

Original Article - Year 2016 - Volume 31 - Issue 2
Complications of otoplasty surgeries
Complicações em Otoplastia
ABSTRACT
INTRODUCTION: Protruding ears are caused by poor development of the antihelix, hyperplasia of the concha, abnormal cephaloauricular angle, a large and prominent lobule, or any combination of the above.
METHODS: A prospective study was performed, in which 60 patients who underwent otoplasty were followed up from January 2014 to January 2015 at the Hospital Municipal Barata Ribeiro.
RESULTS: Early complications included infection (0%), hematoma (1.6%), and skin necrosis (3.3%). Late complications included asymmetry (10%), recurrence (3.3%), extrusion of sutures (10%), granuloma formation (0%), hypertrophic scarring (0%), and keloid formation (0%). When patients were asked to rate the otoplasty, 3.3% stated that it was poor, 3.3% fair, 3.3% good, 3.3% very good, and 86.8% excellent.
CONCLUSION: The rates of early and late complications are similar to those described in the literature.
Keywords: Reconstructive surgical procedures; Postoperative complications; External ear abnormalities; Auricle.
RESUMO
INTRODUÇÃO: Orelha em abano é caracterizada pelo pobre desenvolvimento da anti-hélice, hiperplasia da concha, ângulo céfalo-auricular anormal, lóbulo grande e proeminente ou qualquer combinação dos itens citados.
MÉTODOS: Foi realizado um estudo prospectivo, em que foram acompanhados 60 pacientes submetidos à otoplastia, no período de janeiro de 2014 a janeiro de 2015, no Hospital Municipal Barata Ribeiro.
RESULTADOS: Entre as complicações precoces, citamos infecção (0%), hematoma (1,6%) e necrose de pele (3,3%). Entre as complicações tardias: assimetria (10%), recidiva (3,3%), extrusão de pontos (10%), granuloma, cicatriz hipertrófica (0%) e queloide (0%). Quando os pacientes foram questionados quanto aos resultados obtidos com a otoplastia, 3,3% responderam que o resultado foi ruim, 3,3% regular, 3,3% bom, 3,3% ótimo e 86,8% excelente.
CONCLUSÃO: As taxas de complicações precoces e tardias são semelhantes às descritas na literatura.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Complicações pós-operatórias; Orelha externa/anormalidades; Pavilhão auricular.
Protruding ears are caused by poor development of the antihelix, hyperplasia of the concha, abnormal cephaloauricular angle, large and prominent lobule, or any combination of the above1 (Figure 1).

Figure 1. A: Protruding ears, anterior view; B: Protruding ears, rear view.
Protrusion is the most frequent congenital abnormality of the external ear, with an approximate incidence of 5% in Caucasians, and affects both sexes equally2. Etiologically, it is a hereditary malformation, transmitted as an autosomal dominant pattern with variable penetrance2. In 60% of cases, it can be diagnosed at birth, but the deformity becomes more apparent in the first years of life3.
The ear comprises the auricle, which collects sound, and the external acoustic meatus, which conducts sound to the tympanic membrane4. The anatomical structure of the outer ear consists of three aligned complexes: the helix with a lobule, the antihelix with the antitragus, and the concha5 and other components.
In normal mature ears, the length varies from 5.5 to 6.5 cm, and the width varies from 50 to 60% of the length. The cephaloauricular angle is approximately 25º in males and 21º in females, while the scaphoconchal angle is 90º or less6. The ear is 10-12 mm removed from the scalp in the upper 1/3, 16-18 mm in the middle 1/3, and 20-22 mm in the lower 1/3 (lobule). The helix is projected in front of the antihelix and the lobule is projected medially to the lower third of the ear7.
OBJECTIVE
This study determined the percentages of early and late complications of otoplasties performed at the Hospital Municipal Barata Ribeiro, Rio de Janeiro, RJ, from January 2014 to January 2015.
METHODS
A prospective study was performed in 60 patients (ages 14-45 years, mean: 20 years) diagnosed with protruding ears, who underwent otoplasty surgery from January 2014 to January 2015.
All patients were referred from basic health care units to the Plastic Surgery clinic of the Hospital Municipal Barata Ribeiro. Patients were selected as candidates for otoplasty after joint evaluation by the surgical team and residents of the Hospital Municipal Barata Ribeiro. The criteria for exclusion were age less than 12 years, skin lesions close to the surgical site, and uncontrolled disease.
The candidates for otoplasty underwent clinical and laboratory tests, and were photographed. Signed consent was obtained during the preoperative consultation, with the understanding that surgery would be performed by residents under the supervision of the team. The surgical technique was previously described6.
The patients were discharged on the first postoperative day and were reevaluated in the first and second postoperative weeks, and first, second, and sixth postoperative months; all early and late complications of the otoplasty were documented by the team and residents.
Surgical Technique
All patients underwent surgery at the Surgical Center of the Hospital Municipal Barata Ribeiro. Intravenous cefazolin 2 g was administered 30 minutes before surgery, which was performed under local anesthesia using a solution of 1% lidocaine and epinephrine 1:200,000.
With the patient in dorsal decubitus and slight cranial elevation, surgical marking of the antihelix, concha, and retroauricular region was performed with a dermographic pen (Figure 2). With light pressure on the helix in the anteroposterior direction, the position of the antihelix was marked at four equidistant points at the top edge and four equidistant points on the bottom edge; the markings were parallel and symmetrical. Then, the excess concha, which was to be resected conservatively, was evaluated, with four points marked in the shape of a half moon, followed by the marking of a retroauricular skin spindle 2 mm above the groove.
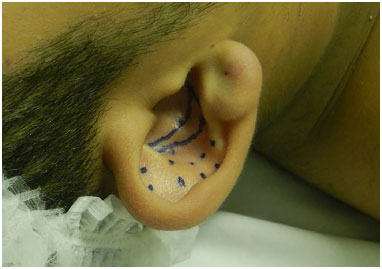
Figure 2. Preoperative marking of concha and antihelix.
The area was cleansed with 2% chlorhexidine and 0.5% alcohol chlorhexidine, surgical drapes were placed, and appropriate surgical garments were used by the team. The auditory canal was protected and subdermal local anesthesia was administered 1 mm below the ear lobule with a 1 ml syringe and insulin needle, followed by subdermal infiltration in the retroauricular, preauricular, and concha regions, to block the anterior and posterior branches of the great auricular nerve, auriculotemporal nerve, and branches of the glossopharyngeal and vagus nerves (Figure 3).

Figure 3. Asepsis and antisepsis.
We waited for 10 minutes, and tattooed the premarked points with a black needle and methylene blue according to the method of Davis and Kitlowski1. We began with the resection of the skin spindle in the posterior region of the middle ear, 2 mm above the groove, followed by detachment of the retroauricular flap superiorly until all points of the antihelix were visualized (Figure 4). This was followed by the withdrawal of the perichondrium in the posterior region of the antihelix and careful excision along its entire extension (Figure 5). Broad detachment of the concha from the mastoid was performed, with emphasis on the upper 1/3 of the ear and resection of excess concha according to the previous marking (Figures 6 and 7).

Figure 4. Spindle resection of the retroauricular skin.
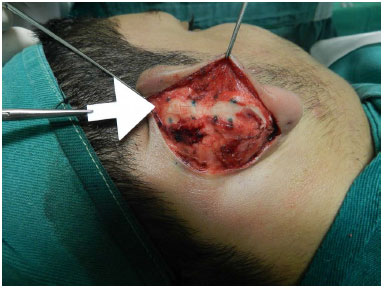
Figure 5. Posterior scraping of antihelix.

Figure 6. Detachment of the concha from the mastoid.
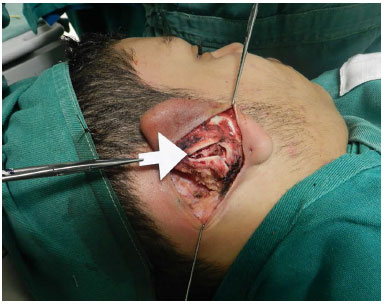
Figure 7. Resection of excess concha.
The antihelix was modeled with four Mustardé sutures, using 4.0 nylon, and the concha was rotated with three Furnas sutures, using 3.0 nylon, allowing a cephaloauricular distance of 6-10 mm in the upper 1/3, 12-16 mm in the middle 1/3, and 16-20 mm in the lower 1/3 (Figures 8 and 9). In patients with protrusion of the lobule, we performed a triangular resection of the skin in the lower 1/3 of the prior incision, which was repositioned with 5.0 nylon sutures, bypassing the skin of the anterior incision, periosteum of the mastoid, and posterior skin incision. We assessed hemostasis and began the skin suturing with 5.0 nylon.
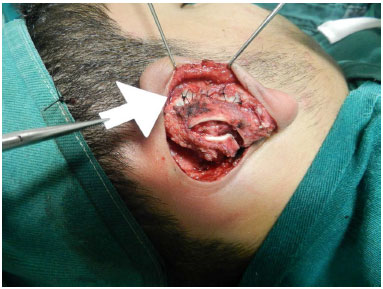
Figure 8. Modeling of the antihelix with Mustardé sutures.

Figure 9. Rotation of the ear with scaphotemporal sutures for the upper 1/3 and Furnas suture for the middle and lower 1/3.
Dressing was placed with moist sterile cotton modeling the concha and scapha, with sterile gauze in the posterior region of the ear, and coverage of the ear with cushioned gauze, followed by sterile bandaging of the head.
Postoperative management included a prescription of analgesics, antibiotics (oral cephalexin 500 mg for 7 days), daily cleaning, and use of a protective earband.
RESULTS
Early complications included infection (0%), hematoma (1.6%), and skin necrosis (3.3%) (Figure 11). Late complications included asymmetry (10%), recurrence (3.3%), extrusion of sutures (10%), granuloma formation (0%), hypertrophic scarring (0%), and keloid formation (0%) (Figures 10, 11, and 12). When the patients were asked to rate the otoplasty, 3.3% stated that the result was poor, 3.3% fair, 3.3% good, 3.3% very good, and 86.8% excellent.

Figure 10. Late hematoma, right ear, third postoperative week.

Figure 11. A: Protruding ears, preoperative period; B: Sixth postoperative month, showing poor positioning.
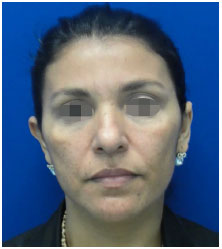
Figure 12. Sixth postoperative month, showing recurrence in the right upper 1/3.
DISCUSSION
Although individuals with protruding ears do not experience loss or reduction in the capture and conduction of sound, the deformity may negatively influence their social life. Protruding ears are minor deformities, but provoke joking, mainly among children, and may lead to a decline in the quality of life, resulting in poor performance at school and work, social avoidance, and decreased self-confidence2.
Thus, the ideal age to perform otoplasty is between 6 and 7 years, since the individual will have completed growth of almost the entire ear and will begin school integration8.
The rates of complications in otoplasties published in the literature are somewhat variable, and are associated with the experience of the surgeon and the surgical technique employed. Aki et al.3 reviewed 508 cases of otoplasty surgeries performed by plastic surgery residents under supervision, with predominant use of a combination of Mustardé and Furnas sutures; infection occurred in 5.1% of cases, followed by hematoma (4.2%) and skin necrosis (2.5%). The most frequent late complication was poor positioning, which occurred in 11% of cases, and 3.1% of patients required reoperation due to relapse. Complications related to suturing were observed in 6.1% of cases, with late extrusion (4.1%) and granuloma (2.0%), followed by hypertrophic scarring and keloid formation (3.3%).
Yugueros and Friedland9 reported a suture extrusion rate of 10%. Calder and Nassan10 reviewed 562 cases performed by residents and preceptors (Senior House Officers, Registrars, Senior Registrars, and Consultants), whose technique included anterior excision; complications included infection (5.2%), hematoma (2.0%), anterior skin necrosis (1.4%), residual deformity (8%), and keloid formation and hypertrophic scarring (2.1%).
We followed 60 patients in our study, and used a surgical technique described by Whiters. No cases of infection were found. We attribute this result to stringent asepsis and antisepsis during surgery; antibiotic prophylaxis with intravenous cefazolin 2 g, 30 minutes before surgical incision; and oral antibiotic therapy with cephalexin 500 for seven days in the postoperative period. We observed only one case of hematoma (1.6%), which occurred in the third postoperative week, with the hematoma located on the lower 1/3 of the ear, next to the lobule.
The main cause of hematoma is inadequate hemostasis10, but other causes should be taken into account, such as trauma, use of anti-inflammatory agents, antiplatelet agents and anticoagulants, and hematologic diseases. Hematomas frequently occur in the immediate postoperative period, presenting a clinical picture of pain and local convexity, and may be complicated by skin necrosis and infection, leading to catastrophic chondritis, which is treated by cartilage debridement, and leads to other sequelae and residual deformities3,11.
Hematoma treatment consists of immediate drainage. As late hematoma can occur without pain, serial follow-up is of utmost importance, with instructions to return immediately if the patient perceives some alteration in the postoperative period. There were two cases of slight necrosis (3.3%) located in the concha. The main causes of necrosis are excessive use of electrocautery and excessive dressing pressure10.
In our study, we found that the cases of necrosis were due to the excessive use of electrocautery during hemostasis at the withdrawal site of the conchal cartilage. Treatment is conservative, consisting of daily dressing, washing with saline solution, cleaning of the edges of the wound with alcohol 70%, and dressing with sterile gauze, thus promoting the closure of the wound by second intention.
We found eight cases of poor positioning, six (10%) with asymmetry and two (3.3%) of recurrence. The main factor contributing to asymmetry in the postoperative period was the degree of protrusion of the ears, and was more evident in patients with an increased cephaloauricular angle. Another factor that influences asymmetry in the postoperative period is the vertical dimension of the ear; recurrence factors include the early rupture of sutures, hematoma, and infection.
Messener and Crysdale12 reported that ears with vertical dimension less than 50mm had a greater tendency to maintain the corrected position, which was established immediately after surgery, for long term8. Sutures maintain the ear in the new position until the formation of fibrosis13; hematoma and infection impair the healing process and contribute to relapse3.
The loss of correction of the upper pole was reported by Messener and Crysdale in patients who underwent posterior excision with Mustardé and Furnas sutures. The corrected ears returned to the preoperative position in 33.3% of cases, and 33.3% of the cases returned to an intermediate position between the corrected and preoperative state. Despite this loss of correction of the upper 1/3, 85% of patients were satisfied with the outcome8. For the correction of the lateralization of the upper 1/3, Adamson recommended adding suturing of the triangular fossa to the temporal fascia8.
To avoid lateralization of the upper 1/3 after otoplasty, we started to use scaphotemporal suturing and obtained better symmetry and control of the upper 1/3. We found six cases (10%) of complications related to sutures. The sutures used were of 4.0 nylon for modeling of the antihelix and 3.0 nylon for the rotation of the concha. As nonabsorbent suture causes less tissue reaction and has good resistance to tension, we used nylon.
We attribute the high percentage of late extrusion to the thickness of the wire used for the rotation of the concha. The patients experience symptoms of discomfort in the posterior region of the ear and the sutures become visible. Management included daily local cleaning and scheduled removal of the suture after the sixth month. There was no case of keloid formation or hypertrophic scarring. Keloid formation can be caused by tension on the suture14, and is more common in black individuals. Treatment involves intralesional resection, infiltration with corticosteroids, and beta radiation therapy.
CONCLUSION
The rates of early and late complications are similar to those described in the literature.
COLLABORATIONS
FVB Analysis and/or data interpretation; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; writing of the manuscript or critical review of its contents.
CEJB Analysis and/or data interpretation; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; writing of the manuscript or critical review of its contents.
RC Analysis and/or data interpretation; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; writing of the manuscript or critical review of its contents.
RFA Analysis and/or data interpretation; statistical analysis; completion of operations and/or experiments.
REFERENCES
1. Spira M, McCrea R, Gerow FJ, Hardy SB. Correction of the principal deformities causing protruding ears. Plast Reconstr Surg. 1969;44(2):150-4. DOI: http://dx.doi.org/10.1097/00006534-196944020-00007
2. Braun T, Hainzinger T, Stelter K, Krause E, Berghaus A, Hempel JM. Health-related quality of life, patient benefit, and clinical outcome after otoplasty using suture techniques in 62 children and adults. Plast Reconstr Surg. 2010;126(6):2115-24. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181f449c7
3. Aki F, Sakae E, Cruz DP, Kamakura L, Ferreira MC. Complicações em otoplastia: revisão de 508 casos. Rev Bras Cir Plást. 2006;21(3):140-4.
4. Moore KL, Dalley AF. Anatomia orientada para a clínica. Rio de Janeiro: Guanabara Koogan; 2001.
5. Porter CJ, Tan ST. Congenital auricular anomalies: topographic anatomy, embryology, classification, and treatment strategies. Plast Reconstr Surg. 2005;115(6):1701-12. DOI: http://dx.doi.org/10.1097/01.PRS.0000161454.08384.0A
6. Mélega JM. Cirurgia plástica: fundamentos e arte: princípios gerais. Rio de Janeiro: Guanabara Koogan; 2011.
7. Janz BA, Cole P, Hollier LH Jr, Stal S. Treatment of prominent and constricted ear anomalies. Plast Reconstr Surg. 2009;124(1 Suppl):27e-37e. PMID: 19568137 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181aa0e9d
8. Janis JE, Rohrich RJ, Gutowski KA. Otoplasty. Plast Reconstr Surg. 2005;115(4):60e-72e. PMID: 15793433
9. Yugueros P, Friedland JA. Otoplasty: the experience of 100 consecutive patients. Plast Reconstr Surg. 2001;108(4):1045-51.
10. Calder JC, Naasan A. Morbidity of otoplasty: a review of 562 consecutive cases. Br J Plast Surg. 1994;47(3):170-4. PMID: 8193854
11. Hoehn JG, Ashruf S. Otoplasty: sequencing the operation for improved results. Plast Reconstr Surg. 2005;115(1):5e-16e. PMID: 15622225
12. Messner AH, Crysdale WS. Otoplasty. Clinical protocol and long-term results. Arch Otolaryngol Head Neck Surg. 1996 Jul;122(7):773-7. PMID: 8663953
13. Miyamoto J, Nagasao T, Tamaki T, Nakajima T. Biomechanical evaluation of surgical correction of prominent ear. Plast Reconstr Surg. 2009;123(3):889-96. PMID: 19319052
14. Caouette-Laberge L, Guay N, Bortoluzzi P, Belleville C. Otoplasty: anterior scoring technique and results in 500 cases. Plast Reconstr Surg. 2000;105(2):504-15. PMID: 10697153
1. Hospital Municipal Barata Ribeiro, Rio de Janeiro, RJ, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital Municipal Barata Ribeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Felipe Vargas Borges
Rua Barão de São Francisco, 245, bloco 2, apto. 1401 - Vila Isabel
Rio de Janeiro, RJ, Brazil Zip Code 20560-031
E-mail: felipevargasborges@gmail.com
Article received: September 6, 2015.
Article accepted: April 10, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter