

Original Article - Year 2016 - Volume 31 -
Lateral thoracic fasciocutaneous flap for reconstruction of axillary defects after resection of hidradenitis suppurativa: a series of 10 cases
Retalho fasciocutâneo torácico lateral para reconstrução de defeitos axilares após ressecção de hidradenite supurativa: série de 10 casos
ABSTRACT
INTRODUCTION: Hidradenitis suppurativa (HS) is a chronic follicular inflammation that presents varied clinical features, from isolated small nodules to several abscessed lesions, with formation of fistulas and scars. The axillary region is one of the most frequently affected areas. The objective is to evaluate a series of patients with HS in the axillary region who underwent extensive surgical excision and reconstruction with a lateral thoracic fasciocutaneous flap.
METHODS: A retrospective analysis of the medical records of patients who underwent treatment between 2010 and 2012 was conducted.
RESULTS: Ten patients were operated, of whom two had bilateral involvement, totaling 12 procedures. The mean progression time before the surgical indication was 38 months. The mean defect size after the resection was 10 x 9 cm. The mean size of the flaps was 15 x 10 cm. With regard to early complications, two cases of dehiscence (axillary region) and one case of partial epitheliolysis (distal segment of the flap) were observed.
CONCLUSION: We observed that dissection of lateral thoracic fasciocutaneous flaps is not technically difficult and does not present significant functional or aesthetic sequelae in the donor area, making it a reliable and versatile option for reconstruction of larger axillary defects.
Keywords: Axilla; Skin/injuries; Cutaneous fistula; Surgical flaps/surgery; Wound closure techniques; Hidradenitis suppurativa.
RESUMO
INTRODUÇÃO: A hidradenite supurativa (HS) é uma inflamação folicular crônica que apresenta quadro clínico variado, desde pequenos nódulos isolados até diversas lesões abscedadas, com formação de fístulas e cicatrizes. A região axilar é uma das áreas mais frequentemente acometidas. O objetivo é analisar uma série de casos acometidos por HS na região axilar, submetidos à exérese cirúrgica ampliada e reconstrução com retalho fasciocutâneo torácico lateral.
MÉTODOS: Análise retrospectiva dos prontuários dos pacientes submetidos a tratamento no período entre 2010 e 2012.
RESULTADOS: Dez pacientes foram operados, sendo que em dois havia acometimento bilateral, totalizando 12 procedimentos. Foi observado um tempo médio de evolução antes da indicação cirúrgica de 38 meses. O defeito médio observado após a ressecção foi de 10 x 9 cm. O tamanho médio dos retalhos foi de 15 x 10 cm. Em relação às complicações precoces, foram observados dois casos de deiscência (região axilar) e um caso de epiteliólise parcial (segmento distal do retalho).
CONCLUSÃO: Observamos que a dissecção deste retalho não é tecnicamente difícil e que não apresenta sequelas funcionais ou estéticas significativas na área doadora, sendo uma opção confiável e versátil para reconstrução de defeitos axilares de maior porte.
Palavras-chave: Axila; Pele/lesões; Fístula cutânea; Retalhos cirúrgicos/cirurgia; Técnicas de fechamento de feridas; Hidradenite supurativa.
Hidradenitis suppurativa (HS) is a chronic follicular inflammation that can affect the axillary, submammary, inguinal-crural, and perineal regions, among others. It presents varied clinical features, from small isolated nodules to several abscessed lesions, with high incidence rates of inflammatory process, and fistula and scar formations. It affects females more often than males, at a ratio of 3:1, with greater incidence from the second to the fourth decade of life1-6.
The etiology is not fully known, and the most accepted mechanism is occlusion of the terminal portion of the follicular infundibulum due to drainage difficulty1,4,7. As a consequence, follicular duct dilation occurs until its rupture, with the release of fragments of the follicular epithelium and the cells of the bulbar region, generating an inflammatory process. Usually, bacterial cultures yield negative results and patients may not respond to antibiotic therapy. Secondary bacterial infections may occur8-10.
The clinical presentation begins normally in puberty, with an insidious onset, and inflammatory and solitary nodules, or a more aggressive onset, with various abscesses and fistulas. The lesions can be initially diagnosed as furuncles; however, they do not present central necrosis, are deeper, and may not present purulent drainage11,12.
The lesions may be painful and remain without drainage for long periods. Complete regression may occur but sequelae are frequent, with large areas of fibrosis, retraction, and even lymphedema11,13,14.
In accordance with the classification of Hurley, HS can be divided into the following phases: phase I, with single or multiple abscesses, without fistula or cicatricial fibrosis, and clinical treatment is possible; phase II, with recurring abscesses/fistulas and scars, with clinical or excisional treatment; and phase III, with multiple interconnected abscesses, fistulas and fibrosis, with extensive excisions being recommended in the areas affected2,4,10,11,15.
The diagnosis of HS is clinical, with no need of complementary examinations, but no criteria have been preestablished. The main differential diagnoses are Crohn disease, donovanosis (granuloma inguinale), acne (nodular-cystic), and other chronic folliculitis1,3,7,10.
OBJECTIVE
The objective of this report was to evaluate a series of patients with HS in the axillary region who underwent extensive surgical excision and reconstruction with a lateral thoracic fasciocutaneous flap, regarding indications, surgical technique, results, and complications.
METHODS
Medical and photographic records of patients who underwent surgical treatment of HS in the axillary region and repair with a lateral thoracic fasciocutaneous flap between 2010 and 2012 at the Irmandade da Santa Casa de Misericórdia de São Paulo Central Hospital, São Paulo, SP, Brazil, were retrospectively analyzed.
The mean time of disease progression (before surgical indication), dimensions of the defect after resection, dimensions of the flap, hospitalization time, and complications (early and late) were analyzed.
Early complications were those that occurred up to 30 days after the operation, and late complications were those that occurred after this period.
In cases with bilateral involvement, the procedures were performed separately with a minimum interval of 30 days.
Surgical Technique
The patient was placed in the dorsal decubitus position, with abduction of the upper limb by 90º, under general anesthesia. Extensive resection of the fibrotic-scar tissue and areas of fistulas was performed en bloc, with a mean margin of 1 cm, including the whole thickness of the subcutaneous tissue (Figure 1).

Figure 1. Bloody area after resection of the left axillary hidradenitis and demarcation of the lateral thoracic fasciocutaneous flap.
After resection, the bloody area was measured to facilitate the demarcation of the flap. The fasciocutaneous transposition flap of the lateral thoracic region was used, up to the submammary region when necessary (Figure 2). The donor area was closed by using planes. Aspiration drainage was routinely performed (Figure 3).
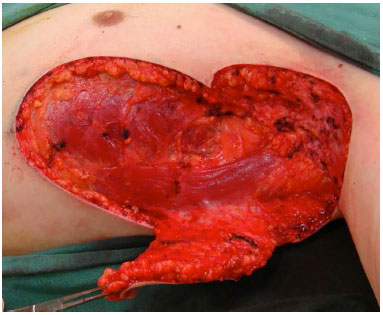
Figure 2. A dissected flap.

Figure 3. Appearance in the immediate postoperative period.
RESULTS
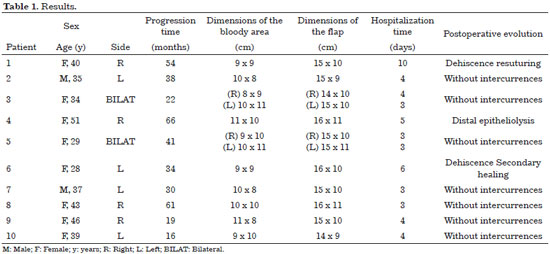
Ten patients were evaluated, of whom two had bilateral involvement, totaling 12 procedures.
The mean progression time before the surgical indication was 38 months. All the patients had already undergone various types of clinical treatment (topical and systemic) and smaller surgeries (partial/sequential resections) but without resolution of the disease (Table 1).
The mean defect size after the resection was 10 x 9 cm, including the skin and subcutaneous tissue in the total thickness. The mean size of the fasciocutaneous flaps was 15 x 10 cm. Primary closure of the donor area was possible in all the cases (Figures 4 to 7; Table 1).

Figure 4. Left axillary hidradenitis: areas of fibrosis and cicatricial retraction.

Figure 5. Bloody area after resection of the left axillary hidradenitis and demarcation of the lateral thoracic fasciocutaneous flap.

Figure 6. Appearance in the immediate postoperative period.

Figure 7. Appearance at 12 months after operation.
The mean time of resection of the HS was 45 minutes, and the completion of the flap described was 80 minutes. No intraoperative complications occurred, and the mean hospitalization time was 4.3 days.
With regard to early complications, two cases of dehiscence (axillary region) were observed, one of which was resolved with debridement and suturing, and the other was resolved with dressings and secondary healing. One case of partial epitheliolysis (distal segment of flap), about 2 cm, was also observed with spontaneous resolution. No complications related to the donor area were observed.
Regarding late complications, we observed one case of recurrence or residual disease, which was treated with new resection and advancement of the previously used flap, and one case of limitation in abduction of the upper limb (due to cicatricial contracture), treated with zplasties and physiotherapy.
DISCUSSION
HS is one of the dermatological diseases that greatly affect the patient's quality of life. The etiological factors include obesity, diet rich in sugar and milk, smoking, use of illicit drugs, and genetic predisposition12,13.
Various clinical and surgical treatments have been described1,2,4,14-17. Regardless of disease stage and the treatment chosen, patients should receive general guidelines, including avoidance of skin damage to the regions affected (e.g., avoidance of rubbing or the use of tight clothes); use of neutral products for local hygiene; cessation of smoking habit; and weight loss10-12. Psychological support should also be provided because it is a chronic disease13-15.
Phase I Hurley lesions may be treated with topical antibiotic therapy associated or not with oral anti-inflammatory agents and infiltration with corticosteroids. Systemic antibiotics can also be administered2,3,4,8.
Phase II Hurley cases may be treated with systemic antibiotic therapy. Another option is hormonal therapy with antiandrogenic medications. Surgical procedures for partial and sequential resections should also be considered2,3,4,8.
For cases of more-advanced stages, such phase III Hurley lesions, immunomodulators such as infliximab can be used, which have shown favorable results, or corticoid pulse. At this stage, extensive surgical excision is indicated. The morbidity associated to advanced stages is significant2-4,8,16-19.
In the axillary region, repair after extensive resection of areas affected by HS is highly possible. Options include healing by second intention (although it typically progresses in the long term with difficulties in healing and contractures), closing with primary suture, partial skin grafting, and the use of local (cutaneous, fasciocutaneous, and musculocutaneous flaps) or regional flaps (fasciocutaneous and musculocutaneous)16-19.
In relation to the extension of local treatment of HS cases, Watson20 presented a review of 72 cases and reported a lower rate of reoperation (13%) after extensive local excision and use of a partial skin graft. Paletta19 also reported a lower rate of reoperation (19%) for reconstruction with local flaps. Rompel and Petres21 evaluated 106 patients and reported that the recurrence of the disease is related to the more advanced forms, demonstrating that early and radical excision should be the treatment of choice.
Axillary reconstruction techniques with flaps include scapular and parascapular fasciocutaneous flaps, with pedicles based on the circumflex artery branches of the scapula22. One can use flaps based on perforating vessels of the lateral thoracic artery, with local advancement in double opposing flaps23 or in forward V-Y flaps24. Flaps based on perforating vessels of the thoracodorsal artery, described by Cabanie et al., can also be used25,26.
Rhomboid skin and fasciocutaneous flaps can safely be used, although their perforating vessels are not specifically identified during the procedure27.
CONCLUSION
The lateral thoracic fasciocutaneous flap is a reliable and versatile option for reconstruction of larger axillary defects, as in the cases presented after the surgical excision of HS. We observed that the dissection of this flap is not technically difficult and does not present significant functional or aesthetic sequelae in the donor area.
COLLABORATIONS
DFM Conception and design of the study; analysis and/or data interpretation; statistical analysis; completion of operations; writing of the manuscript and critical review of its content; and final approval of the manuscript
AHJ Conception and design of the study; completion of operations; writing of the manuscript and critical review of its content; and final approval of the manuscript
REFERENCES
1. Revuz J. Hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2009;23(9):985-98. DOI: http://dx.doi.org/10.1111/j.1468-3083.2009.03356.x
2. Wiseman MC. Hidradenitis suppurativa: a review. Dermatol Ther. 2004;17(1):50-4. DOI: http://dx.doi.org/10.1111/j.1396-0296.2004.04007.x
3. Alikhan A, Lynch PJ, Eisen DB. Hidradenitis suppurativa: a comprehensive review. J Am Acad Dermatol. 2009;60(4):539-61. DOI: http://dx.doi.org/10.1016/j.jaad.2008.11.911
4. Jemec GB. Clinical practice. Hidradenitis suppurativa. N Engl J Med. 2012;366(2):158-64. DOI: http://dx.doi.org/10.1056/NEJMcp1014163
5. Revuz JE, Canoui-Poitrine F, Wolkenstein P, Viallette C, Gabison G, Pouget F, et al. Prevalence and factors associated with hidradenitis suppurativa: results from two case-control studies. J Am Acad Dermatol. 2008;59(4):596-601. PMID: 18674845 DOI: http://dx.doi.org/10.1016/j.jaad.2008.06.020
6. Jemec GB, Heidenheim M, Nielsen NH. The prevalence of hidradenitis suppurativa and its potential precursor lesions. J Am Acad Dermatol. 1996;35(2 Pt 1):191-4. DOI: http://dx.doi.org/10.1016/S0190-9622(96)90321-7
7. Danby FW, Margesson LJ. Hidradenitis suppurativa. Dermatol Clin. 2010;28(4):779-93. DOI: http://dx.doi.org/10.1016/j.det.2010.07.003
8. Slade DE, Powell BW, Mortimer PS. Hidradenitis suppurativa: pathogenesis and management. Br J Plast Surg. 2003;56(5):451-61. DOI: http://dx.doi.org/10.1016/S0007-1226(03)00177-2
9. von der Werth J, Wood P, Irvine AD, McLean WHI. Genetics of hidradenitis suppurativa. In: Jemec GBE, Revuz J, Leyden JJ, eds. Hidradenitis Suppurativa. Heidelberg: Springer; 2006. p.70-85.
10. von der Werth JM, Williams HC. The natural history of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2000;14(5):389-92. DOI: http://dx.doi.org/10.1046/j.1468-3083.2000.00087.x
11. Sartorius K, Emtestam L, Jemec GB, Lapins J. Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol. 2009;161(4):831-9. PMID: 19438453 DOI: http://dx.doi.org/10.1111/j.1365-2133.2009.09198.x
12. Simonart T. Hidradenitis suppurativa and smoking. J Am Acad Dermatol. 2010;62(1):149-50. PMID: 20082894 DOI: http://dx.doi.org/10.1016/j.jaad.2009.08.001
13. Esmann S, Jemec GB. Psychosocial impact of hidradenitis suppurativa: a qualitative study. Acta Derm Venereol. 2011;91(3):328-32. PMID: 21394419 DOI: http://dx.doi.org/10.2340/00015555-1082
14. Jemec GB, Heidenheim M, Nielsen NH. Hidradenitis suppurativa-characteristics and consequences. Clin Exp Dermatol. 1996;21(6):419-23.
15. von der Werth JM, Jemec GB. Morbidity in patients with hidradenitis suppurativa. Br J Dermatol. 2001;144(4):809-13. PMID: 11298541 DOI: http://dx.doi.org/10.1046/j.1365-2133.2001.04137.x
16. Soldin MG, Tulley P, Kaplan H, Hudson DA, Grobbelaar AO. Chronic axillary hidradenitis--the efficacy of wide excision and flap coverage. Br J Plast Surg. 2000;53(5):434-6. DOI: http://dx.doi.org/10.1054/bjps.1999.3285
17. Kagan RJ, Yakuboff KP, Warner P, Warden GD. Surgical treatment of hidradenitis suppurativa: a 10-year experience. Surgery. 2005;138(4):734-40. DOI: http://dx.doi.org/10.1016/j.surg.2005.06.053
18. Gorkisch K, Boese-Landgraf J, Vaubel E. Hidradenitis suppurativa-treatment with myocutaneous island flap or the traditional method. Handchir Mikrochir Plast Chir. 1984;16(2):135-8. PMID: 6745753
19. Paletta FX. Hidradenitis suppurativa: pathologic study and use of skin flaps. Plast Reconstr Surg. 1963;31:307-15. PMID: 13941196 DOI: http://dx.doi.org/10.1097/00006534-196304000-00001
20. Watson JD. Hidradenitis suppurativa--a clinical review. Br J Plast Surg. 1985;38(4):567-9. DOI: http://dx.doi.org/10.1016/0007-1226(85)90022-0
21. Rompel R, Petres J. Long-term results of wide surgical excision in 106 patients with hidradenitis suppurativa. Dermatol Surg. 2000;26(7):638-43. DOI: http://dx.doi.org/10.1046/j.1524-4725.2000.00043.x
22. Nişanci M, Er E, Işik S, Sengezer M. Treatment modalities for post-burn axillary contractures and the versatility of the scapular flap. Burns. 2002;28(2):177-80. PMID: 11900943 DOI: http://dx.doi.org/10.1016/S0305-4179(01)00090-0
23. Geh JL, Niranjan NS. Perforator-based fasciocutaneous island flaps for the reconstruction of axillary defects following excision of hidradenitis suppurativa. Br J Plast Surg. 2002;55(2):124-8. PMID: 11987945 DOI: http://dx.doi.org/10.1054/bjps.2001.3783
24. Rehman N, Kannan RY, Hassan S, Hart NB. Thoracodorsal artery perforator (TAP) type I V-Y advancement flap in axillary hidradenitis suppurativa. Br J Plast Surg. 2005;58(4):441-4. DOI: http://dx.doi.org/10.1016/j.bjps.2004.10.022
25. Cabanie H, Garbe JF, Guimberteau JC. Les bases anatomiques du lambeau axillaire thoracodorsal en vue de son transfert par microchirurgie vasculaire. Anat Clin. 1979;2(1):65-73. DOI: http://dx.doi.org/10.1007/BF01654450
26. Guerra AB, Metzinger SE, Lund KM, Cooper MM, Allen RJ, Dupin CL. The thoracodorsal artery perforator flap: clinical experience and anatomic study with emphasis on harvest techniques. Plast Reconstr Surg. 2004;114(1):32-41. PMID: 15220564 DOI: http://dx.doi.org/10.1097/01.PRS.0000129071.03842.C5
27. Varkarakis G, Daniels J, Coker K, Oswald T, Akdemir O, Lineaweaver WC. Treatment of axillary hidradenitis with transposition flaps: a 6-year experience. Ann Plast Surg. 2010;64(5):592-4. PMID: 20395816 DOI: http://dx.doi.org/10.1097/SAP.0b013e3181da1c4f
Irmandade da Santa Casa de Misericórdia de São Paulo (ISCMSP), São Paulo, SP, Brazil
Institution: Irmandade da Santa Casa de Misericórdia de São Paulo (ISCMSP), São Paulo, SP, Brazil.
Corresponding author:
Daniel Francisco Mello
Rua Mato Grosso, 128 - Higienópolis
São Paulo, SP, Brazil Zip Code 01239-040
E-mail: mello.plastica@gmail.com
Article received: July 29, 2013.
Article accepted: February 4, 2014.
Conflicts of interest: none.
* Nemer Chidid 2013 Award Winner.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter