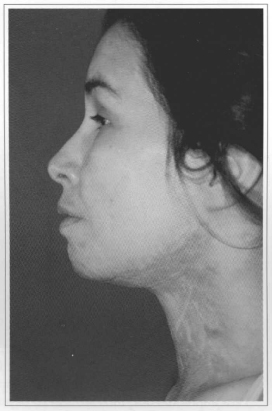
A physician, a physical therapist, an occupational therapist, and, whenever possible, a phoniatrist followed up the patients. The cervical collar was used for a long period (not less than 6 months), longer in proportion to how many cicatricial hypertrophies on the margins of the graft or to how thin the cervical grafts were. In the presence of cicatricial hypertrophic lesions on the face, chin, lateral neck or thorax, masks, chin protectors, compressive elastic mesh and silicone plates were associated (Figs. 9, 10 and 11).
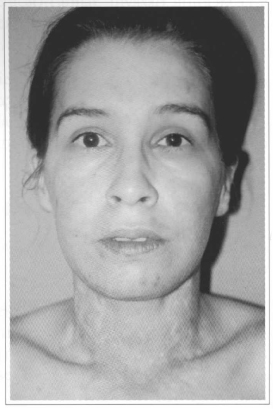
Fig. 9 - Front view 1 year after surgery.
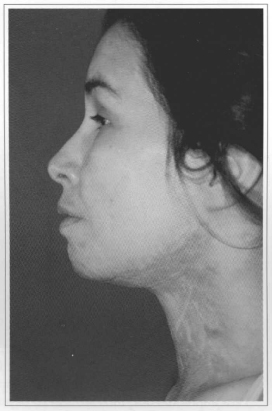
Fig. 10 - Profile in neutral position, 1 year later, with a good cervicomandibular angle.

Fig.11 - Hyperextended profile, 1 year later, without retractions.
RESULTS
All the 24 immediate surgical results were good, with visible gains in the cervical angle, free from intra-operative complications. There was one death on the 12th post-operative day due to clinical complications resulting from the large extension of the burn. There were 5 out of 24 (or 20%) post-operative hematomas that were drained in the bed without any seguelae. There were few cases of graft retraction, as thick skin was used. However, in cases in which the thorax was affected and grafted with expanded skin, there were major retractions (3 out of 23 or 13%), exerting downward traction on the neck. These were the worst results, and two of those cases were re-operated approximately 6 months later due to insufficient cervical extension.
There were 2 cases (8%) of cicatricial hypertrophy on the lateral borders of the cervical graft that were treated with z-plasty, and 2 cases (8%) of small bridles under the graft, which were also treated with z-plasty under local anesthesia. Graft dyschromias were most freguent anlong dark skinned patients, especially hyperchromia, which spontaneously decreased with time or due to the topical use of dermatologic dechroming. As to outpatient follow-up, 19 out of 23 (82%) were followed for 3 months, 15 out of 23 (65 %) for 6 months, 14 out of 23 (60%) for 1 year, 10 out of 23 (43 %) for 2 years, 3 out of 23 (13%) for 3 years, and 1 patient was followed up for 4 years.
DISCUSSION
There are many surgical techniques to correct cicatricial cervical sequelae; some use grafts, others advancements and rotations of flaps (cutaneous, fasciocutaneous, myocutaneous), expanded flaps, free microsurgical flaps, or expanded microsurgical flaps, etc. However, for the acute phase, either due to the extension of the burn, serious ness of the general condition, infections or injuries to adjacent tissues, there are few surgical alternatives.
The verification of the involvement of the platysma muscle in the inflammatory process, favored directly or indirectly by the cervical burn, and its possible resulting fibrosis and retraction, affecting chiefly necks with little subcutaneous tissue, led this author to design this surgical approach. It is worth mentioning that even obese patients or those with a lot of cervical subcutaneous tissue, even when the platysma muscle is not affected, can benefit from a greater definition of the cervicofacial angle, also due to local lipectomy. The biopsies of 11 out of 24 patients showed some lesion to the platysma muscle. No muscular involvement was found in the remaining patients either due to the excess of local adipose tissue or because the tissue that was removed for histological examination was hardly affected.
According to this study, it is not enough to debride and graft the burnt area, especially in necks with little subcutaneous tissue. Results are often poor, even with the prolonged use of a cervical collar (more than 6 months). Early debridement (borne out by extensive references in the literature)( 9-11) helps to remove necrotic tissue, which, along with bacterial proliferation, perpetuates inflammation and the resulting fibrosis. At the same time, after debriding the necrotic cervical tissue, one should not wait toa long for skin grafting, because repairing for healing by local second intention starts with the formation of granulation tissue.
The measure of the surgical gain is performed by "observation and palpation", as there is no previous measure of the angle of cervical mobility. Since we know that this angle depends on the age and biotype of the patient, it is difficult to compare it with other techniques.
A shorter hospital stay is empirical; one would assume that performing the debridement and early skin grafting could also contribute towards earlier discharges.
As to the prevention of seguelae, we found that of the 23 living patients who underwent the proposed surgical technigue, 3 were re-operated due to major retraction of the thoracic mesh graft exerting traction on the neck, 2 underwent z-plasty on the lateral border of the cervical graft and 2 were re-operated with local anesthesia due to small bridles in the center of the graft, perhaps due to adherence of the remaining platysma.
As to outpatient follow-up of burnt patients in public clinics, the main problems were changes in their addresses and the economic difficulty for the follow-up (physician, physical therapist, phoniatrist, psychologist, cosmiatrician, and so on).
Lastly, as to the economic aspect, it is worth mentioning that patients can hardly afford compressive elastic meshes, ortheses, silicone plates, lotions, and sun screen lotions, which are scarcely or not provided by public healthcare services, which makes the already long recovery of burnt patients even more difficult.
CONCLUSION
Considering all that has been mentioned above, this surgical technigue contributes to the treatment of deep cervical burns. It provides better definition of the cervicofacial angle and greater neck extension on the first hospitalization, thus preventing future admissions to treat cervical retractile seguelae. It is, therefore, less costly to healthcare services and reintegrates patients into society more rapidly.
Due to its simplicity, this procedure can be performed in any burns treatment clinic, and it does not reguire technological sophistication.
ACKNOWLEDGEMENTS
The author would like to pay special thanks to the patients who trusted his skills, fellow Plastic Surgery Residem Physicians (Santa Casa de São Paulo, UNIFESP, Hospital Santa Cruz, residents of Dr. Paulo Mateó's clinic and of the Hospital do Servidor Público Estadual) who were interns and helped him during these years in the burn clinics where this study was conducted.
REFERENCES
1. Kapandji IA. Fisiologia Articular. São Paulo: Manole; 1990. p.44-5.
2. Farid MM, Abdalla BM, Abdel FM. Burn contractures of the neck. Plast Reconstr Surg. 1978; 62:66-73.
3. Zani R, Melo JRA. Anatomia Cirúrgica da Face. In: Cirurgia Plástica. Ed. Ateneu; 1996.
4. Weston D, Gardner MD, Willian A, Osburn MMA. Anatomia Humana. 3ªed. São Paulo: Atheneu; 1974. p. 137.
5. Weston D, Gardner MD, Costa B, Nakamura DY, More ML, Blayney CB, Hoover CL. Early excision and grafting of face and neck burns in over 20 years. Plast Reconstr Surg. 2002; 109(4): 1266- 73,.
6. Jonsson CE, Dalsgaard CJ. Early excision and skin grafting of selected of the face and neck. Plast Reconstr Surg. 1991; 88(1) :83-92.
7. Voinchet V, Bardot J, Echinard C, Aubertjp, Magalon G. Advantages of early burn excision and grafting in the treatment of burn injures of anterior cervical region. 1995 21(2):143-6.
8. Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J. Trauma. 1970; 10:1103.
9. Iwuagwu FC, Wilson D, Bailie F. The use of skin grafts in postburn contracture rease: a 10-year review. Plast Reconstr Surg. 1999; 103(4):1198- 204.
10. Cole JK, Engrav LH, Heimbach DM, Gibran NS, Costa BA, Nakamura DY, Moore ML, Blayney CB, Hoover CL. Early excision and grafting of face and neck burns in parients over 20 years. 2002; 109(4): 1266-73.
11. Heimbach DM. Early burn excision and grafting.Surg Clin North Am. 1987; 67:93.
I - Member of the Brazilian Plastic Surgery Society Attending Physician in the Burns Clinic of the Hospital Municipal Dr. Carmino Caricchio and in the Hospital do Servidor Público Estadual de São Paulo.
This study was conducted in the Hospital Municipal do Tatuapé and in the Hospital do Servidor Público do Estado de São Paulo.
Address for correspondence:
Roberto Cammarota Jr., MD
Av.Paulista, 2644 Cj.63
01310-300 - São Paulo - SP Brazil
Phone: (55 11) 3259-4797 - Fax: (55 11) 3231-5584
e-mail: bobcjunior@uol.com.br
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license