

Original Article - Year 2016 - Volume 31 -
Mastoplasty with inclusion of prosthesis during abdominoplasty in post-bariatric patients
Mastoplastia com inclusão de prótese via abdominoplastia em pacientes pós-bariátricos
ABSTRACT
INTRODUCTION: Augmentation mammaplasty during abdominoplasty reduces surgical time and has a better aesthetic effect as it only leaves a single scar. The authors of this study assessed the results obtained in post-bariatric patients undergoing this procedure in the plastic surgery service at Daher Hospital.
METHODS: This was a retrospective longitudinal observational study. Of the 161 post-bariatric patients evaluated, 27 had indications for breast augmentation during abdominoplasty. The surgical technique consisted of classical abdominoplasty and creation of tunnels on the upper and middle abdomen for insertion of implants.
RESULTS: The age of the patients ranged from 35 to 50 years, with a mean of 42.4 years. The volume of the prosthesis ranged from 285 to 300 ml. The average body mass index was 22.2 kg/m2.The average surgical time period was 2 hours and 35 minutes. None of the following complications were observed: deep vein thrombosis, pulmonary embolism, skin necrosis, hematoma, capsular contracture and/or event. Two patients (7.4%) presented with seroma in the mammary region and one patient developed infection.
CONCLUSION: The aesthetic results were satisfactory, as there was only a single scar for these two procedures in post-bariatric patients. Selecting the ideal patient was crucial for good operative success.
Keywords: Mammaplasty; Breast implantation; Abdominoplasty; Bariatric surgery.
RESUMO
INTRODUÇÃO: A mastoplastia com inclusão de prótese via abdominoplastia proporciona redução do tempo cirúrgico e um melhor efeito estético, em decorrência da presença de uma única cicatriz. Os autores desse estudo avaliaram os resultados obtidos em pacientes pós-bariátricos submetidos à inserção de prótese mamária pela via abdominal no serviço de cirurgia plástica do Hospital Daher.
MÉTODOS: Trata-se de um estudo observacional longitudinal retrospectivo. Dos 161 pacientes pós-bariátricos operados, 27 apresentavam indicação de mamoplastia de aumento pela via abdominal. A técnica cirúrgica consistiu na realização da abdominoplastia clássica e confecção de túneis ao espaço retroglandular para inserção dos implantes.
RESULTADOS: A faixa etária das pacientes variou de 35 a 50 anos, com média de 42,4 anos. O volume das próteses variou de 285 a 300 ml. A média do índice de massa corporal foi de 22,2 kg/m2. O tempo médio operatório foi de 2 horas e 35 minutos. Não foram observadas complicações como trombose venosa profunda, embolia pulmonar, necrose de pele, hematoma, contratura capsular e/ou deiscências. Duas pacientes (7,4%) apresentaram seroma na região mamária sendo que uma paciente teve infecção.
CONCLUSÃO: Os resultados estéticos obtidos com a confecção de uma única cicatriz para esses dois procedimentos em pacientes pós-bariátricos foram satisfatórios. A escolha do paciente ideal foi fundamental para o bom sucesso operatório.
Palavras-chave: Mastoplastia; Implante mamário; Abdominoplastia; Cirurgia bariátrica.
Obesity is one of the major public health problems in Brazil, and in other countries. It is an endemic disease with a worldwide incidence. It is estimated that 5% of the population of western countries are obese1.
Gastroplasty aims to provide a better quality of life and a reduction of risk factors for obese patients; however, the weight loss generated by this surgical procedure is associated with a variety of corporal changes2.
The abdomen is an important aesthetic and functional segment of the body. Abdominoplasty together with plication of the rectus abdominis muscle improves the appearance of the abdomen in post-bariatric patients3.
Breast asymmetries or ptosis are evident in most patients undergoing gastroplasty. The indication for the most appropriate surgical procedure for correction depends on several factors4.
Abdominoplasty associated with breast augmentation procedures is frequently performed within plastic surgery departments. The insertion of silicone implants using an abdominal approach reduces surgical time and leaves only a single scar5.
OBJECTIVE
This study aims to present the results in post-bariatric patients undergoing mastoplasty with prosthesis insertion during abdominoplasty surgery in the plastic surgery service of Daher Hospital, Brasília, DF.
METHODS
This was a retrospective longitudinal study developed in the plastic surgery service at Daher from March 2012 to March 2015.
The research project followed the legal procedures established by Resolution 196/96 of the National Health Council regarding research involving human subjects.
The sampling was intentional and based on post-bariatric patients undergoing surgery at our institution. Of the 161 patients undergoing surgery during the study period, 27 patients underwent mastoplasty with insertion of a prosthesis using abdominoplasty.
The variables were age, duration of surgery, postoperative surgical complications, symmetry of the breasts after breast implant insertion, weight of the abdominal insert, length of hospital stay, and type, shape, and volume of the prosthesis.
The criteria used in this study for surgery were:
1. Female patients;Exclusion criteria were:
2. Post-bariatric patients who maintained a stable weight for a minimum period of 6 months with a body mass index (BMI) between 18.5 and 29.9 kg/m2;
3. Patients who wished to undergo abdominoplasty and breast augmentation at the same time, and who had surgical indication for the procedure;
4. Patients with hypomastia, absence of breast ptosis (or those with breast ptosis grade I according to the Regnault6 classification and absence of pseudoptose) and absence of mammary asymmetry or slight asymmetry;
5. Patients with excess skin and fat in the abdomen with surgical indication for classic abdominoplasty;
6. Patients with an American Society of Anesthesiology (ASA) fitness score of 1 or 2.
1. Weight stability for a shorter period than 6 months and/or BMI >29.9 kg/m2;Surgical technique
2. Graduate breast ptosis that was not second grade I Regnault6;
3. Significant breast asymmetry;
4. ASA score > 3.
The surgeries were performed in the operating room under general anesthesia. Markings were made with the patients standing, sitting, and prone. The infiltration was performed either in the abdomen or in the breast at a concentration of 1: 1,000,000 and 1: 300,000, respectively.
A transverse incision was made above the pubic bone, with detachment of the retail up to the xiphoid, and laterally across the ribs to the inframammary crease. A tunnel was then created towards to the retroglandular space as preparation for insertion of the breast implant. The size of the hole was variable depending on the desired size and position of the breasts. Preoperative measurements were taken using prosthetic molds to determine this.
The breast implants were all the same model, and had a polyurethane surface with cohesive silicone gel, round shape, size, and a high profile that varied according to the wishes of the patient. In patients who presented with ptosis, the detachment of the breast crease was performed in a lower position. After preparing the prosthesis site, hemostasis was carefully assessed, the prosthesis was inserted and the tunnels were closed.
Statistical analysis
The results were analyzed in Epi Info program, version 3.5.1. A descriptive analysis of the data was performed.
RESULTS
Of the 161 post bariatric patients who underwent surgery during the study period, 27 (16.7%) had breast implants inserted during abdominoplasty surgery.
The age of patients ranged from 35-50 years with a mean of 42.4 years.
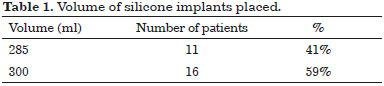
The volume ranged from 285 to 300 ml, and in 11 patients (41%) was added 285 ml and in 16 patients (59%), 300 ml (Table 1).
The average time of surgery was 2 hours and 35 minutes. The hospital stay was 24 hours for all patients.
The weight of the abdominal retail was ranged from 2000 g to 5000 g, with an average of 4248.4 g.
The mean BMI of the patients was 22.2 kg/m2.
The immediate postoperative results were satisfactory regarding the positioning and symmetry of the breasts.
Only one patient had a scar in the breast region (submammary) due to local postoperative infection observed.
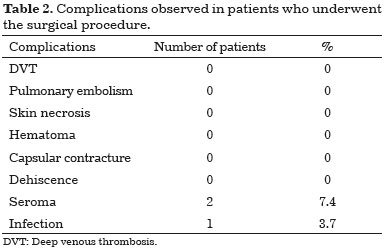
There were no complications such as deep vein thrombosis (DVT), pulmonary embolism, skin necrosis, hematoma, capsular contracture and/or dehiscence.
Of the 27 patients who underwent surgery, two (7.4%) had seroma (Table 2) in the breast region. Of these, 1 case improved with massage and drainage of seroma towards the abdomen. The other case developed an infection, requiring the removal of the prosthesis by submammary incision, washing, and antibiotics to achieve complete regression of the infection. The prosthesis was replaced after 1 year.
During the postoperative follow-up, it was confirmed that the patients were satisfied with the final results. Figures 1 to 5 illustrate some sample cases in this study.

Figure 1. Preoperative markings.

Figure 2. Construction of tunnels and insertion of silicone molds.

Figure 3. Final appearance with breast symmetry.
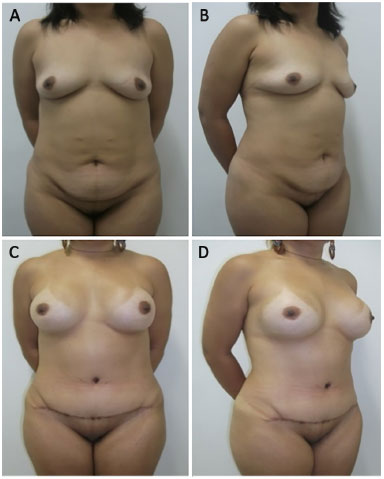
Figure 4. 43 year-old patient. A and B: preoperative view; C and D: 1 year postoperative follow-up. 300 ml breast implants.
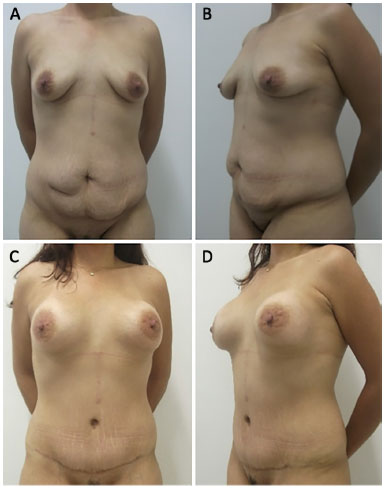
Figure 5. 40 year-old patient. A and B: preoperative view; C and D: 2 year postoperative follow-up. 285 ml breast implants.
DISCUSSION
Patients with indication for abdominoplasty often wish to undergo breast augmentation. Breast implant insertion using the same incision as abdominal surgery is a technique that aims to reduce surgical time and leave only one scar7,8.
This is a procedure based on principles known in the medical literature. Planas was the first author to describe it, between 1972 and 1976, and used a sample of 12 patients and achieved satisfactory results9.
The identification of the ideal patient, especially among post-bariatric patients, is fundamental to a good surgical outcome. Patient without ptosis or first degree breast ptosis benefit from augmentation mastoplasty via abdominoplasty; however, patients with ptosis of second or third degree achieve better results with mastopexy.
The study population consisted of young women with a mean age of 42.4 years and an average BMI of 22.2 kg/m2, similar data to those reported by Sodré et al8.
Surgical time is a principle that should be considered in all patients undergoing surgical procedures. Almeida and Almeida10 showed a variation of 95-210 minutes operative time in patients undergoing classic abdominoplasty.
Regarding the time of surgery in our study, the average was 2 hours and 35 minutes. We emphasize that, associated with abdominoplasty, we held the augmentation mastoplasty corroborating the argument of reducing the operative time in performing this surgical procedure.
For making the retroglandular stores for this type of surgery, the use of molds in tunnels favors local hemostatic compression (in which the surgeon removes the tunnel and prepares the contralateral store) and breast symmetrization11.
The authors of this study found that the previous use of molds in the manufacture of shops allowed the ideal symmetry to be obtained in the cases studied.
Jatene et al.12 published a review of 424 abdominoplasties associated with other surgeries, focusing on the occurrence of complications. Among its results, 8% of patients developed seroma, 1.6% experienced hematoma, 0.7% developed suture dehiscence, 0.4% had necrosis for retail, and 0.7% developed DVT.
In a study by Wallach which consisted of the introduction of breast implants using abdominoplasty surgery, there was a 9% incidence of seroma and wound infection13.
In a study by Paoliello7, the main complications were seroma (58%) and capsular contracture (42%).
In a study conducted by Dini et al.11 no drain was used in patients undergoing insertion of breast implants and a tummy tuck achieved low rates of postoperative complications. The author believes that there is need to use drains in the breasts when performing this type of procedure, since whole blood or plasma drains through the tunnels.
In our study, all patients undergoing augmentation mastoplasty during abdominoplasty did not receive surgical drains. Seroma formation was observed in two cases, one in the breasts, and one in which there was regression with massage towards the abdomen. The other case evolved as a result of infection in the store, requiring local drainage with resection of the prosthesis by submammary incision, washing, and antibiotic administration. Replacement of the prosthesis was performed after 1 year and it did not change the patient's satisfaction with the surgery.
No cases of dehiscence, hematoma, skin necrosis, or DVT was observed in our study.
The authors of this study did not perform liposuction of the abdomen wall during the tummy tuck. We observed that this favored the reduction of surgical time and had no effect on seroma formation in the abdominal region. We believe that vigorous hemostasis associated with careful surgical technique were key factors in preventing this complication.
The literature review shows a lack of studies that shed light on the use of this procedure in post-bariatric patients. The development of targeted surgical techniques for these patients is of paramount importance, given that the number of patients undergoing gastroplasty has increased significantly14.
Finally, the results obtained in this study were considered satisfactory, according to the patients at the postoperative follow-up. We stress the importance of considering the criteria for inclusion of patients for this procedure. Selection of the ideal patient is critical for surgical success.
CONCLUSION
The insertion of breast prostheses during abdominoplasty in post-bariatric patients provides satisfactory results with reduced of the redundancy distributed asymmetrically in the breast and abdomen, reduced surgical time compared with the conventional technique, and production of a single scar providing a good aesthetic effect.
The correct identification of patients is of fundamental importance to the success of plastic surgery.
COLLABORATIONS
JNRN Performance of operations and/or experiments.
DASS Conception and design of the study.
MCC Drafting the manuscript or critical review of content.
LMCD Conception and design of the study.
RQL Conception and design of the study.
CMA Conception and design of the study.
IRJ Conception and design of the study.
JCD Final approval of the manuscript.
REFERENCES
1. Moreno Esteban B, Zugasti Murillo A. Bariatric surgery: an update. Rev Med Univ Navarra. 2004;48(2):66-71.
2. Ribeiro L. Pedículos em mamoplastia: atlas e texto. Rio de Janeiro: Guanabara Koogan; 2005.
3. Dini GM, Ferreira LM. Putting the umbilicus in the midline. Plast Reconstr Surg. 2007;119(6):1971-3.
4. Castro CC, Aboudib JH, Coelho RFS, Gatorno M. Conceituação sobre as mamoplastias e mastopexias. Rev Bras Cir Plást. 2002;17(3):11-26.
5. Rinker B, Jack JM. Subpectoral breast augmentation through the abdominoplasty incision. Ann Plast Surg. 2007;58(3):241-5.
6. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
7. Paoliello HR Jr. Inclusão mamária por via abdominal. In: Stocchero IN, Tournieux AAB, eds. Atualização em cirurgia plástica estética e reconstrutiva. São Paulo: Robe; 2006. p.703-6.
8. Sodré RL, Calil JA, Fonseca JMM, Oyagawa MY, Secco LG, Ogata DY, et al. Mastoplastia de aumento através da abdominoplastia. Rev Bras Cir Plást. 2012;27(3):435-40.
9. Planas J. Introduction of breast implants through the abdominal route. Plast Reconstr Surg. 1976;57(4):434-7.
10. Almeida EG, Almeida Júnior GL. Abdominoplastia: estudo retrospectivo. Rev Bras Cir Plást. 2008;23(1):1-10.
11. Dini GM, Milani J, Albuquerque LG, Oliveira MF, Santos Filho IDAO, Iurk LK, et al. Aumento mamário por meio da incisão da abdominoplastia: estudo prospectivo de 100 casos. Rev Bras Cir Plást. 2013;28(1):105-13.
12. Jatene PRS, Jatene MCV, Barbosa ALM. Abdominoplastia: experiência clínica, complicações e revisão da literatura. Rev Bras Cir Plást. 2005;20(2):65-71.
13. Wallach SG. Transabdominal breast augmentation. Aesthet Surg J. 2004;24(4):373-8.
14. Meira AAM, Andrade IF, Ferreira FPM. Cirurgia plástica após gastroplastia redutora: abordagem pré, per e pós-operatória. Rev Bras Cir Plást. 2008;23(1):15-21.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Daher Lago Sul, Brasília, DF, Brazil
Institution: Hospital Daher Lago Sul, Brasília, DF, Brazil.
Corresponding author:
Daniel Augusto dos Santos Soares
CCSW 02 lote 03, Ed. Unique Duplex Apto 105 - Sudoeste
Brasília, DF, Brazil Zip Code 70680-250
E-mail: daniel.soares@globo.com
Article received: November 20, 2015.
Article accepted: August 6, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter