

Original Article - Year 2016 - Volume 31 -
Dermatofibrosarcoma protuberans misdiagnosed as keloid and treated with triamcinolone acetonide
Dermatofibrossarcoma protuberante diagnosticado erroneamente como queloide e tratado com acetonido de triancinolona
ABSTRACT
INTRODUCTION: Dermatofibrosarcoma protuberans is a rare skin tumor with intermediate malignancy, low metastatic potential, and high recurrence rates after surgical treatment. Owing to a possible clinical resemblance with hypertrophic scars and keloids, the correct diagnosis is fundamental for treatment success. The objective of the present work is to report on four cases of dermatofibrosarcoma protuberans misdiagnosed as keloid and treated elsewhere with infiltration of triamcinolone acetonide.
METHOD: Between November 1983 and January 2008, four patients with dermatofibrosarcoma protuberans who had undergone intralesional infiltration with triamcinolone acetonide elsewhere were treated because of an erroneous diagnosis of keloid. Radical surgical excision was performed, and 3 cm of healthy tissue was removed from the side margins, including the deep margin, an anatomical structure not infiltrated by the tumor. The patients underwent long-term periodic medical evaluations.
RESULTS: The patients were followed-up for an average of 159 months. Three patients (75%) are still alive without signs of disease at the time of this report. One patient (25%) died of the disease after an attempt to remove the advanced recurrent tumor using extensive craniofacial surgery. Recurrence occurred 7 years after the radical operation.
CONCLUSION: Dermatofibrosarcoma protuberans must be considered in the differential diagnosis of keloids. Intralesional infiltration with triamcinolone acetonide should only be performed after diagnostic confirmation , which may require pathological examination. A careful clinical examination and knowledge of the lesion favor a precise diagnosis and an appropriate treatment.
Keywords: Dermatofibrosarcoma; Keloid; Triamcinolone acetonide; Diagnostic errors.
RESUMO
INTRODUÇÃO: Dermatofibrossarcoma protuberante é um tumor de pele raro e de malignidade intermediária, com baixo potencial metastático, mas altas taxas de recorrência após tratamento cirúrgico. Por apresentar eventual semelhança clínica com cicatrizes hipertróficas e queloides, o diagnóstico correto mostra-se fundamental para o sucesso do tratamento. O objetivo do presente trabalho é fazer um alerta e relatar quatro casos de dermatofibrossarcoma protuberante erroneamente diagnosticados como queloide e tratados alhures com infiltração de acetonido de triancinolona.
MÉTODO: Entre novembro de 1983 e janeiro de 2008, foram atendidos quatro pacientes com dermatofibrossarcoma protuberante que tinham sido submetidos alhures a infiltrações intralesionais de acetonido de triancinolona, em virtude de diagnóstico errôneo de queloide. Nos quatro casos, foram realizadas excisões cirúrgicas radicais, com remoção de 3 cm de tecido sadio nas margens laterais, incluindo-se, na margem profunda, uma estrutura anatômica não infiltrada pelo tumor. Os pacientes receberam avaliação médica periódica em longo prazo.
RESULTADOS: Os pacientes foram acompanhados por uma média de 159 meses. Três pacientes (75%) permaneceram vivos, sem sinais de doença em atividade. Um paciente (25%) faleceu devido à doença, após tentativa de remover o avançado tumor recorrente, por meio de extensa cirurgia craniofacial. A recidiva ocorreu sete anos após a operação radical.
CONCLUSÃO: Dermatofibrossarcoma protuberante deve ser considerado no diagnóstico diferencial dos queloides. A infiltração intralesional de acetonido de triancinolona só deverá ser realizada após diagnóstico de certeza, que pode demandar exame anatomopatológico prévio. Um exame clínico cuidadoso e o conhecimento da lesão favorecem um diagnóstico preciso e, portanto, um tratamento adequado.
Palavras-chave: Dermatofibrossarcoma; Queloide; Triancinolona Acetonida; Erros de diagnóstico.
Dermatofibrosarcoma protuberans (DFSP) is a rare indolent cutaneous neoplasm with low metastasis rates despite aggressive local and recurrent behavior1,2. DFSP occurs most often in individuals between the third and fourth decades of life and has a slight predominance in the male sex1. The regions most affected by the injury include the torso, followed by the lower limbs and the head and neck1-5.
Clinically, this neoplasm initially manifests as a firm skin plate that causes one or more nodules that create a protruding appearance. Its progression is slow and the tumor itself may have a reddish or brownish discoloration1,2. Often, the neoplasm resembles a keloid2,6 and can manifest as an atrophic lesion similar to circumscribed scleroderma1.
The diagnosis is made based on clinical suspicion and confirmed by using the results of pathological examinations. Making the clinical diagnosis in childhood, however, is difficult because of possibly confusing the tumor with a cutaneous vascular malformation1.
The recommended treatment is eminently surgical, consisting of the enlarged excision of the lesion with large lateral margins of healthy tissue. Mohs micrographic surgery is also performed, although the studies regarding the results with this technique are compromised by bias7,8.
Although scarce and indolent, the tumor may affect noble areas, and owing to its recurring nature, it may result in significant deformities. Given the clinical resemblance of DFSP with keloid and the possibility of an erroneous diagnosis between the two entities9, it is fundamental for the professional to be familiar with this condition to enable the determination of the precise nature of the tumor and the establishment of an effective treatment.
OBJECTIVE
The objective of the present work is to report on four cases of DFSP misdiagnosed as keloid and treated with infiltration of triamcinolone acetonide.
METHOD
Data of four patients with five DFSP treated between November 1983 and January 2008 were reviewed, including patient sex and age, tumor location, and surgical technique and findings.
All patients underwent surgery and were followed-up postoperatively in the Plastic Surgery Clinic of the Felício Rocho Hospital (Belo Horizonte, MG, Brazil). The surgical technique consisted of enlarged resection with lateral 3-cm margins of healthy tissue. The deep margin included a non-infiltrated anatomical structure, such as fascia, muscle, or an outer bone blade. All patients underwent immediate reconstruction using grafts or skin flaps.
The patients were followed-up by clinical examination every 4 months during the first 2 years and every 6 months until the fifth year. The individuals were encouraged to attend an annual medical consultation indefinitely. Those who could not attend the consultation were followed-up by postal mail, e-mail, or telephone call.
All surgical specimens were examined at the Department of Pathology of the same institution. All samples were subjected to hematoxylin-eosin staining, while two were studied immunohistochemically.
Data were entered in a Microsoft Office Excel spreadsheet (Microsoft, 2007). The related literature was reviewed using the terms dermatofibrosarcoma, keloid, triamcinolone acetonide, and diagnostic errors as keywords and descriptors.
This retrospective study was approved by the Research Ethics Committee of the Felício Rocho Hospital (protocol number 166/06).
RESULTS
Four patients were studied, including two (50%) men and two (50%) women (male/female ratio, 1:1). The patients' ages at the time of surgery were 38-57 years (mean, 49 years). Two (40%) lesions were in the head, one (20%) was in the neck, and one (40%) was in the torso.
The patients were followed-up for an average of 159 months. Three patients (75%) remained alive without signs of disease. One patient (25%) died of disease recurrence 7 years after an attempt to remove the recurring advanced tumor by extensive craniofacial surgery.
Case 1
A 55-year-old woman was admitted to the Plastic Surgery Clinic of the Felício Rocho Hospital in 1983 with a previous history of an automobile accident and the treatment of facial and cervical scars by a plastic surgeon. She presented with recurrent lesions in the right lateral cervical region that had developed over a 6-year period and a misdiagnosis of keloid, without biopsy, and was treated with intralesional infiltration of triamcinolone acetonide and surgical resection (Figure 1). A biopsy performed after admission to our service confirmed the clinical diagnosis of DFSP. In November 1983, wide tumor resection was performed with 3-cm lateral margins, inclusion of the cervical fascia in the deep margin, and reconstruction with a skin graft (Figure 2). Clinical follow-up in November 2009 showed no residual tumor or recurrence for a total of 310 months.

Figure 1. Case 1, 55-year-old woman. Lesion in the right lateral cervical region. Note the rounded and elevated reddish tumefaction with telangiectasia.

Figure 2. Case 1, 55-year-old woman. Lesion in the right lateral cervical region. Postoperative aspect 2 months after tumor resection and skin grafting.
Case 2
A 57-year-old man was admitted in 1998 with a lesion in the right cheek that had developed over 35 years that was treated prior at another institution. He underwent two biopsies with erroneous diagnoses of fibromatosis and keloid and treated with intralesional triamcinolone acetonide injections in 1980 and 1993. Ten months after the last application, the patient developed nodular lesion in the zygomatic region and lower right eyelid (Figures 3A and 3B), and a biopsy performed in the Plastic Surgery Clinic of the Felício Rocho Hospital confirmed the clinical diagnosis of DFSP. In March 1998, radical surgical excision was performed, followed by reconstruction with a frontal flap and skin graft and finally radiotherapy (Figures 4A, 4B, and 5A). The neoplasm recurred 7 years later, and the patient underwent orbital exenteration in January 2005. In 2007, owing to orbital invasion (Figure 5B), the patient underwent a craniectomy and maxillectomy but died of meningitis.
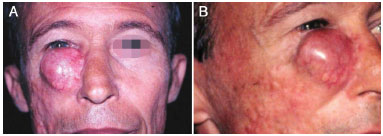
Figure 3. A: Case 2, 57-year-old man. Lesion in the zygomatic region and lower right eyelid. Observe the growth of the protruding aspect, which is reddish and with telangiectasia. B: Lesion on a firm skin plate on the right cheek.
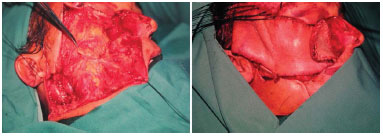
Figure 4. A: Case 2, 57-year-old man. Lesion in the zygomatic region and lower right eyelid. Bloody area after enlarged excision. B: Final aspect in the immediate postoperative period after construction of a frontal flap to cover the skin and a skin graft in the donor area and nasal mucosa.
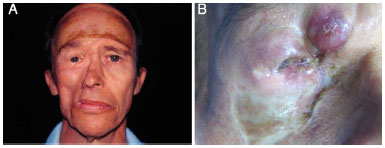
Figure 5. A: Case 2, 57-year-old man. Lesion in the zygomatic region and lower right eyelid. Postoperative aspect 4.5 months after tumor resection and reconstruction with a frontal flap and skin grafting. B: Tumor recurrence 7 years after the initial excision.
Case 3
A 46-year-old man presented with a cutaneous lesion in the left mandibular region for 2 years that was previously treated with intralesional infiltration of triamcinolone acetonide and surgical excision but eventually recurred (Figure 6). In May 2000, he underwent radical tumor resection including the superficial musculoaponeurotic system of the face and part of the orbicularis oris and buccinator muscles as well as the construction of a myocutaneous flap of the platysma muscle (Figures 7A-7C). The patient had a satisfactory postoperative course (Figures 8A and 8B), but an interscapular DFSP emerged 5 months later. In October 2007, the patient underwent enlarged excision of the torso lesion and reconstruction with a skin graft. His last follow-up appointment was in February 2013 (a total of 153 months of follow-up) during which no signs of recurrence were detected.

Figure 6. Case 3, 46-year-old man. Lesion in the left mandibular region. Note the rounded and protuberant formation, reddish and with telangiectasia.

Figure 7. A: Case 3, 46-year-old man. Lesion in the left mandibular region. Bloody area after enlarged excision. B: Preparation of a myocutaneous flap of the platysma muscle. C: Final aspect in the immediate postoperative period.
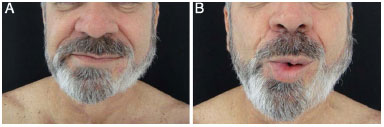
Figure 8. A: Case 3, 46-year-old man. Aspect in the late postoperative period. B: Aspect in the late postoperative period.
Case 4
A 38-year-old woman admitted in January 2008 presented with a history of injury in the infraclavicular region 12 years prior. An erroneous diagnosis of keloid had been made. One year after the lesion was treated elsewhere via surgical resection, local recurrence occurred. Several biopsies were performed, but the results were inconclusive. In 2005, the patient underwent four intralesional applications of triamcinolone acetonide. A biopsy and immunohistochemistry examination conducted in 2007 indicated DFSP. The patient was admitted to the Plastic Surgery Clinic of the Felício Rocho Hospital in January 2008 with several areas of dyschromia induced by the injections (Figures 9A and 9B). Wide tumor excision was performed with 3-cm lateral margins including the greater pectoral muscle fascia in the deep margin (Figure 10A). Reconstruction was performed using a skin flap (Figures 10B and 10C). At the last follow-up appointment in January 2015 (a total of 84 months of follow-up), no signs of tumor recurrence were observed.
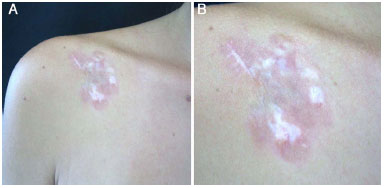
Figure 9. A: Case 4, 38-year-old woman. Lesion in the left infraclavicular region. Note the reddish plate with areas of peripheral dyschromia. B: Detailed view.

Figure 10. A: Case 4, 38-year-old woman. Lesion in the left infraclavicular region. Bloody area after enlarged excision. B: Final aspect in the immediate postoperative period after preparation of the skin flap. C: Final aspect in the immediate postoperative period after preparation of the skin flap.
DISCUSSION
First described by Taylor10 in 1890 in an article entitled "Sarcomatous tumors resembling in some aspects keloid," DFSP is an uncommon cutaneous neoplasia characterized by indolent growth but aggressive local behavior and high rates of recurrence 1,2. The possibility of misdiagnosing DFSP due to possible confusion of this tumor with a keloid has been reported a few times in the literature since then6,7,9.
DFSP presents as a firm pink or purple area of skin surrounded by telangiectasias, similar to a keloid7,10, which justifies any diagnostic confusion7.
The treatment of choice for this neoplasm is surgical, marked by surgical resection, with wide margins, 3-cm lateral margins, and the inclusion of a healthy structure in the deep margin. In a study published by Alves7,8 in 2010 involving a total of 27 patients with DFSP who submitted to an average postoperative follow-up of 115.57 months and operated in the way described, only one case (3.7%) presented with tumor recurrence. This patient's case was similar to case 2 of this report and consisted of an extensive facial lesion misdiagnosed as a keloid and treated with the intralesional injection of triamcinolone acetonide 18 years previously.
The local infiltration of corticosteroid has been used in the therapeutic approach of hypertrophic scars and keloids. The use of triamcinolone acetonide for such a purpose was first described by Murray11 in 1963. In 1974, Manalan et al.9 reported a case of DFSP diagnosed as a keloid and treated with the intralesional injection of that corticosteroid. Twenty-three years later, in an article by Silva Filho et al.6 published in 1997, 20% of a total of 10 patients with DFSP received the topical infiltration of triamcinolone acetonide due to the improper diagnosis. Cases 1 and 2 of this study are part of that group.
The present study reports four cases of DFSP misdiagnosed as keloid and treated elsewhere with the intralesional injection of triamcinolone acetonide. One of these cases involved complications that led to death. Throughout the medical literature researched, only four similar publications were found6-9. Of them, three in previous studies are similar to those reported here6-8.
Corticosteroids exert an immunosuppressant effect and change tissue permeability11; however, the effects of inadvertent topical infiltration on tumor behavior are unknown. In the study by Ogawa et al.12 in 2009 comprising a series of 378 patients with a self-diagnosis of a hypertrophic scar or keloid, four cases (1.06%) were considered misdiagnoses, but none were DFSP. Therefore, biopsies of the lesion are recommended in atypical cases to obtain histological confirmation before the completion of empirical treatments12.
CONCLUSION
DFSP is a rare and indolent cutaneous tumor with aggressive local behavior. Its diagnosis is eminently clinical and confirmed by pathological examination. The treatment is surgical, characterized by an enlarged excision with lateral 3-cm margins and the inclusion of healthy structures within the deep margin.
The present study reported four cases of patients with DFSP who received an erroneous diagnosis of keloid. The patients underwent the intralesional injection of triamcinolone acetonide in other facilities. In one case, the facial tumor became aggressive and the patient died after an attempt to treat the orbital invasion with an enlarged craniectomy.
A careful clinical examination together with knowledge of this type of lesion is essential to a correct diagnosis and appropriate treatment. One should also stress the importance of the precise diagnosis of keloid before therapy, and biopsies should be performed in doubtful cases.
REFERENCES
1. McKee PH, Calonge E, Granter SR. Dermatofibrosarcoma protuberans. In: McKee PH, Calonge E, Granter SR, eds. Pathology of the skin with clinical correlations. 3rd ed. Philadelphia: Elsevier Mosby; 2005. p.1729-35.
2. Shapiro L, Brownstein MH. Dermatofibrosarcoma protuberans. In: Andrade R, Gumport SL, Popkin GL, Rees TD, eds. Cancer of the skin: biology, diagnosis, management. Philadelphia: WB Saunders; 1976. p.1069-78. DOI: http://dx.doi.org/10.1097/00000658-196711000-00011
3. McPeak CJ, Cruz T, Nicastri AD. Dermatofibrosarcoma protuberans: an analysis of 86 cases--five with metastasis. Ann Surg. 1967;166(5):803-16. PMID: 4964386
4. Enzinger FM, Weiss SW. Fibrohistiocytic tumors of intermediate malignancy. In: Enzinger FM, Weiss SW, eds. Soft tissue tumors. 3rd ed. St Louis: Mosby; 1995. p.325-49.
5. Heenan PJ. Tumors of the fibrous tissue involving the skin. In: Elder D, ed. Lever's histopathology of the skin. 8th ed. Philadelphia: Lippincott-Raven; 1997. p.847-87.
6. Silva Filho AF, Andrade Filho JS, Siqueira IMG, Saraiva PS, Magalhães GM, Alves JCRR. Dermatofibrossarcoma protuberante: aspectos clínicos e cirúrgicos. An Bras Dermatol. 1997;72(3):247-51.
7. Alves JCRR, Fonseca RPL, Silva Filho AF, Andrade Filho JS, Araújo IC, Almeida ACM, et al. Ressecção alargada no tratamento do dermatofibrosarcoma protuberante. Rev Bras Cir Plást. 2014;29(3):395-403.
8. Alves JCRR. Tratamento cirúrgico radical do dermatofibrossarcoma protuberante. In: Anais da Academia Mineira de Medicina [Relação de trabalhos aprovados para ingresso como membros titulares]. Belo Horizonte; 2010.
9. Manalan SS, Cohen IK, Theogaraj SD. Dermatofibrosarcoma protuberans or keloid--a warning. Case report. Plast Reconstr Surg. 1974-54(1):96-8. PMID: 4832476
10. Taylor RW. Sarcomatous tumors resembling in some aspects keloid. Arch Dermatol.1890;8:384-7.
11. Murray RD. Kenalog and the treatment of hypertrophied scars and keloids in negroes and whites. Plast Reconstruct Surg. 1963-31:275-80.
12. Ogawa R, Akaishi S, Hyakusoku H. Differential and exclusive diagnosis of diseases that resemble keloids and hypertrophic scars. Ann Plast Surg. 2009;62(6):660-4. PMID: 19461281
1. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
4. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
5. Faculdade de Medicina da Universidade de Itaúna, Itaúna, MG, Brazil
6. Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil
7. Hospital da Polícia Militar de Minas Gerais, Belo Horizonte, MG, Brazil
Institution: Hospital Felício Rocho/Pós Graduação Ciências Médicas - MG (PGCM-MG), Belo Horizonte, MG, Brazil.
Corresponding author:
Erick Horta Portugal
Rua Santa Maria de Itabira, 217, Bairro Sion
Belo Horizonte, MG, Brazil Zip Code 30310-600
E-mail: erickhphp@yahoo.com.br
Article received: June 7, 2015.
Article accepted: January 4, 2016.
Institution: Hospital Felício Rocho/Pós Graduação Ciências Médicas - MG (PGCM-MG), Belo Horizonte, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter