ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Giant lipoma of the buccal fat pad: case report and literature review
Lipoma gigante do coxim adiposo bucal: relato de caso e revisão da literatura
ABSTRACT
INTRODUCTION: Lipomas are the most common benign mesenchymal tumors. Nevertheless, they are infrequent in the face, particularly giant lipomas, which are derived from the buccal fat pad. The literature regarding these tumors is scarce and their incidence is likely underestimated.
METHODS: We present a case report of surgical treatment of a relapsed giant buccal and temporal lipoma and review the related English literature in Pubmed and that in the Brazilian Journal of Plastic Surgery.
RESULTS: The tumor, which anatomically and morphologically corresponded to the buccal fat pad, was completely excised by facial and temporal access without sequelae to the facial nerve. A total of 31 reported cases of lipoma originating from the buccal fat pad were found; however, several were found and reported under other names.
DISCUSSION: The buccal fat pad is larger and more complex than assumed, and several pathologies are derived thereof, making the differential diagnosis of simple lipoma with fusiform cell lipoma and liposarcoma difficult due to their extreme similarities.
CONCLUSION: In lipomatous lesions of the face, the possible origin in the buccal fat pad must be considered. An extensive study of these lesions with the purpose of standardizing the terminology and determining its real incidence must be performed.
Keywords:
Lipoma; Lipomatosis; Dual symmetric lipomatosis; Local relapsed neoplasia; Surgery.
RESUMO
INTRODUÇÃO: Lipomas são os tumores benignos mesenquimais mais comuns. Entretanto, são pouco frequentes na face, principalmente o tipo considerado gigante, derivado do coxim adiposo bucal. A literatura é escassa e provavelmente a sua incidência é subestimada.
MÉTODO: Relato do caso de tratamento cirúrgico de lipoma gigante bucal e temporal recidivado, e revisão da literatura no Pubmed na língua inglesa e na Revista Brasileira de Cirurgia Plástica.
RESULTADOS: O tumor, anatômica e morfologicamente, corresponde ao coxim adiposo bucal, foi totalmente retirado pelo acesso facial e temporal, sem sequelas ao nervo facial. Foram encontrados 31 casos relatados de lipoma de origem do coxim adiposo bucal, entretanto, vários casos foram encontrados e relatados sob outras denominações.
DISCUSSÃO: O coxim adiposo bucal é maior e mais complexo que se conhecia, e várias patologias se derivam deste, sendo importante o diagnóstico diferencial do lipoma simples com o de células fusiformes e com o lipossarcoma, devido a sua extrema semelhança.
CONCLUSÃO:Nas lesões lipomatosas da face, a possível origem no coxim adiposo bucal deve ser considerada. Um estudo amplo dessas lesões com a finalidade de uniformizar a terminologia e de determinar a sua real incidência deve ser realizado.
Palavras-chave:
Lipoma; Lipomatose; Lipomatose simétrica dupla; Recidiva local de neoplasia; Cirurgia.
INTRODUCTION
Lipomas are neoplasms composed of mature adipose cells that represent the most common benign mesenchymal tumors and can be found in all sites containing fatty tissue. Occurring more commonly in the chest and extremities, impairment of the head and neck is less frequent, representing approximately 13-20% of cases. The majority of lesions in this region are located in the posterior portion of the neck and rarely develop in the anterior neck, face, and other regions1,2. Upon searching the international literature, we found only 31 cases of buccal fat pad lipoma, buccal fat pad, or Bichat ball, which indicates the rarity of this disease and even suggests a possible underreporting of cases3.
Here, we report a case of relapsed giant lipoma of the buccal fat pad that was treated at the Federal Hospital of Andaraí, Rio de Janeiro, RJ.
METHOD
Case Report
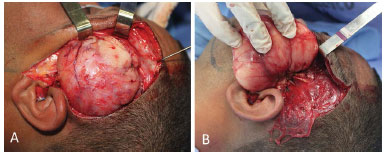
Patient PSRC, a 29-year-old man, sought medical care at the Microsurgery of the Plastic Surgery Service, Hospital Federal Andaraí, for excision of a tumor in the temporal region measuring approximately 10 cm and another tumor in the face measuring approximately 10 cm in its largest axis that had progressed over 18 months (Figures 1A and 1B). The patient reported an expansive lesion in the left temporal region 4 years prior and underwent surgical exeresis in another service in November 2009, with an anatomopathological diagnosis of lipoma.
 Figure 1. A:
Figure 1. A: Subcutaneous tumor with an 18-month progression. Tumor recurrence in the temporal region with incomplete resection performed at another service.
B: Pre-capillary temporal scar from a previous resection surgery.
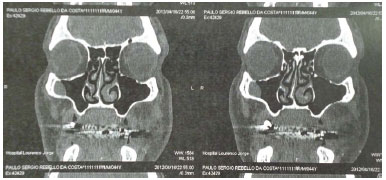
A nuclear magnetic resonance imaging examination after the first excision showed an expansive lobulated lesion with regular contours in the temporal and left infratemporal fossa and a hypersignal in the T1 and T2 and cleavage planes with adjacent structures that was suggestive of lipoma (Figure 2).
 Figure 2.
Figure 2. Preoperative magnetic resonance imaging.
A complete preoperative evaluation was performed and surgical treatment was proposed for total lesion excision after explaining possible sequelae, mainly with regard to the facial nerve, to the patient and obtaining the patient's consent. Under general anesthesia, a pre-auricular incision was performed with temporal extension in the posterior boundary of the tumor and inferior extension in the posterior edge of the mandible.
Dissection by plane in the temporal region revealed a fan-shaped encapsulated tumor lesion that was 10 x 10 x 5 cm, was located between the temporal muscle fibers, extended to the infratemporal fossa, and passed below the zygomatic arch (Figures 3A and 3B). The segment located in the face was submuscular, encapsulated, and multilobular, and it measured 10 x 10 x 5 cm. It involved the zygomatic and buccal branches of the facial nerve as well as the parotid duct since it extended to the buccal mucosa.
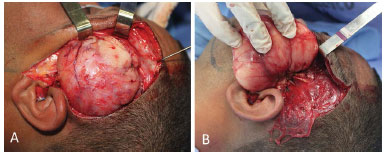 Figure 3. A:
Figure 3. A: Encapsulated and vascularized tumor between the fibers of the temporal muscle.
B: The tumor extends to the face underneath the zygomatic arch.
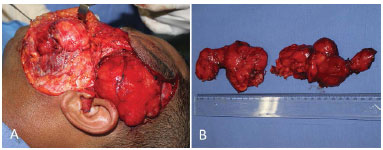
Dissection of the upper and lower segments of the tumor was performed to isolate them from the branches of the facial nerve and parotid duct (Figures 4A and 4B). The upper portion of the tumor was sectioned close to the zygomatic arch to allow for the excision of the rest of the tumor. The surgery was finalized by closure in layers and vacuum drainage.
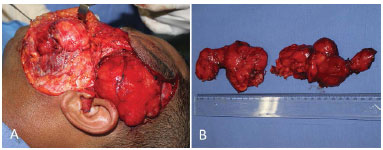 Figure 4. A:
Figure 4. A: Tumor between the layers of the facial muscles and the branches of the facial nerve and parotid duct in continuity with the temporal segment.
B: Resected facial and temporal segments measuring > 10 cm at the largest axis in each portion.
Literature Review
A bibliographic review of English articles in the Pubmed database was performed using the term "lipoma of buccal fat pad" and in the Brazilian Journal of Plastic Surgery using the terms "lipoma of buccal fat pad," "Bichat ball," and "lipoma".
RESULTS
The patient presented with moderate paresis in the left frontal region in the immediate postoperative period that progressively improved during monitoring but featured neuropraxis of the left temporal branch after surgical manipulation (Figures 5A and 5B). The histopathological analysis confirmed the diagnosis of classic lipoma and the tomographic control at 1 month showed only cicatricial changes at the surgical site with no residual lipomatous lesion (Figure 6).
 Figure 5. A:
Figure 5. A: Postoperative 30 days.
B: Barely perceptible scar.
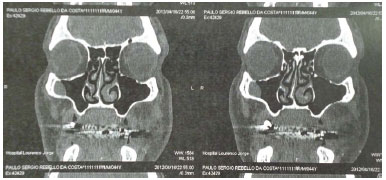 Figure 6.
Figure 6. Postoperative magnetic resonance imaging.
Literature Review
We found no reports in the Brazilian Journal of Plastic Surgery. In Pubmed, 18 articles were found, only three of which detailed lipoma from the buccal fat pad1-4. One article in Portuguese was published in the Brazilian Journal of Maxillo-Facial Surgery. Other articles included six on intraoral lipomas or of the oral mucosa5-10, four on pseudolipoma or post-traumatic hernia11-14, one on hypertrophy by HIV15, one on lipoma of the parotid gland16, one on using the buccal fat pad in reconstructive surgery of the face17, and two on anatomic description18,19.
Anatomy of the buccal fat pad
The buccal fat pad was first described by Heister in 1727, but Bichat described its lipid nature in 1801. This structure is located in the space between the chewing muscles, separating them from each other and the adjacent bone structures3,4; however, it is much larger and more complex than assumed.
Anatomically, the structure is large, well organized, and located between the masseter and buccinator muscles. In accordance with the capsular, ligament, and vascular network formation characteristics, the buccal fat pad is divided into anterior, intermediate, and posterior lobes, the latter of which is divided into four segments.
Each lobe is coated with an independent membrane and each segment is nourished by different vascular pedicles (Figure 7). The anterior lobe is located below the zygomatic arch and extends over the buccinator muscle and maxilla below the lifter of the upper lip and the greater zygomatic muscle. The intermediate lobe is located between the anterior and posterior lobes, resting laterally over the maxilla. The posterior segment of the buccal fat pad is in the masticatory space and extendes to the infraorbital fissure, the space around the temporal muscle, and the ramus of the mandible.
 Figure 7.
Figure 7. Anatomy of the buccal fat pad. 1) Anterior lobe; 2) oral process; 3) intermediate lobe; 4) temporal process, superficial part; 5) parotid; 6) parotid duct.
Its ramifications give rise to buccal, pterygopalatine, pterygoid, and temporal processes. The buccal process represents the lower portion of the posterior lobe below the parotid duct. The extension that extends to the pterygopalatine fossa is called the pterygopalatine process. The pterygoid process is the most posterior segment, filling the pterygomandibular space. The temporal region houses the temporal process, which can be divided into superficial and deep parts.
The superficial segment is located between the deep temporal fascia and the temporal muscle and presents as a continuity with the deep segment, which lies on the wall of the orbit and the frontal process of the zygomatic bone.
Histopathology of the buccal fat pad
Its embryological origin is suspected to be ectodermic unlike the subcutaneous adipose tissue in its anatomy and physiology4. Several pathologies originate from this structure, such as lipoma, lipoblastomatosis, liposarcoma, hemangioma, arteriovenous malformation, and nodular fasciitis other than pseudolipoma, which is a herniation of the fat pad, generally from trauma3,4.
The expansive lesions of the buccal fat pad can be classified as follows according to their histological type: simple/classic lipomas, fibrolipoma, angiolipoma, and fusiform cell lipomas3,4. This last histological variety can represent up to 50% of the lesions reported and its differentiation from well-differentiated liposarcoma can be quite difficult in some cases3,4.
Simple/classic lipoma, found in the described case, is responsible for the other half of the findings. It may present various dimensions when reaching large proportions (> 10 cm in one of its planes), at which it is called a giant lipoma.
These lesions are considered rare and, in this situation, it is of utmost importance to consider a differential diagnosis of liposarcoma and other soft tissue tumors, due to their close relationship with lesion size. Malignant transformation is uncommon and should be suspected in rapidly growing recurring tumors with skin ulcerations3,4.
Treatment of tumors of the buccal fat pad
The treatment is surgical, and access depends on tumor extension. An intraoral incision can be used to approach the lesion and the buccal extension. In cases of diffusely growing tumors, giant lipomas, recurrences, or suspicion of liposarcoma, cutaneous access with temporal and mandibular prolongation is recommended4.
No postoperative complications were found in the literature. De Wijn et al.4 reported 27 cases of tumors in their literature review, the diameters of which were 1-8 cm, including one case of relapse due to fusiform cell lipoma.
DISCUSSION
In this case, cutaneous access was preferred due to familiarity with the facial dissection, diffuse temporal and facial extension of the tumor, and the recurrent nature of the disease. The perioperative findings of the case highlight the characteristics of being well-vascularized, encapsulated, and with global hypertrophy, occupying the intermuscular space from the zygomatic arch to the edge of the mandible in the face with the temporal process involving the entire temporal muscle.
Pathological examination confirmed the nature of a simple lipoma; in terms of size, it was a rare giant lipoma of the buccal fat pad. The recurrence was probably a result of incomplete exeresis of the first resection. All anatomical characteristics, histopathological findings, and the surgical approach and results are in agreement with those reported in the scarce literature.
Due to various possible forms of presentation, depending on the degree of hypertrophy of each lobe and process, of the different histological compositions, many reports were published with other terms and classifications. The anatomical complexity of the face and the buccal fat pad itself may lead to interpretation errors20-23. Kakudo et al.1 called their two cases "halter lipoma" originating from the "masticatory adipose cushion"1. Pyon et al.22 reported eight cases of facial lipoma removed by endoscopy, of which five were localized below the SMAS with probable origin in the buccal pad. Assis et al.23 reported a case of facial lipoma removed by intraoral access, located below the buccinator muscle, the description of which suggests a buccal fat pad lipoma.
CONCLUSION
In bulky tumoral lesions or tumor recurrences of the face, cutaneous access allows a better approach of all facial structures with the possibility of cranial and caudal extension that permits complete tumor excision. The origin in the buccal fat pad should always be considered in lipomatous lesions of the face. The differential diagnosis with lipoma of fusiform cells and liposarcoma should be performed. Imaging exams are important in the detection of their nature and anatomic extension. Although rare, malignant transformation is closely related to lesion size, and its clinical and histological differentiation is quite difficult.
The buccal fat pad is an anatomically and functionally complex structure that lacks full clarification. The literature is poor and confusing, and the articles to date have been published by dental surgeons and various other medical surgical specialists. The incidence of DFSP is probably underestimated, and a large surgical and pathological anatomical study is necessary to standardize its pathology since the majority of lipomatous lesions of the face and mouth published to date probably have the same origin in the buccal fat pad.
REFERENCES
1. Kakudo N, Kusumoto K, Takemoto T, Tanaka Y, Kurokawa I, Ogawa Y. Dumbbell-formed lipomas under the zygomatic arch. J Plast Reconstr Aesthet Surg. 2008;61(1):107-10. PMID: 18068659 DOI: http://dx.doi.org/10.1016/j.bjps.2006.06.011
2. Salvatore C, Antonio B, Del Vecchio W, Lanza A, Tartaro G, Giuseppe C. Giant infiltrating lipoma of the face: CT and MR imaging findings. AJNR Am J Neuroradiol. 2003;24(2):283-6.
3. Brucoli M, Arcuri F, Borello G, Benech A. Surgical technique of the transoral approach to remove a lipoma of the buccal fat pad. J Craniofac Surg. 2011;22(6):2415-8. DOI: http://dx.doi.org/10.1097/SCS.0b013e318231fe2b
4. de Wijn RS, van der Heijden EP, Kon M. On lipoma of the buccal fat pad: report of two cases and review of the literature. J Plast Reconstr Aesthet Surg. 2009;62(1):28-35. PMID: 18249050 DOI: http://dx.doi.org/10.1016/j.bjps.2007.11.022
5. Khubchandani M, Thosar NR, Bahadure RN, Baliga MS, Gaikwad RN. Fibrolipoma of buccal mucosa. Contemp Clin Dent. 2012;3(Suppl 1):S112-4. DOI: http://dx.doi.org/10.4103/0976-237X.95119
6. Kaur R, Kler S, Bhullar A. Intraoral lipoma: report of 3 cases. Dent Res J (Isfahan). 2011;8(1):48-51.
7. Allon I, Aballo S, Dayan D, Vered M. Lipomatous tumors of the oral mucosa: histomorphological, histochemical and immunohistochemical features. Acta Histochem. 2011;113(8):803-9. PMID: 21376375 DOI: http://dx.doi.org/10.1016/j.acthis.2010.11.010
8. de Castro AL, de Castro EV, Felipini RC, Ribeiro AC, Soubhia AM. Osteolipoma of the buccal mucosa. Med Oral Patol Oral Cir Bucal. 2010;15(2):e347-9. DOI: http://dx.doi.org/10.4317/medoral.15.e347
9. Scariot R, Giovanini AF, Torres-Pereira CC, Piazzetta CM, Costa DJ, Rebellato NL, et al. Massive growth of an intraoral lipoma. J Contemp Dent Pract. 2008;9(7):115-21.
10. Epivatianos A, Markopoulos AK, Papanayotou P. Benign tumors of adipose tissue of the oral cavity: a clinicopathologic study of 13 cases. J Oral Maxillofac Surg. 2000;58(10):1113-7. DOI: http://dx.doi.org/10.1053/joms.2000.9568
11. Gadhia K, Rehman K, Williams RW, Sharp I. Traumatic pseudolipoma: herniation of buccal fat pad, a report of two cases. Int J Oral Maxillofac Surg. 2009;38(6):694-6. DOI: http://dx.doi.org/10.1016/j.ijom.2008.12.017
12. Takasaki K, Kihara C, Enatsu K, Kumagami H, Takahashi H. Traumatic pseudolipoma of the buccal fat pad. Otolaryngol Head Neck Surg. 2007;136(5):858-9. PMID: 17478232 DOI: http://dx.doi.org/10.1016/j.otohns.2006.11.004
13. Ribas Mde O, Martins WD, de Sousa MH, Braga AM. Traumatic pseudolipoma of the oral cavity: report of a case. J Contemp Dent Pract. 2006;7(4):89-97.
14. Brooke RI. Traumatic herniation of buccal pad of fat (traumatic pseudolipoma). A review. Oral Surg Oral Med Oral Pathol. 1978;45(5):689-91. PMID: 353625 DOI: http://dx.doi.org/10.1016/0030-4220(78)90141-X
15. Rotunda AM, Jones DH. Human immunodeficiency virus-associated lipohypertrophy (buccal fat pad lipoma-like lesions) reduced with subcutaneously injected sodium deoxycholate. Dermatol Surg. 2010;36(8):1348-54.
16. Kim DS, Kwon H, You G, Jung SN. Surgical treatment of a giant lipoma in the parotid gland. J Craniofac Surg. 2009;20(5):1601-2. DOI: http://dx.doi.org/10.1097/SCS.0b013e3181b1464e
17. Conley J, Angel MF. Surgery on the buccal fat pad in masseter transfer. Arch Otolaryngol Head Neck Surg. 1988;114(3):287-90. PMID: 3342121 DOI: http://dx.doi.org/10.1001/archotol.1988.01860150069017
18. Yousuf S, Tubbs RS, Wartmann CT, Kapos T, Cohen-Gadol AA, Loukas M. A review of the gross anatomy, functions, pathology, and clinical uses of the buccal fat pad. Surg Radiol Anat. 2010;32(5):427-36. DOI: http://dx.doi.org/10.1007/s00276-009-0596-6
19. Dubin B, Jackson IT, Halim A, Triplett WW, Ferreira M. Anatomy of the buccal fat pad and its clinical significance. Plast Reconstr Surg. 1989;83(2):257-64. PMID: 2911625 DOI: http://dx.doi.org/10.1097/00006534-198902000-00009
20. Zhang HM, Yan YP, Qi KM, Wang JQ, Liu ZF. Anatomical structure of the buccal fat pad and its clinical adaptations. Plast Reconstr Surg. 2002;109(7):2509-18. DOI: http://dx.doi.org/10.1097/00006534-200206000-00052
21. Piattelli A, Fioroni M, Rubini C. Intramuscular lipoma of the cheek: a case report. J Oral Maxillofac Surg. 2000;58(7):817-9. PMID: 10883702 DOI: http://dx.doi.org/10.1053/joms.2000.7281
22. Pyon JK, Park BJ, Mun GH, Cha MK, Lim SY, Bang SI, et al. Endoscopic excision of cheek lipomas. Ann Plast Surg. 2008;61(4):413-8. PMID: 18812713 DOI: http://dx.doi.org/10.1097/SAP.0b013e318168d304
23. Assis GM, Silva SRP, Moraes HM, Amaral JIQ, Germano AR. Lipoma Facial Removido por Acesso Intrabucal: Caso Clínico. Rev Bras Cir Buco-Maxilo-Fac. 2010;10(2):89-93.
1. Sociedade Brasileira de Cirurgia Plástica, Rio de Janeiro, RJ, Brazil
2. Hospital dos Servidores do Estado do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
3. Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil
Institution: Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Chang Yung Chia
Rua Carlos Oswald, 140 bloco 1 apto. 206, Barra da Tijuca
Rio de Janeiro, RJ, Brazil Zip Code 22793-120
E-mail: changplastica@gmail.com
Article received: September 27, 2012.
Article accepted: January 28, 2013.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license