

Original Article - Year 2016 - Volume 31 -
Development and implementation of an anthropometric protocol to evaluate results of otoplasty
Desenvolvimento e aplicação de um protocolo antropométrico para a avaliação de resultados de otoplastia
ABSTRACT
INTRODUCTION: Prominence is the most common deformity of the ear, affecting about 5% of the population. Most reports on otoplasty describe subjective evaluations, and do not provide accurate postoperative assessment or a comparison between techniques. We propose the development and implementation of a specific protocol to evaluate results.
METHOD: A prospective evaluation for a period of one year in patients who underwent bilateral otoplasty was performed, using a technique based on modeling of the cartilage with sutures, and helix-to-mastoid distance measurements at standardized points.
RESULTS: A total of 23 patients with an average age of 17.8 years underwent surgery. Reoperation was performed in 21.7% of the patients or 10.7% of the ears. Nearly 45% of the correction obtained at the upper point and 35% at the middle and lower points were lost in patients who did not undergo reoperation.
CONCLUSIONS: The protocol was easily used and allowed objective evaluation of the preoperative deformity and surgical results. This technique produced results considered adequate and comparable to the literature.
Keywords: Ear cartilage; Ear; External ear; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A proeminência dos pavilhões auriculares é a forma mais comum de deformidade desta estrutura, afetando em torno de 5% da população. A maioria dos trabalhos acerca da cirurgia de otoplastia apresenta avaliações subjetivas, não permitindo apreciar acuradamente os resultados no pós-operatório, bem como dificultando a comparação entre técnicas. Propõe-se o desenvolvimento e aplicação de protocolo específico para avaliação dos resultados.
MÉTODO: Avaliação prospectiva pelo período de um ano de pacientes submetidos à otoplastia bilateral utilizando técnica baseada em modelagem cartilaginosa com suturas, utilizando medidas da distância hélice-mastoide em pontos padronizados.
RESULTADOS: Foram operados 23 pacientes com idade média de 17,8 anos. A incidência de reoperação foi de 21,7% dos pacientes ou 10,7% das orelhas. Houve perda de cerca de 45% da correção obtida no ponto superior e 35% nos pontos médio e inferior nos pacientes não reoperados.
CONCLUSÕES: O protocolo foi de fácil utilização e permitiu a avaliação objetiva tanto da deformidade no pré-operatório quanto dos resultados cirúrgicos. A técnica utilizada produziu resultados considerados adequados e comparáveis aos da literatura.
Palavras-chave: Cartilagem de orelha; Orelha; Orelha externa; Procedimentos cirúrgicos reconstrutivos.
Prominence is the most common deformity of the ear, affecting about 5% of the population1. Although it does not compromise hearing function, there is great psychological impact associated with ear prominence; issues arising from social interaction are an important cause of complaints and a search for treatment2.
The main anatomical findings that characterize ear prominence are turbinate hypertrophy; inadequate formation of the antihelix with obliteration of normal contour, extending to the main portion and upper and lower branches; and lobe protrusion. These findings may occur singly or more commonly in combination, with a range of prominence3.
Although the first attempts to surgically repair the pinna were reported in the sixth century in India, otoplasty for correction of prominent ears was only first used in the nineteenth century, with publication of the first case by Ely in 18814. Since then, numerous techniques have been described, with at least 200 variations5. There are 2 basic techniques: one involving incision or scraping of the cartilage, as described by Luckett6, Stenstrom7, Chongchet8, and Pitanguy et al.9, and another that preserves cartilage and is based on modeling with sutures only, as in studies by Mustardé 10, Furnas11, and Spira12.
Several published case series evaluated the postoperative results obtained with different techniques. However, the majority of reports only described subjective evaluations based on either physical examination by a surgeon, or on patient satisfaction13-17, without accurately evaluating postoperative symmetry or the extent of loss of correction (which is known to occur in the long term); the reports also did not compare techniques18,19.
OBJECTIVE
Since it is difficult to quantify and document preoperative ear prominence, as well as to describe postoperative evolution and surgical outcomes, the present work aims to develop a follow-up protocol based on measurements of the ear that allow objective assessment of the otoplasty technique used.
METHOD
Patients
A total of 23 patients who underwent surgery from June 2012 to June 2013 at the Serviço de Cirurgia Plástica, Hospital de Clínicas at Unicamp, were studied. Patients who completed one year of follow-up and were discharged, or who required reoperation to correct relapses during the follow-up period, were included in the study.
Surgical procedure
All surgeries were performed as an outpatient under local anesthesia. A fusiform retroauricular incision was made, with excision of excess skin. The treatment of the antihelix was performed with 4-0 polypropylene sutures using the points described by Mustardé10. Treatment of the cephaloconchal angle was performed using 4-0 polypropylene concha-mastoid sutures, according to the method of Furnas11. Fusiform partial excision of conchal cartilage was applied in cases in which cartilage hypertrophy was observed on physical examination or at surgery, with excessive resistance to correction and/or obliteration of the acoustic meatus when the corrected cephaloconchal angle was simulated. After excision, the margins of the conchal cartilage were brought together with continuous 4-0 polypropylene suture. Skin closure was performed with intradermal 4-0 nylon. After the procedure, the patient wore an occlusive bandage for 24 hours, followed by the use of an elastic band for 7 days.
Evaluation protocol
The evaluation of ear position was standardized through measurements of distance between the most lateral portion of the helix and the surface of the mastoid region at 3 points - upper, middle, and lower - based on anatomical references, with the patient maintaining a neutral head position and eyes facing front.
The upper point corresponded to the bifurcation level of the antihelix at its superior and inferior branches; the middle point was at the level of the upper border of the acoustic meatus (the porion); and the lower was at the deepest point of the intertragic incisure (Figure 1). All measurements were performed by the author, using a millimeter caliper, with positioning of the depth probe perpendicular to the mastoid surface at the level of the point to be measured (Figure 2).

Figure 1. Standardization of the upper, middle, and lower measurement points according to anatomical references.
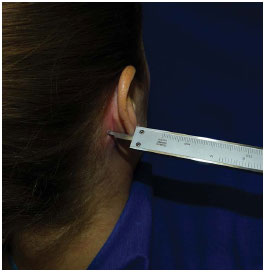
Figure 2. Positioning of the depth-probe caliper perpendicular to the mastoid surface.
Measurements were performed preoperatively, immediate postoperatively (IPO), and on follow-up at 30 days, three months, six months, and one year postoperatively. Reinterventions were indicated when there was loss of correction of the ear protrusion, and were performed at least 6 months after primary surgery.
All patients gave signed informed consent after they agreed to participate in the study. The research protocol was approved by the Committee on Ethics in Research of the Faculty of Medical Sciences, State University of Campinas - Unicamp (Approval no. 15000 of 27/03/2012).
BioEstat 5.0 (Instituto de Desenvolvimento Sustentável Mamirauá, Tefé, Brazil) was used for statistical analysis. Parametric tests were used for comparisons, with Student's t-test for paired and unpaired samples, as indicated for each comparison. An α level of 0.05 was selected. All p values were bilateral.
RESULTS
Of the 23 patients who underwent surgery, 14 (60.9%) were females. The average age was 17.8 years (range 10 to 34). In all patients, Mustardé sutures were used to correct the antihelix (average 2.9 stiches per ear) and Furnas sutures to correct the cephaloconchal angle (average 2 stiches per ear). In 15 patients (65.2%), fusiform partial excision of the conchal cartilage was performed.
Among the patients who underwent surgery, 5 had loss of correction of the prominence in one of the ears, with reintervention being indicated. The incidence of loss of correction requiring reoperation was 21.7% of the patients or 10.7% of the operated ears.
Patients with loss of correction requiring reoperation 6 months after primary surgery were analyzed as a separate group that did not require a second surgery, and did not complete one year of postoperative follow-up.
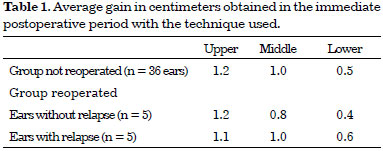
There was no significant difference in the preoperative ear measurements in both groups (intra- and inter-group comparisons). Surgery was able to significantly reduce the measurements at all points, and produced similar results in both ears in the immediate postoperative period (comparisons between measurements in the immediate postoperative period were not significantly different in both groups) (Figures 3 and 4). The average gain in centimeters obtained with the technique used was also comparable between the groups (Table 1).
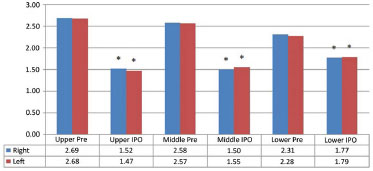
Figure 3. Comparisons between preoperative and immediate postoperative measurements in the group that did not require reoperation. * p < 0.0001 in comparison with respective preoperative values. IPO: immediate postoperatively.
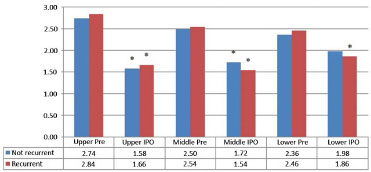
Figure 4. Comparisons between preoperative and immediate postoperative measurements in the group that required reoperation. * p < 0.05 in comparison with respective preoperative values. IPO: immediate postoperatively.
The averages of measurements obtained during postoperative progression in patients who did not undergo reoperation are shown in Figures 5 and 6. Values for patients who required reoperation are shown in Figures 7 and 8.
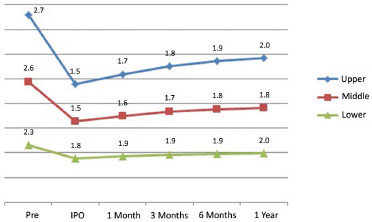
Figure 5. Evolving measurements of the right ear. IPO: immediate postoperatively.
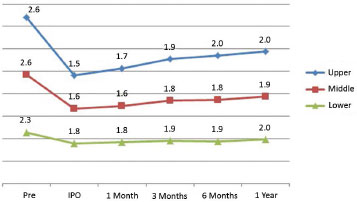
Figure 6. Evolving measurements of the left ear. IPO: immediate postoperatively.
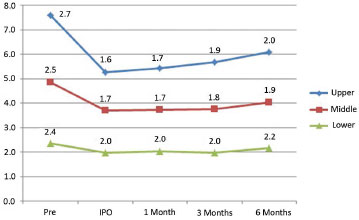
Figure 7. Evolving measurements of the ear without relapse. IPO: immediate postoperatively.
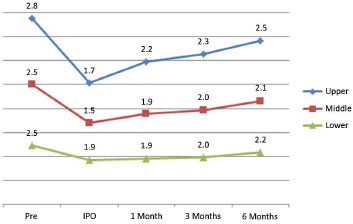
Figure 8. Evolving measurements of the ear with relapse. IPO: immediate postoperatively.
The overall average ear measurements in the group of patients that were not reoperated showed that the loss of correction was progressive at all points during the postoperative evolution, in particular in the first 6 months. In a comparison between measurements at 6 months and one year postoperatively, we observed a significant difference (Figure 9).

Figure 9. Overall evolution of ears in the group that did not need reintervention. * p < 0.0001 vs. immediate postoperative period; # p = 0.0011 vs. immediate postoperative period; § p < 0.05 vs. measurement at 6 months. IPO: immediate postoperatively; PO: postoperative.
The same statistical trend of significant differences was not seen in measurements taken 6 months postoperatively, and in the immediate postoperative period in the group that underwent reoperation, although we also observed an increase in measured values (Figures 7 and 8).
The percentage loss of correction relative to the gain obtained by surgery in ears requiring reoperation was greater as early as the first month postoperatively, especially at the upper and middle points. On the other hand, we observed a late loss of correction at the lower point, at 3 to 6 months postoperatively. Ears that did not require reoperation progressed similar to the group that did not undergo reoperation (Figures 10 to 12).
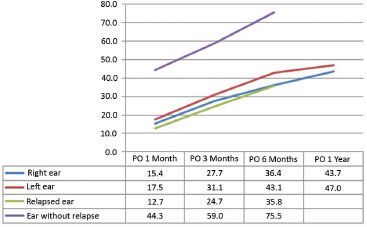
Figure 10. Evolution of the percentage loss of correction obtained at the upper point. PO: Postoperative.
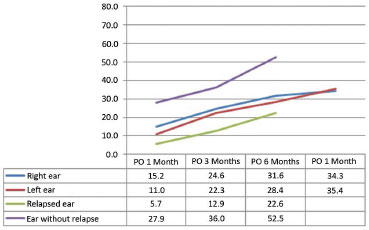
Figure 11. Evolution of the percentage loss of correction obtained at the middle point. PO: postoperative.
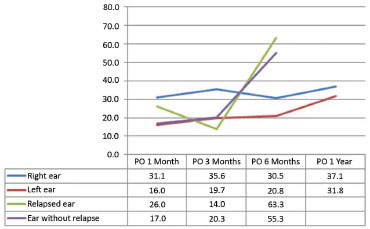
Figure 12. Evolution of the percentage loss of correction obtained at the lower point. PO: postoperative.
The loss of correction observed in the group that did not undergo reoperation indicates that the majority had losses in the range of 25% to 50% of the gain obtained with the procedure at the upper and middle points, and 0 to 25% at the lower point (Figure 13).
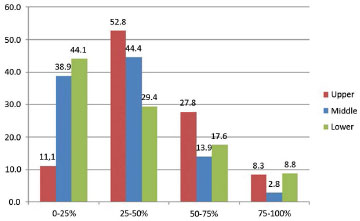
Figure 13. Stratification of the level of loss of correction after one year in the group that was not reoperated.
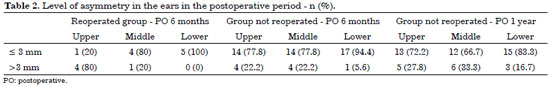
The evaluation of postoperative symmetry shows that the group that did not undergo reoperation had favorable results, with the majority presenting differences up to 3 mm after 6 months or at one year. In contrast, in the reoperated group, all patients presented differences of at least 3 mm at the upper point after 6 months (Table 2).
DISCUSSION
After more than two centuries, otoplasty to correct prominent ears remains controversial, with many variations in technique and widely variable results and complication rates20. Although there is a consensus in regard to the general objectives of surgery20,21, the majority of papers have reported subjective and inconsistent methods of evaluation to compare the form and position of the ear at different time points, and do not allow comparison between techniques22.
The proposed evaluation protocol emerged from the need to evaluate the deformity in the preoperative and postoperative periods in a more objective manner. Measuring the distance between the helix and mastoid region using points at levels defined by anatomical structures was based on the study by Messner and Crysdale23, with modifications of the anatomical references, and with measurement of upper and lower points.
The implementation of the method was simple and practical, taking only a few minutes to obtain the measurements, and only relying on the use of a caliper. Thus, the method is more achievable in daily clinical practice than other methods that are more costly in time and resources despite having possibly greater precision24,25.
The surgical technique used was able to produce the desired anatomical corrections, and reduced the helix-to-mastoid distances at all points. This effect was observed not only in clinical examination but also with measurement, which showed significant reduction in the immediate postoperative period. The gain observed was comparable to that obtained in studies using cartilage suturing techniques, such as those by Adamson et al.26 and Messner and Crysdale23, who obtained gains of 10.3 mm and 10.1 mm at a point that would correspond to the upper level evaluated in our study. Schlegel-Wagner et al.27 and Foda28 obtained reductions of 14 mm and 17 mm, respectively, at the same level in the ear.
However, different approaches were used, such as previous scraping of the antihelix cartilage27 and deliberate overcorrection28. At the middle point, a reduction of 1 cm was obtained, comparable to the studies by Messner and Crysdale (9.9 mm) and Foda (10.5 mm). The only work in which the measurement was comparable to the lower point was the study by Messner and Crysdale, with a correction of 5.8 mm, less than that obtained in our study. The remaining protocols27,28 did not evaluate points of measurement compatible with the lower point in our study, and we were not able to perform comparisons.
During the postoperative period, there was progressive loss of the correction obtained at all points of measurement. The loss was significant until the end of the evaluation period of one year in the group that did not undergo reoperation. In a comparison of our data with other studies performed with similar methodology, we observed a loss at 6 months postoperatively, similar to that by Foda (33.9% loss at the upper point and 26.9% at the middle point).
The remaining studies showed results from different times of evaluation. Adamson et al.26 reported measurements at an average interval of 6 months postoperatively, with loss of 45% of the correction at the level equivalent to the upper point. However, the follow-up time ranged from one to 24 months, in contrast to our evaluation. After a follow-up average of 3.7 years, Messner and Crysdale23 reported losses of correction of 58% at the upper point and 45% at the middle, slightly higher than the values obtained here. Schlegel-Wagner et al.27 showed lower losses of around 23% after an average of 6.25 years postoperatively at the level equivalent to the upper point.
It is clear from the data that there is loss of correction over time using techniques of cartilage modeling with sutures. In comparisons, it should be highlighted that there is a difference in regard to the age group of the population under study, despite similarity in the pattern of loss of correction. In 4 studies discussed23,26-28, the average age of the patients was 11 years, with the majority being children aged 6 to 8 years. Therefore, we observed that the pattern of evolution of operated ears is similar in children and young adults.
By comparing the evolving patterns of loss of correction between reoperated ears and those not reoperated (Figures 10 to 12), we observed loss as early as after one month. This early loss suggests a failure in the Mustardé and/or Furnas stiches in maintaining adequate positioning of the cartilage. A factor that could partly explain such an occurrence is the higher average age of patients that progressed to the need for reoperation (24.2 years in the reoperation group vs. 16 years in the group not reoperated).
It is known that cartilage progressively loses its flexibility with aging, making it more resistant to repositioning. It is not possible to draw definite conclusions from the small number of patients that progressed to the need for reoperation, and assessments with a greater number of cases would be required to correctly evaluate the influence of age on the loss of correction.
The final result of the surgeries in the group that was not reoperated may be considered satisfactory compared to previously established criteria. The most cited guideline of objectives in otoplasty is the study by McDowell21, who established intervals considered optimal for distance between the external border of the helix and the mastoid region. The distances reported are 10-12 mm at the upper point, 16-18 mm at the middle third, and 20-22 mm at the lower third. Adamson et al.29 report that 2 cm should be the limit of normal distance between the mastoid region and the "upper portion of the helix," but a more accurate anatomical reference for this location is not given in the study.
By comparing the measurements of the group that was not reoperated after an interval of one year (Figure 9), we observed that only the upper point differed from that described by McDowell, which is probably because the measurements were performed using different anatomical references. If we consider the measurement performed by Adamson et al., the results would still be within normal range. The final measurements of reoperated ears (Figure 8) have values at upper and middle points greater than any of the criteria reported. It should be noted that McDowell does not describe where the measurements were taken, and Adamson et al. used a population without clearly identified ethnic origin.
Since it is difficult to accurately characterize and differentiate measurements of the prominent ear and the ear considered normal30, standardization of the objective measurements to be achieved by surgery should be based on an analysis of the local population. Thus, we emphasize the need for Brazilian studies on ear anthropometry with better comparison standards.
To improve technique for stabilization of results and reduction of asymmetry and severe loss of correction (in particular in the upper portion of the ear), we suggest use of previous scraping of the antihelix cartilage. Overcorrection suggested by some authors23,28 does not seem to be the best alternative, since there is a risk of inducing excessive permanent correction in some patients, and progression to lower level losses (Figure 13). There are indications that modeling of the cartilage with sutures and previous scraping of cartilage may act synergistically, reducing the loss of correction in the long term27,31 at the topographic regions with the highest losses observed in our study.
CONCLUSIONS
The otoplasty technique used showed favorable results, with progression comparable to studies in the literature. However, previous scraping of cartilage in the topography of the antihelix as a procedure in otoplasty to reduce the loss of correction is suggested.
The evaluation protocol applied was easy to use and allowed objective characterization of a preoperative deformity, as well as evaluation of postoperative evolution and demonstration of the positioning behavior of the ears. The method of evaluation may be useful for future comparisons between techniques.
REFERENCES
1. Petersson RS. Current Trends in Otoplasty. In: Shiffman MA, ed. Advanced Cosmetic Otoplasty. Art, Science, and New Clinical Techniques. 1st ed. Heidelberg: Springer; 2013. p.65-80.
2. Cooper-Hobson G, Jaffe W. The benefits of otoplasty for children: further evidence to satisfy the modern NHS. J Plast Reconstr Aesthet Surg. 2009;62(2):190-4. PMID: 18032121 DOI: http://dx.doi.org/10.1016/j.bjps.2007.09.020
3. Janis JE, Rohrich RJ, Gutowski KA. Otoplasty. Plast Reconstr Surg. 2005;115(4):60e-72e. PMID: 15793433 DOI: http://dx.doi.org/10.1097/01.PRS.0000156218.93855.C9
4. A classic reprint: An operation for prominence of the auricles (with two wood-cuts). By Edward T. Ely. 1881. Aesthetic Plast Surg. 1987;11(2):73-4. DOI: http://dx.doi.org/10.1007/BF01575489
5. Kelley P, Hollier L, Stal S. Otoplasty: evaluation, technique, and review. J Craniofac Surg. 2003;14(5):643-53. DOI: http://dx.doi.org/10.1097/00001665-200309000-00008
6. Rogers BO. The classic reprint. A New Operation for Prominent Ears Based on the Anatomy of the Deformity by William H. Luckett, M.D. (reprinted from Surg. Gynec. & Obst., 10: 635-7, 1910). Plast Reconstr Surg. 1969;43(1):83-6.
7. Stenstroem SJ. A "Natural" technique for correction of congenitally prominent ears. Plast Reconstr Surg. 1963;32:509-18. PMID: 14078273 DOI: http://dx.doi.org/10.1097/00006534-196311000-00003
8. Chongchet V. A method of antihelix reconstruction. Br J Plast Surg. 1963;16:268-72. PMID: 14042756 DOI: http://dx.doi.org/10.1016/S0007-1226(63)80120-4
9. Pitanguy I, Müller P, Piccolo N, Ramalho E, Solinas R. The treatment of prominent ears: a 25-year survey of the island technique. Aesthetic Plast Surg. 1987;11(2):87-93. PMID: 3630840 DOI: http://dx.doi.org/10.1007/BF01575492
10. Mustarde JC. The correction of prominent ears using simple mattress sutures. Br J Plast Surg. 1963;16:170-8. PMID: 13936895 DOI: http://dx.doi.org/10.1016/S0007-1226(63)80100-9
11. Furnas DW. Correction of prominent ears by conchamastoid sutures. Plast Reconstr Surg. 1968;42(3):189-93. PMID: 4878456
12. Spira M. Otoplasty: what I do now--a 30-year perspective. Plast Reconstr Surg. 1999;104(3):834-40.
13. Yugueros P, Friedland JA. Otoplasty: the experience of 100 consecutive patients. Plast Reconstr Surg. 2001;108(4):1045-51. DOI: http://dx.doi.org/10.1097/00006534-200109150-00038
14. Bhatti AZ, Donovan DO. Sutureless otoplasty by scoring of the cartilage: a study in 34 patients. Br J Oral Maxillofac Surg. 2007;45(3):217-20. PMID: 17067729 DOI: http://dx.doi.org/10.1016/j.bjoms.2006.08.004
15. Colpaert SDM, Missotten FEM. Otoplasty for prominent ears: personal technique and review of 150 consecutive cases. Eur J Plast Surg. 2005;28(3):179-85. DOI: http://dx.doi.org/10.1007/s00238-005-0738-y
16. Mahler D. The correction of the prominent ear. Aesthetic Plast Surg. 1986;10(1):29-33. DOI: http://dx.doi.org/10.1007/BF01575264
17. Maricevich P, Gontijo de Amorim NF, Duprat R, Freitas F, Pitanguy I. Island technique for prominent ears: an update of the Ivo Pitanguy clinic experience. Aesthet Surg J. 2011;31(6):623-33. DOI: http://dx.doi.org/10.1177/1090820X11415975
18. Mandal A, Bahia H, Ahmad T, Stewart KJ. Comparison of cartilage scoring and cartilage sparing otoplasty-A study of 203 cases. J Plast Reconstr Aesthet Surg. 2006;59(11):1170-6. DOI: http://dx.doi.org/10.1016/j.bjps.2006.01.055
19. Panettiere P, Marchetti L, Accorsi D, Del Gaudio GA. Otoplasty: a comparison of techniques for antihelical defects treatment. Aesthetic Plast Surg. 2003;27(6):462-5. DOI: http://dx.doi.org/10.1007/s00266-003-3073-3
20. Limandjaja GC, Breugem CC, Mink van der Molen AB, Kon M. Complications of otoplasty: a literature review. J Plast Reconstr Aesthet Surg. 2009;62(1):19-27. PMID: 18952516 DOI: http://dx.doi.org/10.1016/j.bjps.2008.06.043
21. McDowell AJ. Goals in otoplasty for protruding ears. Plast Reconstr Surg. 1968;41(1):17-27. PMID: 5639206 DOI: http://dx.doi.org/10.1097/00006534-196801000-00004
22. Richards SD, Jebreel A, Capper R. Otoplasty: a review of the surgical techniques. Clin Otolaryngol. 2005;30(1):2-8. DOI: http://dx.doi.org/10.1111/j.1365-2273.2004.00939.x
23. Messner AH, Crysdale WS. Otoplasty. Clinical protocol and long-term results. Arch Otolaryngol Head Neck Surg. 1996;122(7):773-7. PMID: 8663953 DOI: http://dx.doi.org/10.1001/archotol.1996.01890190069016
24. Wang B, Dong Y, Zhao Y, Bai S, Wu G. Computed tomography measurement of the auricle in Han population of north China. J Plast Reconstr Aesthet Surg. 2011;64(1):34-40. DOI: http://dx.doi.org/10.1016/j.bjps.2010.03.053
25. da Silva Freitas R, Sanchez ME, Manzotti MS, Baras F, Ono MC, de Oliveira e Cruz GA. Comparing cephaloauricular and scaphaconchal angles in prominent ear patients and control subjects. Aesthetic Plast Surg. 2008;32(4):620-3. PMID: 18414935 DOI: http://dx.doi.org/10.1007/s00266-008-9160-8
26. Adamson PA, McGraw BL, Tropper GJ. Otoplasty: critical review of clinical results. Laryngoscope. 1991;101(8):883-8. PMID: 1865738 DOI: http://dx.doi.org/10.1288/00005537-199108000-00013
27. Schlegel-Wagner C, Pabst G, Müller W, Linder T. Otoplasty using a modified anterior scoring technique: standardized measurements of long-term results. Arch Facial Plast Surg. 2010;12(3):143-8. DOI: http://dx.doi.org/10.1001/archfacial.2010.34
28. Foda HM. Otoplasty: A graduated approach. Aesthetic Plast Surg. 1999;23(6):407-12. DOI: http://dx.doi.org/10.1007/s002669900310
29. Adamson JE, Horton CE, Crawford HH. The growth pattern of the external ear. Plast Reconstr Surg. 1965;36(4):466-70. PMID: 5831865 DOI: http://dx.doi.org/10.1097/00006534-196510000-00008
30. Alexander KS, Stott DJ, Sivakumar B, Kang N. A morphometric study of the human ear. J Plast Reconstr Aesthet Surg. 2011;64(1):41-7. DOI: http://dx.doi.org/10.1016/j.bjps.2010.04.005
31. Tan KH. Long-term survey of prominent ear surgery: a comparison of two methods. Br J Plast Surg. 1986;39(2):270-3. PMID: 3697576 DOI: http://dx.doi.org/10.1016/0007-1226(86)90100-1
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade Estadual de Campinas, Campinas, SP, Brazil
Institution: Faculdade de Ciências Médicas da Universidade Estadual de Campinas, Campinas, SP, Brazil.
Corresponding author:
Davi Reis Calderoni
Rua Tessália Vieira de Camargo, 126, Cidade Universitária "Zeferino Vaz"
Campinas, SP, Brazil Zip Code 13083-887
E-mail: davicalderoni@yahoo.com.br
Article received: July 30, 2014.
Article accepted: November 17, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter