

Original Article - Year 2015 - Volume 30 -
Craniofacial reconstructions: is there still room for locoregional flaps?
Reconstruções craniofaciais: ainda há espaço para os retalhos locorregionais?
ABSTRACT
INTRODUCTION: Advanced tumors of the head and neck still have a high prevalence in Brazil. Reconstructing a defect resulting from a craniofacial resection is a challenge for the plastic surgeon. Free flaps are the first choice for these reconstructions, and locoregional flaps have been used in selected cases. The objective of this study was to evaluate a number of reconstructions with locoregional flaps in patients undergoing craniofacial oncologic resection, to demonstrate the applicability of these flaps and the end result of the reconstructions.
METHODS: We retrospectively studied four craniofacial reconstructions with locoregional flaps on the forehead and scalp. The patients were operated at the Clinical Hospital of the Federal University of Pernambuco. They signed a consent form allowing the scientific publication of their photographs and clinical case records.
RESULTS: All reconstructions were successful. There were no cases of local infection or meningitis, flap necrosis, liquor fistula, or dehiscence. Reconstructions with locoregional flaps were safe and simple to perform for extensive defects in the craniofacial region.
CONCLUSIONS: Plastic surgeons can perform complex reconstructions with locoregional flaps, demonstrating that there is still room for this type of reconstruction.
Keywords: Head and neck neoplasms; Reconstructive surgical procedures; Microsurgery; Face; Plastic surgery.
RESUMO
INTRODUÇÃO: Os tumores avançados de cabeça e pescoço ainda têm elevada prevalência no Brasil. A reconstrução de um defeito resultante de ressecção craniofacial é um desafio para o cirurgião plástico. Os retalhos livres são a primeira escolha para essas reconstruções e os retalhos locorregionais têm sido utilizados em casos selecionados. O objetivo deste estudo é avaliar uma série de reconstruções com retalhos locorregionais em pacientes submetidos a ressecções oncológicas craniofaciais, demonstrando a aplicabilidade desses retalhos e o resultado final das reconstruções.
MÉTODOS: Foram avaliadas, retrospectivamente, quatro reconstruções craniofaciais com retalhos locorregionais de fronte e couro cabeludo. Os pacientes foram operados no Hospital das Clínicas da Universidade Federal de Pernambuco (HC-UFPE) e assinaram termo de consentimento permitindo a publicação científica de suas fotos e casos clínicos.
RESULTADOS: Todas as reconstruções foram bem sucedidas. Não ocorreram casos de infecção local ou meningite, necrose do retalho, fístulas liquóricas ou deiscências. As reconstruções com retalhos locorregionais apresentadas foram seguras e simples para reconstruir defeitos extensos em região craniofacial.
CONCLUSÕES: Os cirurgiões plásticos podem realizar reconstruções complexas com estes retalhos, demonstrando que ainda há espaço para este tipo de reconstrução.
Palavras-chave: Neoplasias de cabeça e pescoço; Procedimentos cirúrgicos reconstrutivos; Microcirurgia; Face; Cirurgia plástica.
Advanced tumors of the head and neck still have a high prevalence in Brazil. The reconstruction of a defect resulting from the resection of an extensive malignant neoplasm in the craniofacial region is a challenge for the plastic surgeon1-4.
Although there are many techniques for repairing these defects, the ideal reconstruction depends on a careful evaluation of each clinical case, with the aim to achieve the best functional and aesthetic results, with minimal morbidity in the donor area and for the patient.
The use of free flaps has become the gold standard for complex reconstructions of the orbitofrontal and parietal regions5,6. However, this type of reconstruction is not performed in most hospitals in Brazil. Thus, knowledge of reconstruction techniques with locoregional flaps for large craniofacial defects is of utmost importance.
Minimizing complications such as liquor fistula and meningitis is a common goal of the team of oncology and plastic surgeons. The flaps used in reconstructions should promote the rapid recovery of patients7.
OBJECTIVE
The objective of this study was to evaluate a series of reconstructions with locoregional flaps in patients undergoing craniofacial oncologic resection, to demonstrate the applicability of these flaps and the final reconstruction results.
METHODS
We retrospectively evaluated four craniofacial reconstructions with locoregional flaps on the forehead and scalp, performed in two patients: three reconstructions in the same male patient (age, 71 years) and one reconstruction in a female patient (age, 58 years).
The first three successive reconstructions in the same patient clearly illustrate the main options of forehead and scalp flaps and, the second case was chosen because it was used as a rescue after the failure of a free flap.
The patients were operated at the Clinical Hospital of the Federal University of Pernambuco (HC-UFPE). They signed a consent form allowing the scientific publication of their photographs and case histories.
After a left hemifrontal resection, which included the frontal bone segment containing a basal cell carcinoma, the male patient was submitted to a first reconstruction with an extended medio-frontal flap (Figures 1 and 2).

Figure 1. (A) Defects of frontal-parietal and frontal bone soft tissues. (B) Final result of the reconstruction with an extended medio-frontal flap (at 6 months).
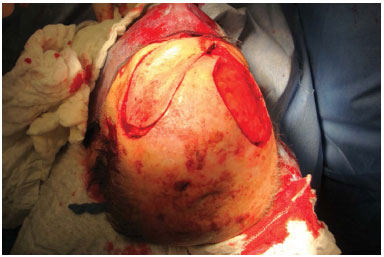
Figure 2. Trans-surgery of the patient in Figure 1, with the extended mediofrontal flap already positioned.
With the recurrence of the lesion, even with postoperative radiotherapy, a second reconstruction was performed after a new resection, which included all previous flaps, with enlargement of the bone and skin defects. Reconstruction was done with a temporal myocutaneous flap, based on the temporal branch of the superficial temporal artery, with skin graft at the donor site (Figures 3 to 5).

Figure 3. Tumor recurrence in the left frontal-parietal region.

Figure 4. Intraoperative image showing bone defects and soft tissue in the frontal-parietal region, including the marking for the temporal-parietal flap.

Figure 5. Temporal-parietal flap at 6 months after surgery. Note the skin graft donor site.
After a new recurrence and a consequent extended tumor resection, the third reconstruction was performed with a temporal-parietal-occipital flap based on the temporal branch of the contralateral superficial temporal artery, associated with the methyl methacrylate plate (Figures 6 and 7). About 4 weeks after this reconstruction, a new procedure was performed for the section of the flap pedicle. The donor area was not grafted because of the need to shorten the surgical time, in consideration of the patient's severe heart disease.

Figure 6. A: Extensive defect of the frontal-parietal and left orbital regions. The reconstructed bone defect is shown, filled with methyl methacrylate. B: Final result after the pedicle section of the temporal-parietal-occipital flap based on right superficial temporal vessels.

Figure 7. Transoperative detail of the temporal-parietal-occipital flap used in the reconstruction shown in Figure 6.
The female patient underwent resection of the orbitofrontal region for a squamous cell carcinoma. The resulting defect was reconstructed with forehead and scalp flaps based on supraorbital/supratrochlear and superficial temporal vessels, respectively, after a failed reconstruction attempt with a free vertical rectus abdominis myocutaneous (VRAM) flap. The donor area healed by secondary intention (Figure 8).

Figure 8. Reconstruction of the frontal-parietal and orbital regions with forehead and temporal parietal flaps after the free flap failure.
All resections were performed by a head and neck surgeon and/or a neurosurgeon, and the reconstructions were performed after obtaining free margins by means of frozen section histopathology.
This work was approved by the research ethics committee of the UFPE under CAAE: 38704414.4.0000.5208.
RESULTS
All flap reconstructions were successful. There were no cases of local infection or meningitis, flap necrosis, liquor fistula, or dehiscence.
Both patients returned to their social life after the reconstructions.
The male patient died in September 2014, 1 year after the third reconstruction operation, due to tumor recurrence and brain compromise.
The female patient was disease free at 2 years after surgery.
The functional results were considered good by the patients and the medical staff; however, the aesthetic result in the female patient was poor.
DISCUSSION
The reconstruction of extensive defects after oncologic resections is a challenge to plastic surgeons, who need preparation and training. These defects may involve the soft tissues in the temporal, parietal, frontal, orbital, and sometimes nasal regions; subjacent bone tissue; meninges; orbit content; and frontal sinus3.
Reconstruction should be done in association with the following objectives: skin-covering restoration of soft tissue and the craniofacial contour, obliteration of dead spaces, and protection of intracranial contents, preventing the occurrence of infections from exposure of the meninges and/or frontal sinus.
In the four reconstructions presented, there were meningeal exposures due to the resected segments of the frontal and/or parietal bone.
Bone loss repair was performed in the third surgery of the first patient due to the resulting extensive bone defect of approximately 30 cm2. In the plastic surgery service, we choose not to use bone grafts or synthetic materials for defects < 10 cm2 or in cases in which the patient will undergo radiotherapy.
Free flaps, in general, offer several advantages for these reconstructions, including the abundance of tissue that is well vascularized, and less damage to the donor site. Recent publications have highlighted these advantages, which are widely disseminated5,6,8. The use of free flaps is the gold standard for reconstructions and should be encouraged in educational centers for specialists.
The success of free flaps and the learning of their manufacture and handling have popularized reconstructions with microvascular anastomosis9,10. Thus, tumors previously considered inoperable can now be resected and reconstructed, allowing the rehabilitation of a wide variety of patients.
Despite these advantages, this type of reconstruction is not lacking in complications or constraints. Total or partial necrosis, resulting in thrombosis or nonperfusion, and systemic complications due to a higher operating time may occur. The failure rate of free flaps varies from 1% to 6%1,3,4,11.
The scalp is relatively inelastic, which makes the use of flaps difficult on this area; however, these flaps can be applied in the reconstruction of large local defects.
The free flaps are based on supratrochlear, supraorbital, superficial temporal, occipital, and posterior auricular vessels. They are safe, reproducible, technically easier to achieve, and not requiring a specialized hospital structure or surgical team that specializes in microsurgery.
The plastic surgery team of HC-UFPE performs reconstruction with free flaps, including craniofacial reconstructions. However, in certain cases, this team opts for less complex reconstructions, such as for cardiac and severe kidney disease patients, and in recovery cases after the failure of free flaps.
In the cases presented, four situations were shown in which reconstruction with locoregional flaps were used, highlighting the importance of the knowledge of pedicle flap reconstruction techniques.
The first elderly patient with ischemic heart disease and a history of coronary surgery required a simple and quick surgery. The defect was reconstructed in three separate surgeries with three different locoregional flaps in a safe, fast, and successful manner. The aesthetic results were considered good, as the bald area on the scalp contributed to the reconstruction of the frontal defect.
The flaps used in this patient were the extended medio-frontal flap, temporal-parietal flap, and temporal-parietal-occipital flap.
The medio-frontal flap is usually limited to 7-8 cm in length12. It can be made of extended form with greater length, if it includes supraorbital with supratrochlear vessels. This flap is an excellent choice for the reconstruction of frontoparietal defects and defects of the orbital regions (Figure 2).
The scalp flaps, as they are not very elastic, should always be larger. The temporal-parietal flap can be used for the frontal and occipital regions.
The temporal-parietal-occipital flap, which may have lengths of up to 25 cm, can be used, as in the third reconstruction of the male patient (Figure 7), for contralateral defects in the pedicle. This flap can be used safely in a single time, with a stress on the importance of maintaining a minimum width of 5 cm to ensure a proper length12.
The second patient, who was initially supposed to undergo reconstruction with a microvascularized VRAM flap, instead underwent reconstruction with locoregional flaps of the forehead and scalp after the failure of microvascularized flap perfusion at 8 hours after surgery. The patient, despite an unsatisfactory aesthetic result, did not opt for another surgical procedure.
Figure 8 shows the reconstruction with an extended medio-frontal flap, which was advanced to the right hemifrontal region, and a temporal-parietal flap used to reconstruct the periorbital and temporal regions.
No infections occurred in the cases presented; however, this does not mean that these flaps are better than free flaps or that they have contributed to this result. The small number of cases allows knowledge about their applications, but does not allow for indications or for making conclusive claims on the use of locoregional flaps.
The aesthetic results tend to be most favorable when locoregional flaps are used with respect to free flaps, as long as the hairy and glabrous areas are left undisturbed11. In the cases reported here, we obtained excellent results in the first patient and a poor result on the second patient.
In the forehead reconstructions, free flaps allowed sparing the contralateral forehead, providing a better aesthetic result.
Although it is well established that the complication rates in these types of reconstructions are smaller with free flaps, Suehara et al.7 reported lower complication rates when craniofacial reconstructions were performed with local flaps, which is not a common finding reported in the literature.
The use of the microsurgical technique remains the gold standard for the reconstruction of complex scalp defects. The objective of this work was to show that there may be an indication for reconstructions with locoregional pedicled flaps.
CONCLUSION
The locoregional flaps presented in this study were safe and simple to use for reconstructing large defects in the craniofacial region. However, the small number of reconstructions limits the conclusions drawn.
The presented surgeries show that plastic surgeons can perform complex reconstructions with locoregional flaps, demonstrating that there is still room for this type of reconstruction.
REFERENCES
1. Newman MI, Hanasono MM, Disa JJ, Cordeiro PG, Mehrara BJ. Scalp reconstruction: a 15-year experience. Ann Plast Surg. 2004;52(5):501-6. DOI: http://dx.doi.org/10.1097/01.sap.0000123346.58418.e6
2. Wang HT, Erdmann D, Olbrich KC, Friedman AH, Levin LS, Zenn MR. Free flap reconstruction of the scalp and calvaria of major neurosurgical resections in cancer patients: lessons learned closing large, difficult wounds of the dura and skull. Plast Reconstr Surg. 2007;119(3):865-72. PMID: 17312489 DOI: http://dx.doi.org/10.1097/01.prs.0000240830.19716.c2
3. O'Connell DA, Teng MS, Mendez E, Futran ND. Microvascular free tissue transfer in the reconstruction of scalp and lateral temporal bone defects. J Craniofac Surg. 2011;22(3):801-4. DOI: http://dx.doi.org/10.1097/SCS.0b013e31820f3730
4. McCombe D, Donato R, Hofer SO, Morrison W. Free flaps in the treatment of locally advanced malignancy of the scalp and forehead. Ann Plast Surg. 2002;48(6):600-6. DOI: http://dx.doi.org/10.1097/00000637-200206000-00006
5. Galvão MSL, Sá GM, Farias T, Anlicoara R, Dias FL, Sbalchiero JC. Reconstrução tridimensional da face nos tumores avançados com invasão da fossa craniana anterior. Rev Col Bras Cir. 2004;31(2):124-31. DOI: http://dx.doi.org/10.1590/S0100-69912004000200010
6. Chang KP, Lai CH, Chang CH, Lin CL, Lai CS, Lin SD. Free flap options for reconstruction of complicated scalp and calvarial defects: report of a series of cases and literature review. Microsurgery. 2010;30(1):13-8.
7. Suehara AB, Kavabata NK, Toita MH, Veiga JCE, Gonçalves AJ. Complicações em ressecções craniofaciais: uma análise de 10 casos. Arq Med Hosp Fac Cienc Med Santa Casa São Paulo. 2004;50(1):7-13.
8. Gil Z, Abergel A, Leider-Trejo L, Khafif A, Margalit N, Amir A, et al. A comprehensive algorithm for anterior skull base reconstruction after oncological resections. Skull Base. 2007;17(1):25-37. DOI: http://dx.doi.org/10.1055/s-2006-959333
9. Chedid R, Sbalchiero JC, Farias TP, Galvão MSL, Moraes L, Leal PR, et al. Reconstrução craniofacial com retalhos microcirúrgicos: análise crítica. Rev Bras Cir Cabeça e Pescoço. 2009;38(2);103-7.
10. Chang DW, Langstein HN, Gupta A, De Monte F, Do KA, Wang X, et al. Reconstructive management of cranial base defects after tumor ablation. Plast Reconstr Surg. 2001;107(6):1346-55. DOI: http://dx.doi.org/10.1097/00006534-200105000-00003
11. van Driel AA, Mureau MA, Goldstein DP, Gilbert RW, Irish JC, Gullane PJ, et al. Aesthetic and oncologic outcome after microsurgical reconstruction of complex scalp and forehead defects after malignant tumor resection: an algorithm for treatment. Plast Reconstr Surg. 2010;126(2):460-70. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181de2260
12. Mathes SJ, Nahai F, eds. Reconstructive surgery: principles, anatomy and technique. New York: Churchill Livingstone; 1997. DOI: http://dx.doi.org/10.1055/s-2008-1080278
1. Hospital das Clínicas da Universidade Federal de Pernambuco, Recife, PE Brasil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brasil
Institution: Serviço de Cirurgia Plástica do Hospital das Clínicas da Universidade Federal de Pernambuco (HC-UFPE). Recife, Pernambuco, Brazil.
Corresponding author:
Rafael Anlicoara
Av. Prof Moraes Rego, S/N, Cidade Universitária
Recife, PE, Brazil Zip Code 50670-901
E-mail: rafaelanlicoara@hotmail.com
Article received: February 3, 2015.
Article accepted: October 8, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter