

Original Article - Year 2016 - Volume 31 -
Portuguese translation of Patient and Observer Scar Assessment Scale (POSAS)
Tradução para o português da Patient and Observer Scar Assessment Scale (POSAS)
ABSTRACT
INTRODUCTION: The scar assessment is a useful tool in surgical intervention and other treatments by documenting efficacy and making possible to improve them. There is no record of a standard scale in Portuguese to scar evaluation, and the Patient and Observer Scar Assessment Scale (POSAS) was chosen to translation and validation for having received the best evaluations in reviews, and because it contemplates the patients' perception.
METHODS:We translated the POSAS scale from English to Portuguese. The translation was based on orientations from the World Health Organization, with permission from the main author of the original scale. Before the pre-testing, the translated scale was sent to the authors of the original scale for analysis, and adjusts were made.
RESULTS: The pre-testing version was applied by three examiners in five patients each (n = 15), and difficulties were reported to the authors. No alterations were necessary during the pre-test.
CONCLUSION: In this manuscript, we present the translation process of POSAS, and its validation is now in progress.
Keywords: Translating; Scars; Scales; Processs assessment (Health Care); Outcome assessment (Health Care).
RESUMO
INTRODUÇÃO: A avaliação de cicatrizes é uma ferramenta útil na análise de intervenções cirúrgicas e outros tratamentos, ao documentar sua eficácia e possibilitar avanços. Não há registro de escala padrão em português para avaliação de cicatrizes, e a Patient and Observer Scar Assessment Scale (POSAS) foi escolhida para tradução e validação por ter recebido as melhores avaliações em revisões e por contemplar também a percepção do paciente.
MÉTODOS: Foi realizada a tradução da escala POSAS do inglês para o português. A tradução foi baseada em orientações da Organização Mundial da Saúde com permissão do autor principal da escala original. Antes de realizar o pré-teste, a escala traduzida foi enviada aos autores da escala original para análise, e ajustes foram realizados.
RESULTADOS: A versão para pré-teste foi aplicada por três examinadores em cinco pacientes cada (n = 15), e dificuldades foram relatadas aos autores. Nenhuma alteração foi necessária durante o pré-teste.
CONCLUSÃO: Apresentamos neste artigo o processo de tradução da POSAS, e sua validação está em andamento.
Palavras-chave: Tradução; Cicatriz; Escalas; Avaliação de processos (Cuidados de Saúde); Avaliação de resultados (Cuidados de Saúde).
Scars are fibrous tissues resulting from skin injuries usually because of trauma, burn or surgical procedure. Its presence can lead to cosmetic, psychological and functional alterations in patients who may complain about pain and itching. The scar features depend on its etiology, location, suture technique and treatment of a wound. Factors like age, race and genetic predisposition can also occur1.
Subjective assessment scales, non-invasive and easily handled are considered clinically more useful. A scale is considered appropriate to compare clinical results when it is reliable, viable, consistent, and valid2. Today, there are about five assessment scales using subjective parameters in an objective manner: Vancouver Scar Scale (VSS), Manchester Scar Scale (MSS), Patient and Observer Scar Assessment Scale (POSAS), Visual Analogous Scale (VAS) and Stony Brook Scar Evaluation Scale (SBSES)3.
POSAS was developed by Draaijers et al. in 20034, to give credit to the patient's opinion as an evaluator. Draaijers et al. study showed that POSAS is more consistent and reliable in burn scar assessment than in VSS.
The POSAS' observers section contains parameters (vascularization, pigmentation, thickness, relief and pliability) that were selected after a critical review of scar evaluation tools and clinical experience5. In addition to the observer assessment, patients answer about itching, pain, and four other parameters (color, stiffness, level, irregularity) parallel to the observer assessment. Assessment of patients allows more complete evaluation to compare the single point of view of the observer. The itching parameter was particularly significant for the patient4.
Van de Kar et al.6 included a new parameter to the original POSAS scale: scar surface area. This new parameter was added to the tasks of scale observer, initially with five parameters, which allowed the assessment of contractions or expansions of scar surface area.
The current POSAS scale comprehends, therefore, two scales (Patient and Observer). These scales include six items punctuated numerically. Each one of the six items of both scales is punctuated from one to ten, and ten indicates worst scar or sensation. Total score of both scales consists in the sum of each one of the six items punctuation (ranging from six to 60). The lowest score, six, reflects normal skin, as the highest score, 60, indicates a very high level of tissue alteration, being this latter the worst scar imaginable.
The scar assessment is an useful tool to surgical intervention and other treatments because it efficiently register and give the chance to advance. There is no record of a standard scale in Portuguese to evaluate scars. The POSAS was chosen to be translated and validated because it has the best evaluations in literature reviews2,7, and includes patients' perception.
METHODS
After authors of the scale approval we translated POSAS scale from English into Portuguese. Translation was based on guidelines provided by the World Health Organization (WHO)8. The first version was reviewed by experts in the field (plastic surgeons) who were fluent in English. After analysis and discussion, some pertinent changes were made. The scale in Portuguese was back-translated into English by independent translator, who was not a health professional and was blinded to the original version of the scale. The back-translation was reviewed and compared with the original version of the scale by authors.
The authors of the original scale made observations that were taken in consideration to design the pre-testing version. The scale was then applied in a small sample of patients (n = 15) to assess its practicability. Three examiners, members of our plastic surgery service, who did have previous knowledge of the scale, applied the scale for five individuals each. Examiners were requested to report any difficulty in terms of understand or apply the scale.
Patients were aged 18 years or older and they were assisted at Hospital de Clínicas de Porto Alegre (HCPA). Data were collected in July 2014. All patients signed the consent form. No criteria were used to select scars because the study sought to analyze the understanding of examiners and patients about the scale. The Ethical and Research Committee of the HCPA approved the study.
RESULTS
During the pre-testing examiners reported difficulties seen among patients with very low educational level to understand the scale. Each examiner, A and B, reported this situation with one patient.. These patients with limitations required more time to complete understand questions, which required the examiners to use synonyms to explain what was asked. The remaining patients (87%) did not have such problem. No other problems was identified during the pre-testing. The translated scale is currently under validation (Figures 1 and 2).
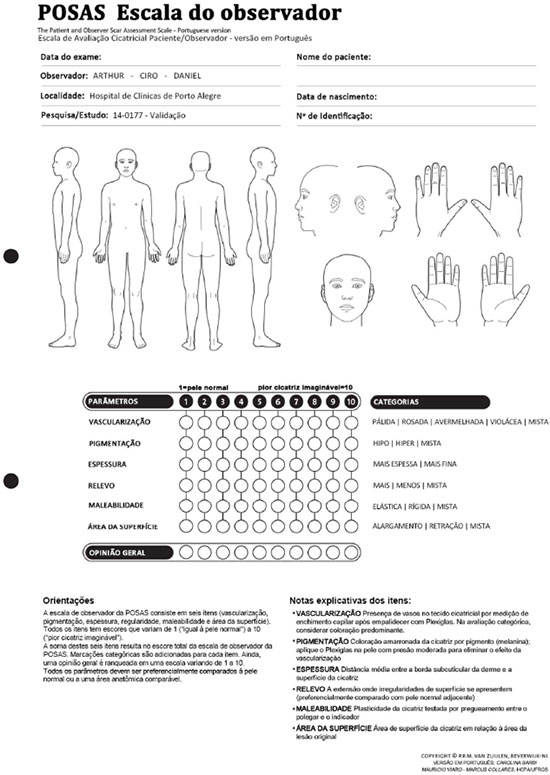
Figure 1. Patient and Observer Scar Assessment Scale - POSAS. Observer scale translated into Portuguese (currently under validation).

Figure 2. Patient and Observer Scar Assessment Scale - POSAS - Patient scale translated into Portuguese (currently under validation).
DISCUSSION
POSAS is a useful tool for assessment of scars after burn injury.4,7 It also presented consistency and applicability for different linear scars2. Reviews have reported that POSAS show adequate internal consistency and good interobserver confidence as this scale was well understood and had better correlation to the patients' estimation compared with VSS.
When scales are exclusively used by health professionals a certain tolerance exist concerning original language used, and for this reason the tool is not always translated. However, when these tests include questions to patients, to translate the questionnaire for patients mother tongue is important to guarantee safety. The translation process of our study is based on guidelines by WHO, but also used references from similar studies in which tests were applied by examiners in order understand patients' knowledge on a given subject/ tool9,10.
Cultural adaptation has a difficult balance to be achieved, i.e., we cannot use terms technical terminology with patients because they probably will not understand, however, but colloquialisms should be avoid because they will be unspecific to convey the message. Therefore, the word "thickness" found in the question "Is the thickness of the scar different from your normal skin at present?" was translated into Portuguese as "altura", which means "height", not into the word "espessura", which means thickeness, because in Portuguese this adaptation seems to facilitate the patient understand and the specificity need to convey the message is maintained.
After discuss with examiners we understood that difficult to understand presented by the two patients (13%) was global due to their very low educational level, but not because of some specific terminology that lead them to not understand questions. For this reason, we decided not to change patients scale. If we make the scale too simple, there is a risk of turning it unspecific and subject to diverse interpretations especially in a country with cultural-linguistic heterogeneity like Brazil. Patients' part in the process was no altered after comparison of the original scale with the back-translation version.
Among the recommended alterations by authors of the original scale is word "Relief", which in our first translation into Portuguese the word "Irregularidade" choice, which means irregularity, and then it was replaced by "Relevo", which means relief. In Explanatory notes on the items the word "Plasticidade" (Suppleness) was used to guide the assessment of "Maleabilidade" (Pliability) and "pregueamento" was a better substitute for wrinkling than "pinçamento", which means pinch.
The different levels of expertise of those who applies the scale may interfere in its comprehension. This limitation was already discussed concerning patients, but it may also occur with the observer. Our examiners were two residents of plastic surgery and one plastic surgeon who has a doctorate in surgery. All examiners had the skills to apply the scale without previous training, by evaluate different scar types. POSAS like all subjective tool present better results depends on the examiners expertise. This interobserver variation can be further evaluated during the validation study.
CONCLUSION
This study developed the Portuguese version of POSAS that gives the possibility to standardize scar assessment in Portuguese language. An evaluation tool in Portuguese was obtained after translation of the original scale in English. This activity improves patient perception especially because the chosen scale is the only one that includes this aspect.
REFERÊNCIAS
1. Deitch EA, Wheelahan TM, Rose MP, Clothier J, Cotter J. Hypertrophic burn scars: analysis of variables. J Trauma. 1983;23(10):895-8. DOI: http://dx.doi.org/10.1097/00005373-198310000-00009
2. Durani P, McGrouther DA, Ferguson MW. Current scales for assessing human scarring: a review. J Plast Reconstr Aesthet Surg. 2009;62(6):713-20. PMID: 19303834 DOI: http://dx.doi.org/10.1016/j.bjps.2009.01.080
3. Fearmonti R, Bond J, Erdmann D, Levinson H. A review of scar scales and scar measuring devices. Eplasty. 2010;10:e43.
4. Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113(7):1960-5. DOI: http://dx.doi.org/10.1097/01.PRS.0000122207.28773.56
5. van Zuijlen PP, Angeles AP, Kreis RW, Bos KE, Middelkoop E. Scar assessment tools: implications for current research. Plast Reconstr Surg. 2002;109(3):1108-22. DOI: http://dx.doi.org/10.1097/00006534-200203000-00052
6. van de Kar AL, Corion LU, Smeulders MJ, Draaijers LJ, van der Horst CM, van Zuijlen PP. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116(2):514-22. PMID: 16079683 DOI: http://dx.doi.org/10.1097/01.prs.0000172982.43599.d6
7. Fearmonti RM, Bond JE, Erdmann D, Levin LS, Pizzo SV, Levinson H. The modified Patient and Observer Scar Assessment Scale: a novel approach to defining pathologic and nonpathologic scarring. Plast Reconstr Surg. 2011;127(1):242-7. PMID: 21200219 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181f959e8
8. World Health Organization. Process of translation and adaptation of instruments [Acesso 3 Ago 2014]. Disponível em: http://www.who.int/substance_abuse/research_tools/translation/en/
9. Sekeff-Sallem FA, Caramelli P, Barbosa ER. Cross-cultural adaptation of the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) to Brazilian Portuguese. Arq Neuropsiquiatr. 2011;69(2B):316-9. PMID: 21625757 DOI: http://dx.doi.org/10.1590/S0004-282X2011000300009
10. Coutinho-Myrrha MA, Dias RC, Fernandes AA, Araújo CG, Hlatky MA, Pereira DG, et al. Duke Activity Status Index for cardiovascular diseases: validation of the Portuguese translation. Arq Bras Cardiol. 2014;102(4):383-90. PMID: 24652056 DOI: http://dx.doi.org/10.5935/abc.20140031
Hospital de Clínicas, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
Institution: Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil.
Corresponding author:
Carolina Barbi Linhares
Rua Ramiro Barcelos, 2350
Porto Alegre, RS, Brazil Zip Code 90035-903
E-mail: cbarbi.cip@gmail.com
Article received: August 4, 2014.
Article accepted: January 25, 2016.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter