

Articles - Year 2004 - Volume 19 -
Wound Closure by Intraoperative Skin Traction: Analysis of 23 Cases
Fechamento de Feridas por Tração Cutânea Intra-operatória. Análise de 23 Casos
ABSTRACT
The study presents 23 cases submitted to a new and simple technique for closure of skin wounds through cycling and continuous traction of their borders in a short period of time. The technique allows for the primary closure of wounds, avoiding more invasive methods such asgrafts or flaps. The procedure utilizes low-cost material, such as Prolene 2T suture and a slender catheter; in contrast to techniques with the same purpose, but that need specific devices (Sure-ClosureTM) and cost much more. In addition to its low costand ease of use, the procedure may be dane on an outpatient basis, with low rates of complications and morbidity and satisfactory clinical results.
Keywords: Skin; distension; expansion; traction; closure
RESUMO
O presente trabalho apresenta casuística de 23 casos submetidos a uma técnica nova e simples para fechamento de feridas cutâneas através da tração cíclica e contínua de suas margens, em curto período de tempo. A técnica permite o fechamento primário das feridas, evitando procedimentos mais invasivos como enxertos ou retalhos.
O procedimento utiliza material de baixo custo, como fio de Prolene 2TM e um cateter fino, em contraposição a técnicas com finalidade similar que necessitam de aparelhos específicos (Sure-ClosureTM) e com custo diversas vezes maior.
Além do baixo custo e da fácil execução, ela pode ser realizada em caráter ambulatorial, apresentando baixos índices de complicação e morbidade e com bons resultados clínicos.
Palavras-chave: Pele; estiramento; expansão; tração; fechamento
The concept of tissue expansion was initially put imo practice by Neuman(1) in 1956, when he used a round inflatable expander in the retro auricular region. He carried out an intermittent expansion during two months, enabling skin gain. Thereafter, Radovan(2) and other authors began to develop the gradual skin expansion technique.
The process called immediate skin expansion was first described by Gibson(3), and is explained by the mechanical creep phenomenon in which collagen fibers stretch parallel to the direction of the traction force and fundamental substance, made up of mucopolysaccharides and tissue fluids, and when moved leads to an increase in the surface area as the final result(4-7).
The techniques aimed at gaining skin by intraoperative distension, described by Hirshowitz(8), Stough(9), Lam(10), Bjarnesen(11) and others, need specialized equipment to be performed. These devices are not generally available in most hospitals, and are expensive.
We propose a simple wound closure technique by skin traction that allows for primary closure, thus avoiding more invasive procedures such as grafts and flaps. It is a low cost, easy procedure with satisfactory practical results.
METHODS
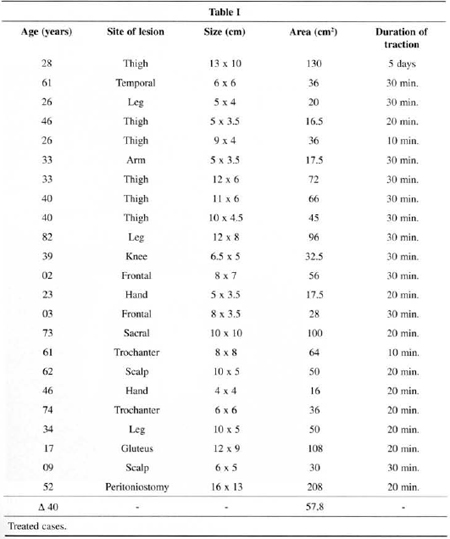
The study presents 20 patients with a total of 23 lesions in need of surgical healing and submitted to primary synthesis after one or multiple skin traction cycles. Ages ranged between 2 and 82 years, with a mean of 40 years. The mean for areas to be closed was 57.8 cm2 and most were in the lower limbs. The number of cycles for each procedure ranged from 1 to 3, and most needed 3 cycles. Data are presented in better detail in Table I. Surgeries were performed in a surgical center using an aseptic technique. Local anesthesia was the most frequently used type of anesthesia. Very large lesions required local-regional block (1 case) or general anesthesia (1 case). The latter was also used in children (2 cases).
The technique consists of rectifying borders, followed by moderately detaching subcutaneous or fasciocutaneous, depending on the location or depth of the wound.
Similar to a "U" suture, the Prolene 2T suture penetrates with a 7.5 cm needle (and not Prolene 2.0TM) in the area posterior to the detachment, and comes out in the interior of the wound, in the direction of the opposite border, where the flap is transfixed at approximately 1 cm from the border; then the suture is covered by a catheter segment, using the needle; to return, the needle penetrates at the end of the detachment and comes out as distant as possible in a nondetached area in order to complete the "U", bilaterally. This step can be observed better in Fig. 1. The length of the catheter per suture, that is, the width of the suture, varies according to the size of the lesion, and is only necessary in the area of greatest tension. Various traction sutures can be associated according to needs, such as in large and/or irregular wounds.
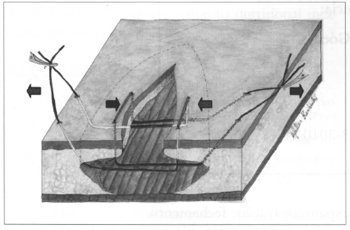
Fig. 1 - The drawing represents the positioning of sutures and direction of traction.
By pulling both sutures on each side simultaneously, in opposite directions, the borders of the lesion are brought together up to a certain point of maximun tension. At this point, the assistant blocks the exits of the sutures dose to the skin using four Kellys in order to maintain the tension (Fig. 2).
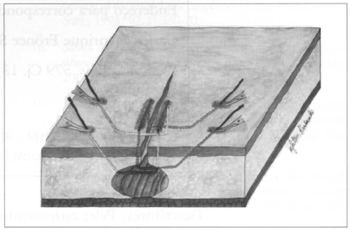
Fig. 2 - After maximum tension is reached, the exit of the suture is clamped dose to the skin.
After 10 minutes, the Kellys are released, the tension is relaxed for 60 seconds and then traction is resumed. At this point, given the skin relaxes because of the previous cycle, the same force applied leads the lesion borders to approach each other more. The cycle (cyclic pressure) is repeated for 1 to 4 cycles (10 minutes each, at 1 minute intervals), until the borders approach each other, allowing suture.
The traction sutures can be used by the assistant to relax and approach the borders during sutures, making the surgeon's work easier. At the end of the procedure, the traction sutures are removed.
The material used for the skin traction costs U$$ 27.
The usual routine care for simple sutures was recommended in the postoperative period and sutures were removed berween the seventh and twenry-first postoperative day,varying according to the region and local conditions.
The postoperative follow-up period ranged between 10 days and 4.5 years.
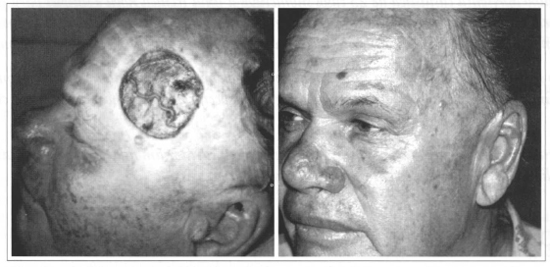
Fig. 3 - A: Immediate postoperative CBC resection at the left fronto temporal region; B: 9th postoperative month of wound dosure utilizing skin traction.
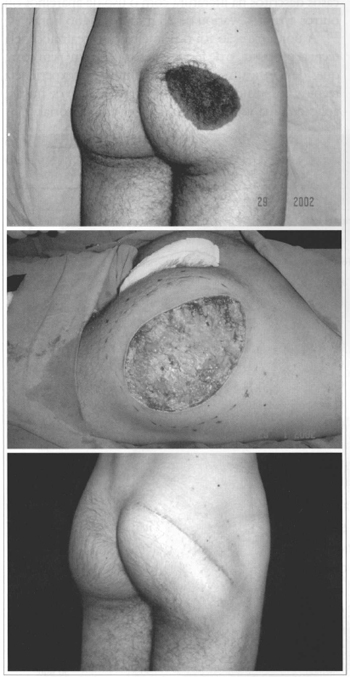
Fig. 4 - A: Preoperative period of a patiem with a congenital gluteus nevus; B: Intraoperative period, before detachment and skin traction; C: 21st postoperative day after suture removal.
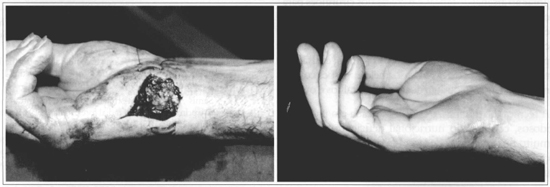
Fig. 5 - A: Traumatic right hand lesion, with substanee loss (positioned traction sutures can be observed); B: 75th postoperative day, with adequate outcome.

Fig. 6 - A: Preoperative period of patient with a peritoniostomy performed 2 months before, and closure required; B: Immediate postoperative period, without the need to maintain traction sutures, even for extensive lesions.
RESULTS
Adequate coaptation of borders was possible in all cases with adequate results at the end of the treatment.
There was one case of total dehiscence that was treated with a skin graft. In another five cases there was partial dehiscence, the largest of which was 0.6 cm by 2.4 cm that healed by second intention, in a maximum period of 21 days.
There was widening of scars in the late postoperative period in three cases. There was one case of sustained alopecia of approximately 2.5 x 4.0 em in the scalp in the late postoperative period (1 year), but without an esthetic sequela, and the patient was satisfied with the result. If necessary the condition may be treated by means of a simple resection of the scar area.
DISCUSSION
Fast distension techniques, when created, took into account the viscoelastic properties of the skin, utilizing continuous and progressive traction. They represem a new concept in wound closure(12-17).
They offer a simple solution for complex wounds in selected cases, and are an alternative to procedures with higher morbidity, such as skins grafts, tissue expanders, local or free flaps(18-21).
The technique described in the present study shortens or prevents hospitalizations, decreasing treatment costs and allowing the patient to return to normal activities early. Vascularization is the limiting factor to skin traction, and the viability of the tegumem may be severely affected if the force is excessive. Thickness, tension of the skin in the detached graft, pale and painful skin are the indicators used by the surgeon to judge how much tension can be applied safely to the borders of the wound. This is where the surgeon's experience and sensitivity influence decisions.
Other techniques utilized with the same objective need devices that are not available in most hospitals, and that need to be requested in advance, ruling out their use in an unexpected situation.
In addition to the difficulties in the availability of traction devices, the mean cost per unit is U$ 250, making the treatment more expensive and making its use unfeasible for lower-income patients. On the other hand, the technique proposed here has an average cost of U$ 27, and the material necessary can be found most hospitals.
Wound closure time using the proposed technique ranged berween 10 and 30 minutes (22 cases). This time ranges between 25 minutes and 456 hours in the cases described in the literature with other equipment or devices(4,10,22). The only exception was the first case performed with the technique proposed, an extensive thigh wound (130 cm2) that due to excessive care and technical inexperience, was sutured after 120 hours (5 days) of traction, applied once a day in an outpatient setting.
Hirshowitz and Stough do not recommend detaching wound borders because it would increase the risk of complications(9-15). Dehiscences, small skin necroses and infections are reported in spite of not detaching(4,15,23), and may also occur in the technique proposed. In experimental studies, Lam and Melis reported that the combination of detachment and external skin traction devices work synergistically in order to attain greater reduction of closure tension, in comparison to each technique alone(10, 23).
The technique proposed allows associating moderate detachment to continuous traction, with a lower risk of complications, because the cutaneous route for irrigating borders is practically intact and the flap is transfixed only in two points. Conversely, techniques that use devices need the introduction of needles or an intradermal Kirschner suture along the full extent of the wound margins connected externally by a traction device(9,13,14), interrupting a substantial part of the skin irrigation route of borders, thus making it indispensable to maintain the subcutaneous route.
The cases with scar widening were due to the positioning of the scar in relation to skin traction lines, as, for example, a vertical direction in two thigh cases and one leg case. The case that progressed with total dehiscence was a patient with a 10 x 5 cm leg wound that was sutured primarily after 20 minutes of traction. It was evolving well up to the 1st postoperative day, when unfortunately the patient began walking normally, and carrying out regular professional activities that demanded intense physical activity, ending in total dehiscence on the 3rd postoperative day.
Wound widening is described in techniques that use devices or other methods(5,11,14,22), although they are esthetically more acceptable than the scars that result from grafts or flaps. Complication rates according to references and the technique praposed are low(6,17,22).
The technique presented is versatile and easy to perform, enabling the surgeon to adjust the traction mechanism to the exact size he wishes, and not limit it to pre-established standards of manufacturers because it is performed with Prolene-2 sutures.
CONCLUSION
This is another valuable alternative to be incorporated imo the armamentarium of tactics and techniques that surgeons can offer for a simple and effective treatment of their patients. It is indicated in various scenarios: traumatic wounds with skin loss; open fasciotomies; peritoniostomies; tumor excisions; skin scar and congenital lesion revisions; closure of a flap harvesting area and others.
However, the technique is not indicated for elderly patients with deficient nutritional status and/or very delicate skin because of the risk of laceration due to traction or total dehiscence due to nutritional incapacity for adequate healing.
REFERENCES
1. Neumann CG. The expansion of an area of skin by progressive distention of a subcutaneous balloon. Plast Reconstr Surg. 1957; 19:124-30.
2. Radovan C. Development of adjacent flaps using a temporary expandable silastic expander. Plast Surg Forum. 1979; 2:62- 4.
3. Gibson T. The physical properties of skin. In J. McCarthy. Plastic Surgery.Vol. 1. Philadelphia: Saunders; 1990. p. 207-20.
4. Alex JC et al. A histologic analysis of three-dimensional versus two-dimensional tissue expansion in rhe model. Laryngoscope. 2001; 111(1):36-43.
5. Molea G et al. Progressive skin extension: clinical and histological evaluation of a modified procedure using Kirschner wires. Br J Plast Surg. 1999; 52:205-8.
6. Wilhelmi BJ et al. Creep vs. stretch: a review of the viscoelastic properties of skin. Ann Plast Surg. 1998; 41(2):215-9.
7. Zhou L et al. Experimental study of the architecrure of skin following tension traction and wound closure]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 1998;12(4):193-6. Chinese.
8. Hirshowitz B et al. Reconstruction of the tip of the nose and ala by load cycling of the nasal skin and harnessing of extra skin. Plast Reconstr Surg. 1986; 77(2):316- 9.
9. Srough DB et al. New devices for scalp reduction. Intraoperative and prolonged scalp extension. Dennatol Surg. 1995; 21(9):777-80.
10. Lam AC et al. Decrease in skin closing tension intraoperatively with surure tension adjustment reei, balloon expansion, and undennining. J Dennatol Surg Oncol. 1994; 20(6):368-71.
11. Bjarnesen JP et al. External tissue stretching for dosing skin defects in 22 patients. Acta Orrhop Scand. 1996; 67(2): 182-4.
12. Armstrong DG et al. Exploiting the viscoelastic properties of pedal skin with the Sure Closure skin stretching device. J Foot Ankle Surg. 1995; 34(3):247-53.
13. Futran ND. Closure of the fibula free flap donor site with the Sure Closure skin stretching device. Laryngoscope. 1996; 106(12):1487-90.
14. Marrero GM et al. An intraoperative skin stretching device to dose wounds in Mohs defects. Dermatol Surg. 1996; 22(6):546-50.
15. Hirshowitz B et al. A skin stretching device for the harnessingof the viscoelastic properties of skin. Plast Reconstr Surg; 1993; 92(2):260-70.
16. Samis AJ et al. Skin-strerching device for intraoperative primary closure of radial forearm flap. Plast Reconstr Surg. 2000; 105(2):698-702.
17. Voy ED et al. Skin expansion screw and skin expandermodern techniques for increasing possibilities in adjacent flap-plasty and defect closure. Handchir Mikroehir Plast Chir. 1998; 30(5):330-3.
18. Armstrong DG et al. 1998 Willian J. Stickel Silver Award. Mechanically assisted, delayed primary closure of diabetic foot wounds. J Am Podiatr Med Assoc. 1998; 88( 10):483- 8.
19. Caruso DM et al. Primary closure of fasciotomy incisions with a skin-stretching device in patients with burn and trauma. J Burn Care Rehabil. 1997; 18(2):125-32.
20. Melis P et al. Primary skin closure of a large groin defect after inguinal lymphadenecromy for penile cancer using a skin stretching device. J Urol. 1998; 159(1):185-7.
21. Ley J et al. Gradual wound closure by dennatotraction of the hand. Handchir Mikroehir Plast Chir. 2001; 33(1):35- 7.
22. Narayanan K et al. Comparative clinical study of the Sure Closure device with conventional wound closure techniques. Ann Plast Surg. 1992; 35(5):485-91.
23. Melis P et al. Tension decrease during skin stretching in undermined versus not undermined skin: an experimental study in piglets.Plast Reconstr Surg, 2001; 107(5):1201-7.
I - Member of the SBCP Assistant of the Instituto de Cirurgia Plástica Santa Cruz, São Paulo - SP. Member of the Plastic Surgery Team of Hospital São Luiz, São Paulo - SP.
II - Member of the SBCP Assistant of the Instituto de Cirurgia Plástica Santa Cruz, São Paulo - SP.
III - Member of the SBCP Director of the Instituto de Cirurgia Plástica Santa Cruz, São Paulo - SP.
Study performed at the Instituto de Cirurgia Plástica Santa Cruz - São Paulo, SP
Address for correspondence:
Carlos Henrique Fröner S. Góes, MD
R. Afonso Brás, 579 Cj. 13
04511-011 - São Paulo - SP Brazil
Phones: (55 11) 3053-3009/3053-3010
e-mail: goescl@terra.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter