

Case Report - Year 2015 - Volume 30 -
Pyoderma gangrenosum in abdominoplasty: a case report
Pioderma gangrenoso em abdominoplastia: relato de caso
ABSTRACT
Pyoderma gangrenosum is a disease characterized by painful ulcers, with imprecise borders of various sizes and depth. The diagnosis is essentially clinical and often exclusionary. The treatment is not specific. Surgical debridement is not indicated because of its potential pathergy. We report a case of pyoderma gangrenosum in a patient who underwent abdominoplasty.
Keywords: Pyoderma gangrenosum; Diagnosis; Treatment, Pathergy; Abdominoplasty.
RESUMO
Pioderma gangrenoso é uma doença caracterizada por úlceras dolorosas, com bordos imprecisos, de diversos tamanhos e profundidade. O diagnóstico é eminentemente clínico, sendo muitas vezes de exclusão. O tratamento não é específico. O desbridamento cirúrgico não é indicado devido a seu potencial de patergia. Neste trabalho, relatamos um caso de pioderma gangrenoso em uma paciente submetida à abdominoplastia.
Palavras-chave: Pioderma gangrenoso; Diagnóstico; Terapêutica; Abdominoplastia.
Pyoderma gangrenosum was first described by Cullen in 1924, and by Brusting et al. in 19301. It is a disease characterized by painful ulcers, with imprecise borders of various sizes and depths. It is a non-neoplastic, non-infectious (infection may occur due to secondary contamination) condition without primary vasculitis2. It is considered an autoimmune disease because epithelial changes lead to immune autophagy causing inflammation and tissue destruction.
The diagnosis is mainly clinical; exclusionary cultures for fungi and bacteria are generally negative, and histopathology is compatible with neutrophilic dermatosis. Pyoderma gangrenosum may appear after trauma or after surgery and can often be confused with surgical wound infection, also known as Cullen's postoperative gangrene3.
The treatment is not specific and surgical debridement is not indicated because of its potential for pathergy. Other therapeutic options such as corticosteroids, immunosuppressants, and immunomodulators are described. Most often the choice of therapy depends on the physician's experience and the patient's clinical condition2,4,5.
This paper reports a case of Pyoderma gangrenosum in a patient undergoing abdominoplasty.
CASE REPORT
Patient aged 36, female, secretary, single, nulliparous, born in Campo Grande, Mato Grosso do Sul, Brazil and resident in Portugal. Sought treatment for plastic surgery in the abdomen. Preoperative testing (laboratory and cardiology) were normal and surgical risk determined to be level 1, and abdominoplasty with liposuction was performed.
Post-operatory antibiotic therapy with cephalothin was introduced and no immediate postoperative complications were observed.
On the second day after surgery there were two painful ecchymoses approximately 5 cm x 1 cm in size in the infra-umbilical area parallel to midline, and the graft showed difficult venous return (Figure 1). Lymphatic drainage was performed on the affected side, but the ecchymoses increased in size.

Figure 1. First day post-surgery.
On the third day post-operative the ecchymosis expanded across the entire infra-umbilical area to the Pfannestiel incision (Figure 2). When infra-umbilical and umbilical sutures were removed, thrombosed vessels were observed throughout practically the entire extension of the adipose tissue in the affected area (Figure 3). Treatment with collagenase ointment was initiated.
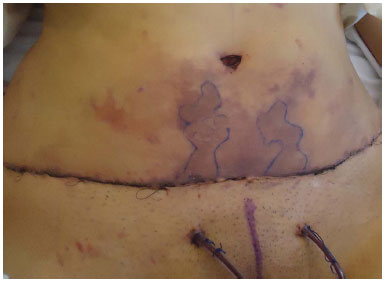
Figure 2. Second day post-surgery.

Figure 3. When infra-umbilical and umbilical sutures were removed.
On the fifth day after surgery, the subcutaneous tissue with necrotic vessels was debrided because of the lack of clinical improvement; only small areas of necrosis on the edges of the skin were debrided, the rest was left intact. Wound treatment with saline and neomycin ointment was continued at the clinic for five days.
On the ninth postoperative day (PO), pyoderma gangrenosum was suspected because of the lack of response to subsequent debridements and increased necrotic area after each debridement. Anatomopathology examination showed subcutaneous tissue with areas of ischemia, necrosis, and hemorrhage.
On the tenth day PO, culture of the abdominal secretion identified Cryseobacterium sp., which is sensitive to ciprofloxacin and oral antibiotic therapy. Ciprofloxacin 500mg every 12 hours and 60 mg/day prednisone were introduced. The wound was rinsed exclusively with saline solution, and debridement was no longer performed.
On the eleventh day PO, laboratory tests were done for cryoglobulins, lupus, anticoagulant, antinuclear antibody, HIV, hepatitis B and C; results for all were negative. Complete blood count (CBC) revealed leukocytosis of 21,000 leukocytes with a shift to the left. Due to significant clinical improvement, prednisone dosage was decreased to 40 mg/day and maintained for 2 days, then dropped to 20 mg/day for 2 days followed by complete withdrawal, and saline rinsing was maintained.
On the twentieth day PO the patient showed significant clinical improvement with virtually no areas of necrotic tissue (Figure 4). However, culture of the abdomen secretion identified Pseudomonas aeruginosa resistant to ciprofloxacin. However, because the CBC did not show leukocytosis nor shift to the left, antibiotic therapy was discontinued, and rising with 1% acetic acid solution 2/ day was initiated.

Figure 4. Twentieth day post-surgery.
Even though on the thirty-third day PO a new culture of the secretion revealed coagulase-negative and chloramphenicol-sensitive Staphylococcus. Because the CBC was normal, antibiotic therapy was not reinitiated but the rinsing regime was halted and aluminum hydroxide bandages were used.
After 7 days a new culture of the abdominal secretion showed no bacterial growth. Given the significant clinical improvement, a new surgical procedure was carried out in order to close the wound (Figure 5).

Figure 5. After a new surgical procedure.
DISCUSSION
Pyoderma gangrenosum is a dermatosis which is difficult to diagnose; it is characterized by necrotic ulcers that are localized mainly in the lower limbs. It affects primarily adults between 20 and 50 years of age, and tends to be more common in females6. Prevalence is estimated to be 1 to 1.5 new cases per 100,000/year. Interestingly, in this present case the pathology occurred in the abdomen, which is not its most common location7.
Although its etiology is not fully understood, it is known that in 50% of cases there is an association of pyoderma gangrenosum with systemic diseases such as inflammatory bowel disease, rheumatic and hematologic diseases. Furthermore, since there is good response to treatment with immunomodulators, an immunological cause is suggested. However, in this case we did not find an association with any systemic diseases2.
This pathology has been described as a postoperative complication in many medical specialties. For example, in plastic surgery it has been reported in patients after breast surgeries, tummy tucks and fasciocutaneous pathwork3.
Further complicating diagnosis, in about 40% of cases of pyoderma gangrenosum develops after some form of trauma. In these cases, the etiology of pyoderma gangrenosum is a pathergy phenomenon, where new and subsequent inflammatory lesions develop in the area of trauma, and are followed by progressive destruction of healthy skin which contraindicates surgical debridement, because this would only worsen these lesions.
Regrettably, because postoperatively the first diagnosis of this kind of lesions is infection of the surgical wound, the correct diagnosis of pyoderma gangrenosum usually becomes more time consuming.
In 2004, Su et al.8 proposed the following diagnostic criteria:
Major criteria
1. Skin ulcer that rapidly becomes necrotic, painful, with an irregular, purple and indeterminate border;
2. Exclusion of other causes of cutaneous ulcers.
Minor criteria
1. History suggestive of pathergy or clinical finding of cribriform scar;
2. Associated systemic disease;
3. The histopathological findings are dermatologically sterile neutrophilic inflammation and mixed lymphocytic vasculitis;
4. Quick response to the use of systemic corticosteroids.
For diagnosis the presence of two major criteria and at least two minor criteria is necessary.
The treatment of pyoderma gangrenosum is based on the use of topical agents to keep the injured area clean and moist. In addition to topical treatment, systemic use of corticosteroids (prednisone or hydrocortisone), immunosuppressants (cyclosporine, cyclophosphamide and thalidomide) and intravenous immunoglobulin is reported to be effective. In general, corticosteroids are the first therapeutic option. If the patient shows serious adverse effects, other therapeutic options are used3,9.
In this case, high doses of prednisone (1-3 mg/kg/ day) were initiated and gradually reduced, as the disease showed improvement. At the end of treatment with immunosuppressive drugs, infection must be excluded3.
Overall, these studies support the findings presented herein. Thus, in this patient significant improvement was observed after initiating use of topical acetic acid to prevent the growth of Cryseobacterium and Pseudomonas, and bandages with aluminum hydroxide to prevent the growth of Staphylococcus, corticosteroids and prednisone therapy, as well as antibiotic therapy with ciprofloxacin because secondary infection in the lesion was detected10.
CONCLUSION
This case report describes a rare disease in an unusual location (abdomen, post-abdominoplasty) and its therapeutic approach, in contrast to the usual approach in cases of skin lesions after abdominoplasty, which would have adversely affected this condition.
Since this pathology may occur as a surgical complication in the post-operatory period, its knowledge is of interest to plastic surgeons because it may lead to early diagnosis, improving therapeutic choices and consequently preventing the appearance of new lesions and worsening of the patient's clinical condition.
REFERENCES
1. Brusting LA, Goeckerman WH, O'Leary PA. Pyoderma (ecthyma) gangrenosum: clinical and experimental observations in 5 cases occurring in adults. Arch Derm Syphilol. 1930;22:655-80.
2. Blitz NM, Rudikoff D. Pyoderma gangrenosum. Mt Sinai J Med. 2001;68(4-5):287-97. PMID: 11514916
3. Meyer TN. Pioderma gangrenoso: grave e mal conhecida complicação da cicatrização. Rev Bras Cir Plást. 2006;21(2):120-4.
4. Serra-Baldrich E, Boixareu MJT. Pioderma gangrenoso: consideraciones. Act Dermatol. 2001;40(2):115-22.
5. Tanus R, Cassol T, D'Aquino Neto V. Pioderma gangrenoso em membro inferior: relato de caso. Arq Catarin Med. 2009;38(Supl 1):70-2.
6. Ruocco E, Sangiuliano S, Gravina AG, Miranda A, Nicoletti G. Pyoderma gangrenosum: an updated review. J Eur Acad Dermatol Venereol. 2009;23(9):1008-17. DOI: http://dx.doi.org/10.1111/j.1468-3083.2009.03199.x
7. Martinez CAR, Priolli DG, Ramos RFB, Nonose R, Schmidt KH. Remissão completa do pioderma gangrenoso após colectomia total em doente portador de retocolite ulcerativa inespecífica. Arq Méd ABC. 2005;30(2):106-10.
8. Su WP, Davis MD, Weenig RH, Powell FC, Perry HO. Pyoderma gangrenosum: clinicopathologic correlation and proposed diagnostic criteria. Int J Dermatol. 2004;43(11):790-800. DOI: http://dx.doi.org/10.1111/j.1365-4632.2004.02128.x
9. Furtado JG, Furtado GB. Pioderma gangrenoso em mastoplastia e abdominoplastia. Rev Bras Cir Plást. 2010;25(4):725-7. DOI: http://dx.doi.org/10.1590/S1983-51752010000400030
10. Sanches TG, Schneider G, Pereira MC, Azevedo LEL, Azevedo GL, Souza MM, et al. Pioderma gangrenoso: relato de caso. Comun Ciênc Saúde. 2006;17(3):237-41.
1. Universidade Federal do Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil
2. Hospital PRONCOR, Campo Grande, MS, Brazil
Institution: Hospital PRONCOR, Campo Grande, MS, Brazil.
Corresponding author:
Suseli Carneiro da Costa
Rua Nove de Julho, 1605
Campo Grande, MS, Brazil Zip Code 79081-050
E-mail: sussaelli@yahoo.com.br
Article received: July 21, 2012.
Article accepted: September 15, 2012.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter