

Ideas and Innovation - Year 2016 - Volume 31 - Issue 2
Tensioned reverse abdominoplasty for reconstruction of large post-mastectomy defects
Abdominoplastia reversa tensionada para reconstrução de defeito estendido após mastectomia
ABSTRACT
Reconstructive options for anterior chest wall defects can be challenging especially when the defect is large and has been subject for preoperative radiotherapy. We report a case of a patient with a neglected large invasive ductal carcinoma of the breast who had received incomplete preoperative radiotherapy and chemotherapy. The pathology examination revealed an 11.5 cm invasive ductal carcinoma, grade III, with lymphovascular invasion and positive axillary lymph nodes (20/20). The post mastectomy large defect following wide skin excision measured 25 x 20 cm and it was immediately covered with a tensioned reverse abdominoplasty flap. To our knowledge, this is the first case reported of a wide skin excision mastectomy reconstructed solely with a reverse abdominoplasty advancement flap and progressive high-tension with quilting sutures demonstrating that, in the selected patients, abdominal skin can be safely and easily advanced superiorly to reach the upper chest area and cover an area of significant defect.
Keywords: Abdominoplasty; Carcinoma ductal; Mastectomy; Thoracic wall; Surgical flaps.
RESUMO
As opções reconstrutivas para defeitos da parede anterior do tórax podem ser desafiadoras especialmente quando o defeito é extenso e sujeito a radioterapia pré-operatória. Apresenta-se caso de paciente com carcinoma ductal invasivo de mama não tratado que realizou radioterapia e quimioterapia incompleta no pré-operatória. O exame patológico revelou carcinoma ductal invasivo de 11,5 cm, grau III, com invasão linfovascular e linfonodos axilares positivos (20/20). Após a mastectomia, defeitos estendidos seguido de longa excisão de pele mediram 25 x 20 cm, sendo esses cobertos imediatamente com retalhos em abdominoplastia reversa tensionada. Trata-se do primeiro caso relatado de excisão larga de mastectomia reconstruída exclusivamente com retalhos avançados em abdominoplastia reversa e alta tensão progressiva de pontos de adesão demostrando que nos pacientes selecionados, a pele abdominal pode ser avançada superiormente com segurança e facilidade para atingir a área superior do tórax e cobrir a área com defeito significante.
Palavras-chave: Abdominoplasti; Carcinoma ductal; Mastectomia; Parede torácica; Retalhos cirúrgicos.
The current advances in screening modalities and improved awareness are enabling the diagnose of most breast cancers at early stages; subsequently, less aggressive ablative surgery such as partial mastectomy, skin preserving and nipple preserving mastectomy became the procedure of choice for most newly diagnosed breast cancer patient. Nevertheless, more radical ablation may be required in certain circumstances making reconstruction of the resultant defect a major reconstructive challenge. Various reconstructive options are available1.
Although the majority of such defects could be repaired with the use of skin grafts or local and regional pedicled musculocutaneous flaps, more complicated cases require free flaps or increasingly sophisticated reconstructive techniques2. Classification systems have been proposed to help the systematic approach for reconstruction. Careful planning is necessary when considering optimal options, however, the exact choice remains specific for each patient depending on defect size, chest wall location, flap arch of rotation, and availability of recipient vessels for autologous microvascular composite tissue transfer1-4.
We present the case of a neglected large invasive ductal breast carcinoma. Following the mastectomy with wide skin excision, the defect was covered with a tensioned reverse abdominoplasty flap.
METHODS
This was a 64 year-old diabetic woman with BMI of 28 and past surgical history of 4 cesarean sections through a midline infraumbilical incision. She presented a massive left breast invasive ductal carcinoma originally diagnosed 4 years earlier. The patient has previously refused the surgery and was noncompliant with chemotherapy. Three months prior to her current presentation, the patient received 12 Gy of radiotherapy over 6 sessions. Subsequently, she developed painful rapid left breast edema and erythema. After ruling out an infectious process, the patient consented to undergo surgery.
Upon physical examination, she had a massively enlarged left breast mass measuring 10x10 cm in the lateral quadrants associated with peau d'orange and tense irradiated skin (Figures 1A and 1B). Besides a low hematocrit of 29, all of her other blood tests were within normal limits. She underwent a palliative left total mastectomy with ipsilateral axillary lymph nodes dissection. During the ablative surgery, the subcutaneous veins were found to be severely enlarged and engorged, therefore, resulting in heavy bleeding that was controlled by the application of heavy hemostatic sutures along the entire surgical incision (Figure 1C) and intra-operative transfusion with 2 units of whole blood. Gross axillary lymph node involvement was also noted extending to the brachial vessels and plexus. The resultant chest wall defect measured 25 x 20 cm (Figure 1D).

Figure 1. A, B - Neglected left breast tumor following 6 sessions of radiotherapy with preoperative planning for TRAM flap reconstruction. Midline infra-umbilical C-section scar indicated by an arrow. C, D - Left mastectomy and axillary node dissection with resultant large defect.
In view of the difficulties experienced by the general surgeon to control heavy bleeding and the palliative nature of the surgery with evidence of grossly residual tumor involvement of the axilla, it was necessary to minimize surgical trauma and limit surgical time. It was hence decided to abort the original preoperative plan to undergo TRAM flap with or without Latissimus dorsii flap and proceed to the reconstruction with a reverse abdominal flap.
An undermining of the left upper abdominal quadrant was performed extending to the level of the umbilicus and advanced superiorly to cover the defect with progressive tension 2-0 vicryl quilting sutures anchoring the flap to the lower costal margin and minimizing the dead space to insure closure of the wound under no tension. Two suction drains were inserted and exteriorized at the axilla (Figure 2A and 2B).
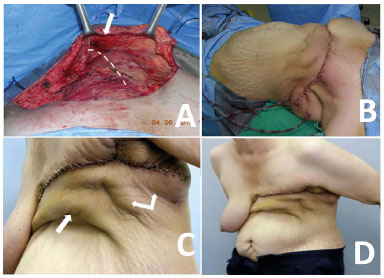
Figure 2. A - Undermining of the abdominal flap indicated by arrow limited to the left upper quadrant allowing mobilization of enough soft tissues to achieve primary closure of the defect. Costal margin highlighted by white dashed line. B - Abdominal flap advanced superiorly with tension quilting sutures. C, D - Immediate post-operative result demonstrating abdominal flap fixation to the costal margin indicated by single arrow and double arrow indicating additional quilting sutures to minimize dead space. Note superior skin recruitment allowing wound closure without tension.
RESULTS
The postoperative was uneventful with ambulation of the patient on the postoperative day one. The patient was discharged 2 days after surgery and drains were removed 6 days after surgery (Figure 2C and 2D). Skin staples were removed 12 days after the procedure. The patient had good wound healing with no evidence of seroma collection on follow up at week 5 (Figure 3).
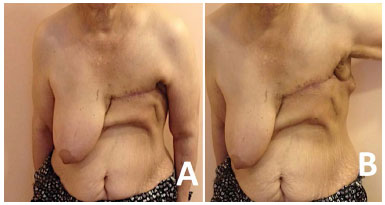
Figure 3. A, B - Stable wound healing 5 weeks after surgery with redundant superiorly recruited abdominal skin preventing tension due to gravity on the scar.
The pathology revealed an 11.5 cm invasive ductal carcinoma, grade 3, with lymphovascular invasion. The axillary lymph nodes were positive 20/20.
DISCUSSION
Reconstruction options for anterior chest wall defects can be complex and very challenging particularly following large tumor resection or when radiation therapy has been given pre-operatively or is being planned postoperatively5. Soft tissue flaps are often required to achieve primary wound healing when wide skin excision is mandated by oncologic considerations or even to cover alloplastic materials used to stabilize the chest wall5.
Many techniques have been described including pedicled muscle flaps such as pectoralis major, latissimus dorsi, rectus abdominis, and external oblique flaps, thoracoepigastric fasciocutaneous flap, omental flap, the contralateral breast as a glandular/myoglandular flap or even free flaps2,5-7. Occasionally, defects are so large that any single flap would be insufficient for coverage necessitating the simultaneous use of a combination of several flaps or complex chimeric flaps2,5.
In selected patients, the reverse abdominoplasty has been described as an alternative to pedicled or free flap reconstruction by recruiting adjacent abdominal tissue for reconstruction of thoracic defects following oncologic resections and for release of burn scar contractures in the upper epigastric region. Expanded reverse abdominoplasty was also described in patients with postburn scars involving the entire epigastric region to reconstruct the inframammary folds and correct breast contour. In these reconstructive cases, the upper abdominal wall tissue has been used either as a random or pedicled fasciocutaneous flap or as part of a musculocutaneous flap1,8,9.
Upper abdominal tissues have also been used in various forms for breast reconstruction10-12. In addition to improving upper abdominal contour, augmentation mammaplasty by reverse abdominoplasty (AMBRA) with autologous deepithelialized excess upper adipofascial abdominal wall tissue shaped as implants and transposed subglandularly has also been described13,14. The technique may probably be more advantageous for massive weight loss patients in whom upper abdominal contouring with concomitant breast augmentation can be performed to improve breast shape and projection8,15-17.
Despite its potential as a reconstructive procedure, the vast majority of reverse abdominoplasties are performed for aesthetic purposes; however, to date, the number of reported aesthetic reverse abdominoplasties remains very limited in the literature written in English language8. The technique implies tissue resection of the upper abdomen and results in submammary scars most often crossing the midline8,16,18,19.
Pantelides et al.1 in 2013 revealed two cases only describing the technique for reconstruction following oncological resection since 1984; the first is about closure of a massive chest wall defect resulting from resection of a chronic ulcer after radiation therapy for advanced breast carcinoma by a combination of multiple flaps including pectoralis major advancement flap, reverse abdominoplasty, omental flap, and latissimus dorsiscapular-parascapular musculofasciocutaneous flap20.
The second reports a very large dermatofibrosarcoma protuberans located in the epigastric area. After wide resection, the defect was reconstructed with a bilateral superiorly based mammaplasty combined with reverse abdominoplasty21.
Quilting sutures, the concepts of high lateral or superior tension abdominoplasty, and the principle of progressive tension sutures are not new; all these have been previously described with abdominoplasties. Results have been greatly improved and morbidity of simple dermolipectomy reduced. Abdominal flap fixation to the aponeurosis with progressive tension sutures not only minimizes the incidence of seroma formation by decreasing dead space and shear forces, it also greatly reduces the risk of skin necrosis and improves scar quality by distributing tension across the whole abdominal flap. It enables proper flap positioning and results in tension-free suture lines22-29.
To our knowledge, this is the first case reported on wide skin excision mastectomy reconstructed solely with a reverse abdominoplasty advancement flap and progressive high-tension quilting sutures demonstrating that in selected patient, abdominal skin can be safely and easily advanced superiorly to reach the upper chest area.
CONCLUSION
Reverse abdominoplasty is not a commonly procedure for aesthetic purposes primarily because of the poor quality of inframammary scars reported mainly whenever crossing the midline over the xyphoid8,28. Reconstructive potentials of this procedure, however, should not be underestimated. It is probably an excellent option for some patients. The surgical procedure is easy to perform. The dissection of the abdominal flap can be done safely bilateral and extending to under the umbilicus.
COLLABORATIONS
BA Analysis and/or interpretation of data; conception and design of the study; final approval of the manuscript; writing the manuscript or critical review of its contents; Completion of surgeries and/or experiments.
SD Analysis and/or interpretation of data; conception and design of the study; final approval of the manuscript; writing the manuscript or critical review of its contents; Completion of surgeries and/or experiments.
JA Analysis and/or interpretation of data; conception and design of the study; final approval of the manuscript; writing the manuscript or critical review of its contents; Completion of surgeries and/or experiments.
NP Analysis and/or interpretation of data; conception and design of the study; final approval of the manuscript; writing the manuscript or critical review of its contents; Completion of surgeries and/or experiments.
REFERENCES
1. Pantelides NM, Mondal D, Wishart GC, Malata CM. Reverse abdominoplasty: a practical option for oncological trunk reconstruction. Eplasty. 2013;13:e2.
2. Chang RR, Mehrara BJ, Hu QY, Disa JJ, Cordeiro PG. Reconstruction of complex oncologic chest wall defects: a 10-year experience. Ann Plast Surg. 2004;52(5):471-9. DOI: http://dx.doi.org/10.1097/01.sap.0000122653.09641.f8
3. Rohrich RJ, Lowe JB, Hackney FL, Bowman JL, Hobar PC. An algorithm for abdominal wall reconstruction. Plast Reconstr Surg. 2000;105(1):202-16. DOI: http://dx.doi.org/10.1097/00006534-200001000-00036
4. Losken A, Thourani VH, Carlson GW, Jones GE, Culbertson JH, Miller JI, et al. A reconstructive algorithm for plastic surgery following extensive chest wall resection. Br J Plast Surg. 2004;57(4):295-302. PMID: 15145731 DOI: http://dx.doi.org/10.1016/j.bjps.2004.02.004
5. Casal D, Fradinho N, Ramos L, Ferreira J, Varanda A, Diogo C, et al. Abdominoplasty and thoraco-epigastric flaps for large anterior trunk defects after dermatofibrosarcoma protuberans wide resection: Two illustrative cases. Int J Surg Case Rep. 2013;4(1):134-8. DOI: http://dx.doi.org/10.1016/j.ijscr.2012.11.002
6. Skoracki RJ, Chang DW. Reconstruction of the chestwall and thorax. J Surg Oncol. 2006;94(6):455-65. PMID: 17061266 DOI: http://dx.doi.org/10.1002/jso.20482
7. Atiyeh BS, Sfeir PM, Hayek SN. Mammary myocutaneous-glandular flap for reconstruction of oncological defects of the anterior midline chest wall. Scand J Plast Reconstr Surg Hand Surg. 2009;43(4):225-9. DOI: http://dx.doi.org/10.1080/02844310701514241
8. Wysocki WM, Komorowski AL, Kolodziejski LS. Chest wall defect reconstruction with contralateral breast. J Surg Oncol. 2007;95(8):680-1. DOI: http://dx.doi.org/10.1002/jso.20765
9. Shoham Y, Koretz M, Kachko L, Silberstein E, Krieger Y, Bogdanov-Berezovsky A. Immediate reconstruction of the chest wall by latissimus dorsi and vertical rectus abdominis musculocutaneous flaps after radical mastectomy for a huge pleomorphic liposarcoma. J Plast Surg Hand Surg. 2013;47(2):152-4. DOI: http://dx.doi.org/10.3109/2000656X.2012.748309
10. Hurwitz DJ, Agha-Mohammadi S. Postbariatric surgery breast reshaping: the spiral flap. Ann Plast Surg. 2006;56(5):481-6. DOI: http://dx.doi.org/10.1097/01.sap.0000208935.28789.2d
11. Kalender V, Aydin H, Karabulut AB, Ozcan M, Amiraslanov A. Breast reconstruction with the internal mammary artery pedicled fasciocutaneous island flap: description of a new flap. Plast Reconstr Surg. 2000;106(7):1494-8. DOI: http://dx.doi.org/10.1097/00006534-200012000-00007
12. Karabulut AB, Kalender V. Internal mammary artery pedicled island flap for the treatment of chest wall radionecrosis. Plast Reconstr Surg. 2001;108(2):583-4. PMID: 11496221 DOI: http://dx.doi.org/10.1097/00006534-200108000-00067
13. Pollock H, Pollock T. Progressive tension sutures in abdominoplasty. Clin Plast Surg. 2004;31(4):583-9. DOI: http://dx.doi.org/10.1016/j.cps.2004.03.015
14. Haik J, Grabov-Nardini G, Goldan O, Tessone A, Regev E, Mendes D, et al. Expanded reverse abdominoplasty for reconstruction of burns in the epigastric region and the inframammary fold in female patients. J Burn Care Res. 2007;28(6):849-53. DOI: http://dx.doi.org/10.1097/BCR.0b013e3181599b69
15. Baroudi R, Keppke EM, Carvalho CG. Mammary reduction combined with reverse abdominoplasty. Ann Plast Surg. 1979;2(5):368-73. DOI: http://dx.doi.org/10.1097/00000637-197905000-00002
16. Deos MF, Arnt RA, Gus EI. Tensioned reverse abdominoplasty. Plast Reconstr Surg. 2009;124(6):2134-41. PMID: 19952671 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181bf8353
17. Agha-Mohammadi S, Hurwitz DJ. Management of upper abdominal laxity after massive weight loss: reverse abdominoplasty and inframammary fold reconstruction. Aesth Plast Surg. 2010;34(2):226-31. DOI: http://dx.doi.org/10.1007/s00266-009-9432-y
18. Halbesma GJ, van Der Lei B. The reverse abdominoplasty: a report of seven cases and a review of English-language literature. Ann Plast Surg. 2008;61(2):133-7. DOI: http://dx.doi.org/10.1097/SAP.0b013e31815f6fb9
19. Berrino P, Campora E, Leone S, Santi P. Correction of type II breast deformities following conservative cancer surgery. Plast Reconstr Surg. 1992;90(5):846-53. PMID: 1410038 DOI: http://dx.doi.org/10.1097/00006534-199211000-00019
20. Bury TF, Reece GP, Janjan NA, McMurtrey MJ. Closure of massive chest wall defects after full-thickness chest wall resection. Ann Plast Surg. 1995;34(4):409-14. PMID: 7793789 DOI: http://dx.doi.org/10.1097/00000637-199504000-00013
21. Dagregorio G, Darsonval V. Aesthetic surgery techniques after excision of dermatofibrosarcoma protuberans: a case report. Br J Plast Surg. 2005;58(4):556-60. DOI: http://dx.doi.org/10.1016/j.bjps.2004.10.008
22. Pacifico MD, Mahendru S, Teixeira RP, Southwick G, Ritz M. Refining trunk contouring with reverse abdominoplasty. Aesthet Surg J. 2010;30(2):225-34. DOI: http://dx.doi.org/10.1177/1090820X10369690
23. Lockwood T. High lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96(3):603-15. DOI: http://dx.doi.org/10.1097/00006534-199509000-00012
24. Le Louarn C, Pascal JF. High superior tension abdominoplasty. Aesthetic Plast Surg. 2000;24(5):375-81. DOI: http://dx.doi.org/10.1007/s002660010061
25. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119(3):1060-4.
26. Mladick RA. Progressive tension sutures to reduce complications in abdominoplasty. Plast Reconstr Surg. 2001;107(2):619. DOI: http://dx.doi.org/10.1097/00006534-200102000-00058
27. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthetic Surg J. 1998;18(6):439-41. DOI: http://dx.doi.org/10.1016/S1090-820X(98)70073-1
28. Zienowicz RJ, Karacaoglu E. Augmentation mammaplasty by reverse abdominoplasty (AMBRA). Plast Reconstr Surg. 2009;124(5):1662-72. PMID: 20009853 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181babd02
29. Janis JE. Use of progressive tension sutures in components separation: merging cosmetic surgery techniques with reconstructive surgery outcomes. Plast Reconstr Surg. 2012;130(4):851-5. PMID: 23018696 DOI: http://dx.doi.org/10.1097/PRS.0b013e318262f1fd
American University of Beirut Medical Center, Beirut, Lebanon
Institution: American University of Beirut Medical Center, Beirut, Lebanon.
Corresponding author:
Nazareth Papazian
Cairo Street
1107-2020, Beirut, Lebanon Zip Code 11072020
E-mail: nazareth.j.papazian@gmail.com
Article received: January 5, 2014.
Article accepted: August 3, 2014.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter