

Case Reports - Year 2016 - Volume 31 -
Galactocele due to drugs prescribed after augmentation mammoplasty: a case report and literature review
Galactocele medicamentosa pós-mamoplastia de aumento: relato de caso e revisão da literatura
ABSTRACT
Augmentation mammaplasty is a common and safe plastic surgery procedure, but it is not free from complications. Galactocele after augmentation mammaplasty is rarely described in the literature. We discuss the case of a 34-year-old woman who had been taking sulpiride for 2 years and 4 months and developed galactocele approximately 100 days after augmentation mammaplasty. However, diagnosis should be suspected if breast size increases and it is associated with postoperative local heat, pain or breast discomfort. We believe that the surgeon must surgically drain galactocele to confirm diagnosis, especially to exclude the presence of breast abscess.
Keywords: Breast diseases; Breat cyst; Mammaplasty; Sulpiride.
RESUMO
A mamoplastia de aumento é um procedimento cirúrgico muito comum e seguro na cirurgia plástica, mas o mesmo não está isento de complicações. A galactocele após mamoplastia de aumento é raramente descrita na literatura. Este relato de caso refere-se a uma paciente de 34 anos de idade, que fazia uso de sulpirida há 2 anos e 4 meses e desenvolveu galactocele cerca de 100 dias após mamoplastia de aumento. O diagnóstico deve ser suspeitado quando se observar uma mama aumentada de volume, associada a calor local, dor ou desconforto mamário no pós-operatório. Acredita-se que a melhor conduta seja a drenagem cirúrgica, a fim de confirmar o diagnóstico de galactocele e excluir a presença de abscesso mamário.
Palavras-chave: Doenças mamárias; Cisto mamário; Mamoplastia; Sulpirida.
Augmentation mammoplasty is a common and safe surgical procedure in plastic surgery; nevertheless, it is not free of complications. Some of these complications are well known, such as seromas, hematomas, and abscesses, but others are less commonly encountered by surgeons, such as galactocele after augmentation mammoplasty. In 1972, Golden and Wangensteen defined galactocele as a rare cyst in lactating breasts1.
Lactation and galactocele formation after augmentation mammoplasty are scarcely reported in the literature2. In 1971, Hartley and Schatten3 were the first authors to report the breast augmentation and lactation after augmentation mammoplasty. Owing to its rarity, the incidence of galactocele after augmentation mammoplasty has not yet been clarified.
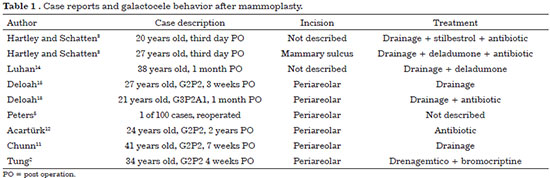
In 1994, Caputy and Flowers4 found 8 cases of galactorrhea in 1000 cases of augmentation mammoplasties. Meanwhile, Peters et al.5 found a unique galactocele case after reoperating 100 cases of augmentation mammoplasty that were directed to them because of complications. The most recent case of galactocele associated with this surgical aesthetic procedure was reported in 20112. After a literature review, it was described as the 10th case of galactocele that occurred after surgery for augmentation mammoplasty for inclusion of a prosthesis (Table 1).
Reports of galactocele cases after reduction mammoplasty are few6,7, and only one case of galactorrhea after mastopexy with placement of a prosthesis was reported8, in addition to two other galactocele cases after mammary injection of a polyacrylamide hydrogel9,10.
The present report describes a case of a 34-year-old woman who had been using sulpiride for 2 years 4 months and who developed galactocele nearly 100 days after undergoing augmentation mammoplasty.
CASE REPORT
A 34-year-old woman, gravida 2 para 2, who was previously healthy (Figure 1), underwent bilateral augmentation mammoplasty with inclusion of a 350-cc, textured, round, high-profile Mentor prosthesis by using the infra-areolar and trans-mammary approaches, positioned at the subglandular plane. During the procedure, rhinoplasty and submental and anterior axillary region lipoaspiration were performed. The surgery was performed without complications, and the patient was discharged on the same day.

Figure 1. Preoperative image, prior to augmentation mammoplasty.
Analgesic medication and antibiotic were prescribed for 7 days. Revisions were performed in the first and second weeks after the surgery and the first month after surgery. The patient was satisfied with the results until that moment and did not have complaints regarding the mammary volume.
After 100 days, the patient sought for a new service because of concern of mammary asymmetry, as she observed that her left breast was smaller than her right breast. The patient did not present systemic symptoms. When tested, the breasts presented with a large volume, considerably larger than that of the right breast, by palpation of the left prosthesis. Inflammation was not observed in any of the breasts (Figure 2).

Figure 2. Postoperative image, after augmentation mammoplasty. Breast asymmetry in galactocele.
Laboratory tests were requested, and no alterations were observed. Bilateral breast ultrasonography revealed discontinuity of the left breast prosthesis, with a possible rupture. The patient had a history of using contraceptive and antidepressant (sulpiride) medications prescribed by a gynecologist. She started the use of sulpiride 2 years 4 months before. Eventually, she presented bilateral galactorrhea, a symptom collateral to the medication used. After inclusion of the breast prosthesis, the patient no longer presented this symptom.
Six days after the ultrasonographic examination, the patient underwent a new surgical procedure for replacement of the left breast prosthesis, which was supposed to be ruptured, and of the right breast prosthesis, because of its smaller volume (bilateral 275 cc) than that of the left breast, as she was not satisfied with the large volume of her breasts. The surgery was initiated through the right breast (greater volume) by approaching the same infra-areolar scar. When the implant capsule was opened, a large amount of milk secretion was found, which did not seem to be a purulent collection. In the left breast, the same milk secretion was present but in a lesser amount, and the breast prosthesis was intact (Figure 3).

Figure 3. Transoperative image. Reintervention surgery for drainage of galactocele.
The implants were removed, the cavities were thoroughly washed with saline solution, and subsequently restored. In accordance with the previous decision made with the consent of the patient, a reduction of the diameter of the nipple-areolar complex was performed. The secretion was submitted to culture testing, and microorganism growth was not observed. The sulpiride medication was suspended, and a 2.5-mg bromocriptine treatment was initiated 2 times/day for 7 days to suspend the hormonal production stimulation.
The patient made one last follow-up visit with the physician nearly 60 days after the last procedure. Upon completion of the bromocriptine treatment, the symptoms of lactation disappeared, and she was satisfied with the result (Figure 4).
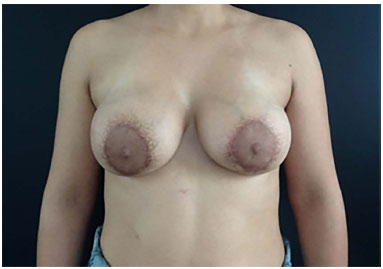
Figure 4. Postoperative image. Final result after drainage of galactocele.
DISCUSSION
In our study on lactation, we observed that the production and expression of milk occur because of the interaction of several hormones. Lactation seems to occur owing to the increase in prolactin levels during the decline in the estrogen and progesterone levels8. Meanwhile, oxytocin regulates milk ejection and is stimulated by the suction reflex2. In contrast, the neuromodulator dopamine acts by inhibiting prolactin secretion via neurohypophysis.
Understanding this physiopathology is required in order to elucidate how sulpiride and other dopamine inhibitors that interact in this hormonal cycle stimulate milk production and contribute to galactocele formation. By contrast, dopamine agonistic factors such as bromocriptine also inhibit prolactin and, consequently, lactation; therefore, they are essential in the treatment of galactocele.
Harper et al.18 recommended that prompt fluid drainage and hormonal therapy concomitant with dopaminergic agonists should be initiated immediately after the diagnosis of galactocele. Meanwhile, Chun and Taghinia11 recommended clinical management with bromocriptine alone if the diagnosis is clearly galactocele.
The bromocriptine dosage should be titrated according to its effect; but unfortunately, no consensus has been reached as to the duration of the therapy2. In the present case, as well as in that reported by Tung and Carr, a dosage of 2.5 mg 2 times/day for 7 days was used2. In both cases, success was achieved and the patients did not report collateral effects. Further studies are required, but we believe that this dosage may be safe to use for similar cases.
Galactocele can be clinically suspected, but a surgical intervention is generally required to drain the fluid collection and confirm the diagnosis11. The main symptom of galactocele is the increase in breast volume, as in the described case, but the disorder may also manifest through pain2,11,12, hyperemia8,12, discomfort2,12, or burning sensation13. On physical examination, breast asymmetry is observed, if unilateral, in addition to tension during palpation of the affected breast.
Ultrasonography is initially a good imaging modality for the study of consistency of lesions9. In the present case, the radiologist identified a discontinuity of the breast prosthesis and suggested rupture of the prosthesis as diagnosis. On the other hand, Chun and Taghinia11 observed a well-organized fluid collection of 8 cm in diameter, which suggested an abscess. Meanwhile, Tung and Carr2 observed on ultrasonography the presence of a complex collection around the prosthesis, which is not typical of seroma.
In 2001, Sawhney et al.17 studied the ultrasonographic appearance of 10 galactocele cases that were previously described and defined in greater detail and the ecographic appearance of these lesions. These were usually echogenic solitary lesions with good delimitation, thin walls, and some degree of posterior reinforcement. The appearance of its internal content varied from homogeneous to heterogeneous, with anechoic clefts and rimes internally.
Galactocele may present an appearance very similar to a cyst, as described earlier, as its milky content is contained within a thin wall, and should not be mistaken with prosthetic rupture, where wall discontinuity with leakage of liquid is assumed.
In regard to the surgical technique, as depicted in Table 1, most of the patients with galactocele underwent prosthetic implantation through a periareolar incision. Therefore, this fact may be more than pure chance. Nevertheless, the possible association remains controversial. Chun and Taghinia11 stated that the approach through the periareolar incision could lead to the obstruction of ducts and contribute to galactocele formation.
Consensus has not been reached as to the possibility of an association between the subglandular or submuscular dissection plane and galactocele formation2. According to Tung and Carr2, theoretically, a truly submuscular dissection plane through a non-periareolar incision would be as invasive as the manipulation of the mammary gland. Moreover, the manipulation of mammary tissue (with incisions made through the ductal tissue) may have likely caused or worsened the galactocele formation12.
Rothkopf and Rosen8 reported that lactation after augmentation mammoplasty was successfully treated with bromocriptine. According to the literature, other treatments include intercostal blockade, isolated surgical drainage, and possible expectant approaches. Golden and Wangensteen1 stated that simple excision of the galactocele effectively cured all the series reported.
Nevertheless, in the case reported by Vassilikos16, the patient was just observed and reevaluated, and after 2 weeks, the lactation ceased spontaneously. Finally, when galactocele is suspected, the lesion should be drained surgically to confirm the diagnosis and to prevent abscess formation and the consequent need for antibiotic therapy.
Rothkopf and Rosen8 stated that the presence of subcutaneous milk exposes the prosthesis to possible infections. The need for pharmacological treatment with bromocriptine or other dopamine agonists is controversial, but these medications are used owing to their possible benefits and absence of significant adverse effects.
CONCLUSION
Finally, when galactocele is suspected, the lesion should be drained surgically to confirm the diagnosis and to prevent abscess formation and the consequent need for antibiotic therapy. Rothkopf and Rosen stated that the presence of subcutaneous milk exposes the prosthesis to possible infections8. The need for pharmacological treatment with bromocriptine or other dopamine agonists is controversial, but these medications are used owing to their possible benefits and absence of significant adverse effects.
COLLABORATIONS
MSSV Surgeon responsible and supervisor.
PSV Literature review and writing of the manuscript.
CB Literature review and writing of the manuscript.
REFERENCES
1. Golden GT, Wangensteen SL. Galactocele of the breast. Am J Surg. 1972;123(3):271-3. PMID: 5011932 DOI: http://dx.doi.org/10.1016/0002-9610(72)90283-8
2. Tung A, Carr N. Postaugmentation galactocele: a case report and review of literature. Ann Plast Surg. 2011;67(6):668-70.
3. Hartley JH Jr, Schatten WE. Postoperative complication of lactation after augmentation mammaplasty. Plast Reconstr Surg. 1971;47(2):150-3. PMID: 5107582
4. Caputy GG, Flowers RS. Copious lactation following augmentation mammaplasty: an uncommon but not rare condition. Aesthetic Plast Surg. 1994;18(4):393-7. PMID: 7817889
5. Peters W, Smith D, Fornasier V, Lugowski S, Ibanez D. An outcome analysis of 100 women after explantation of silicone gel breast implants. Ann Plast Surg. 1997;39(1):9-19. PMID: 9229086
6. Arnon O, Mendes D, Winkler E, Tamir J, Orenstein A, Haik J. Galactorrhea complicating wound healing following reduction mammaplasty. Aesthet Surg J. 2006;26(3):300-1. PMID: 19338911
7. Majdak-Paredes EJ, Shafighi M, During V, Sterne GD. An unusual case of galactorrhea in a postmenopausal woman complicating breast reduction. J Plast Reconstr Aesthet Surg. 2009;62(4):542-6.
8. Rothkopf DM, Rosen HM. Lactation as a complication of aesthetic breast surgery successfully treated with bromocriptine. Br J Plast Surg. 1990;43(3):373-5
9. Lin WC, Hsu GC, Hsu YC, Hsu HH, Li CS, Chen TY, et al. A late complication of augmentation mammoplasty by polyacrylamide hydrogel injection: ultrasound and magnetic resonance imaging findings of huge galactocele formation in a puerperal woman with pathological correlation. Breast J. 2008;14(6):584-7.
10. Kang GC, Ong YS. Large unilateral breast autoinflation after breastfeeding linked to polyacrylamide hydrogel injection augmentation mammaplasty. Aesthetic Plast Surg. 2011;35(1):122-4.
11. Chun YS, Taghinia A. Hyperprolactinemia and galactocele formation after augmentation mammoplasty. Ann Plast Surg. 2009;62(2):122-3. PMID: 19158518
12. Acartürk S, Gencel E, Tuncer I. An uncommon complication of secondary augmentation mammoplasty: bilaterally massive engorgement of breasts after pregnancy attributable to postinfection and blockage of mammary ducts. Aesthetic Plast Surg. 2005;29(4):274-9.
13. Bentley M, Ghali S, Asplund OA. Galactorrhoea causing severe skin breakdown and nipple necrosis following breast reduction. Br J Plast Surg. 2004;57(7):682-4. PMID: 15380704
14. Luhan JE. Giant galactoceles 1 month after bilateral augmentation mammoplasty, abdominoplasty, and tubal ligation: Case report. Aesthetic Plast Surg. 1979;3(1):161-4. PMID: 24173987
15. Deloach ED, Lord SA, Ruf LE. Unilateral galactocele following augmentation mammoplasty. Ann Plast Surg. 1994;33(1):68-71. PMID: 7944201
16. Vassilikos C. Lactation: a rare, late complication of augmentation mammaplasty. Aesthet Surg J. 2004;24(5):449-50.
17. Sawhney S, Petkovska L, Ramadan S, Al-Muhtaseb S, Jain R, Sheikh M. Sonographic appearances of galactoceles. J Clin Ultrasound. 2002;30(1):18-22.
18. Harper JG, Daniel JR, McLean JN, Nahai F. Postaugmentation galactocele. Plast Reconstr Surg. 2013;131(5):862e-3e. PMID: 23629139
1. Hospital de Clinicas de Porto Alegre, Porto Alegre, RS, Brazil
2. Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, RS, Brazil
3. Universidade Federal de Santa Maria, Santa Maria, RS, Brazil
4. Hospital Universitário, Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil
Institution: Universidade Federal de Santa Maria, Santa Maria, RS, Brazil.
Corresponding author:
Mauricio Schneider Salomone Viaro
Rua José Paulo Teixeira, 271 - Camobi
Santa Maria, RS, Brazil Zip Code 97110-750
E-mail: msviaro@hotmail.com
Article received: January 20, 2014.
Article accepted: January 22, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter