

Original Article - Year 2015 - Volume 30 -
Surgical treatment of skin cancer by the plastic surgeon
Tratamento cirúrgico do câncer de pele pelo cirurgião plástico
ABSTRACT
INTRODUCTION: Skin cancer is the most common neoplasm in Brazil and it corresponds to 25% of all diagnosed malignant tumors. The best treatment is surgical resection in early stages. The disease is treated by a plastic surgeon along with a multidisciplinary team. The objective is to assess the effectiveness of surgical procedures performed by plastic surgeons to treat skin cancer.
METHODS: We analyzed medical records of 404 patients operated on between February 2009 and December 2012. Data analyzed included gender, age, diagnosis, localization and evolution.
RESULTS: Patients' mean age was 62 years. A total of 53% of patients had basal cell carcinoma, 25.5% melanoma and 15.1% squamous cell carcinoma. There was a predominance of women in basal cell carcinomas (56%) and melanoma (54%) and predominance of men in squamous cell carcinomas (61%). Basal cell carcinomas (92.99%) and squamous (72.13%) were predominant in the head and neck, melanoma predominated in the trunk region (36.89%) and in lower limbs (24.27%). We performed 67 surgeries with sentinel lymph node, with positivity in 14.93%. Patients with melanoma who had metastasis accounted for 7.76% and 2.91% patients died.
CONCLUSION: Plastic surgeons are one of the important professionals for skin cancer treatment. These professionals are the most skilled one to perform reconstructions after tumor resections, because during education they learn repair concepts using grafts and flaps especially focused on aesthetic appearance of patients. They can also perform surgery for sentinel lymph node and offer follow-up to patients with skin cancer.
Keywords: Cutaneous neoplasms; Skin cancer; Carcinoma, basal cell; Carcinoma, squamous cell; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O câncer de pele é a neoplasia mais frequente no Brasil e corresponde a 25% de todos os tumores malignos. O melhor tratamento é a ressecção cirúrgica em fases iniciais. O cirurgião plástico, juntamente com uma equipe multiprofissional, participa no tratamento desta doença. O objetivo é analisar a eficácia dos procedimentos cirúrgicos realizados pelo cirurgião plástico no tratamento do câncer de pele.
MÉTODO: Foram analisados 404 prontuários de pacientes operados no período de fevereiro de 2009 a dezembro de 2012 e analisados gênero, idade, diagnóstico, localização e evolução.
RESULTADOS: Faixa etária com média de 62 anos. 53% de casos de carcinoma basocelular, 25,5% melanoma e 15,1% carcinoma espinocelular. Houve predomínio de mulheres nos carcinomas basocelulares (56%) e no melanoma (54%) e de homens nos carcinomas espinocelulares (61%). Os carcinomas basocelulares (92,99%) e espinocelulares (72,13%) tiveram sua predominância na região de cabeça e pescoço; enquanto o melanoma predominou em região de tronco (36,89%) e membros inferiores (24,27%). Foram realizadas 67 cirurgias com pesquisa de linfonodo sentinela, com positividade em 14,93%. 7,76% dos pacientes de melanoma apresentaram metástases e 2,91% vieram a óbito.
CONCLUSÃO: O cirurgião plástico é um dos profissionais importantes para o tratamento do câncer de pele, sendo o mais apto para realizar as reconstruções após as ressecções tumorais, pois tem em sua formação os conceitos de reparação, utilizando-se de enxertos e retalhos e considerando o aspecto estético dos pacientes. Cabe-lhe também a realização da cirurgia de pesquisa de linfonodo sentinela e o seguimento dos pacientes com câncer de pele.
Palavras-chave: Neoplasias cutâneas; Câncer de pele; Carcinoma basocelular; Carcinoma de células escamosas; Procedimentos cirúrgicos reconstrutivos.
Skin cancer is the most common cancer in Brazil and it represents 25% of all diagnosed malignant tumors. Approximately 130,000 new cases of skin cancer appear yearly.
Skin cancers are divided into non-melanoma and melanoma. The most common diagnosed among non-melanoma type are basal cell carcinoma (70%), followed by squamous cell carcinoma (25%). The melanoma type has an incidence of 5%1.
Despite the high incidence of basal cell carcinoma it is the less aggressive cancer and rarely produces metastases. Squamous cell carcinoma is more invasive than basal cell carcinoma and metastases may occur. Melanoma is highly invasive, easily produces metastases and has a high mortality rate if not diagnosed early.
On examination a biopsy is performed. Biopsy can be incisional for large injuries or excisional for the small injuries2.
Surgical resection in early stages is the best treatment, but other forms of treatment exist such as therapy with topical medications, cryotherapy, photodynamic therapy, radiotherapy and chemotherapy for advanced disease.
The plastic surgeon along with a multidisciplinary team including a dermatologist, responsible for the majority of skin tumors diagnoses,, an oncological surgeon, responsible for lymphadenectomy and infusion and perfusion techniques, an head and neck surgeon (in cases of large resections), and a vascular surgeons (in cases of surgery of infusion or exfusion) and an oncologist (in cases of systemic disease) who actively participate in the treatment of the disease. This team may also include a psychologists and professionals who are specialized in pain and management of advanced cases of the disease.
OBJECTIVE
This study analyzes the effectiveness of surgical procedures for skin cancer carried out by plastic surgeons.
METHODS
This retrospective study included 404 patients who were admitted and underwent surgery at specialized cancer hospital. Data were collected from electronic medical records of patients operated on by a plastic surgeon from March 2009 to December 2012.
Inclusion Criteria
We included hospitalized patients who underwent surgery and did not have palpable lymphadenopathy. Patients with palpable lymph nodes were referred to the oncological surgeon or treatment with an oncologist.
Patients had skin tumors that were benign, malignant or suspected of malignancy. Those with malignant tumors needed hospitalization for sedation or general anesthesia, and required intraoperative frozen of margins, observance of medical conditions or advanced age.
Exclusion Criteria
We excluded from the study all patients from clinical surgery center (1,130 cases) who underwent excisions, incisional biopsies, excisional biopsies, and resection of margins on the same day (Figure 1).

Figure 1. Resection of basal cell carcinoma with reconstruction using flap composed of septal cartilage and nasal mucous plus facial skin flaps. A, E: Preoperative. B: After tumor resection, C: Graft composed of septal cartilage and nasal mucous in the lower eyelid. D: Immediate postoperative period. F: Late postoperative.
Casuistry
We included 404 patients with skin tumors who were hospitalized and underwent surgery at clinical surgical center at a specialized cancer hospital.
Distribution of patient group
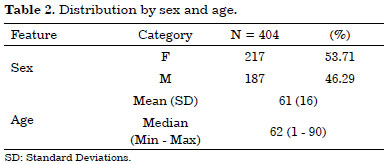
Patients' age ranged between 1 and 90 years, their mean age was 62 years. Women comprised of 53.71% and men of 46.29% of the sample.
Evaluation of tumors
Morphological classification
In all operated cases the diagnosis was skin tumors classified as benign and malignant tumors.
Histopathological classification of surgical margins
All operated cases had diagnosis confirmed by pathological examination, and all melanoma cases were reviewed before the surgery. Frozen cases were processed for histopathology by paraffin embedding.
Techniques used for surgeries
Surgical margins recommended to remove the tumors were 4 to 10mm to basal cell caricnomas3, and 6 to 10 mm for squamous cell carcinomas3 in places where there was the possibility of primary closure. In patients with tumors located in the skin or lacking its removal as the noble face forwarded to remove the lesion and freezing the banks, allowing it to uproot the entire tumor, while preserving as much healthy tissue around and taking into consideration the best aesthetic result possible.
In the case of melanoma used the following recommendation for margins as the depth of Breslow3 (Table 1):
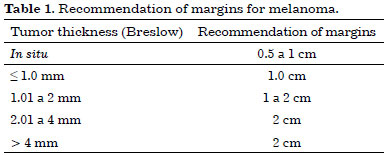
The presence or absence of metastases in regional lymph nodes that drain the primary tumor is the main prognostic factor in patients with early-stage melanoma, the most powerful predictor of recurrence and survival4. For this reason, these patients underwent sentinel lymph node staging.
The indications for surgery for sentinel lymph node were in merckel carcinomas and melanomas (Figure 2). The indication for melanoma followed the criteria3,5:

Figure 2. Resection of melanoma with craniectomy and reconstruction using trapezius muscle flap. A: After tumor resection plus cranioectomy because of bone invasion. B, C: Lifting of flap. D: Immediate postoperative period. E: 2nd waiting time. F: Postoperative.
Breslow thickness greater than or equal to 0.76 mm;
Presence of ulceration or regression;
Mitotic index greater than or equal to 1 mm2;
Clark IV and V.
The indication of achievement of sentinel lymph node in head and neck surgery is controversial in the literature for the morbidity of the lymph node and it was performed only in patients who surgery did not increase this morbidity3.
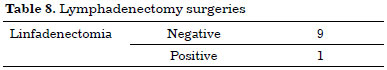
The main techniques used for reconstruction in this study were: primary closure, local flaps, neighborhood (bilobed, VY, rhomboid, nasolabial folds, frontal, glabellar, and Z-plasty), distance, and skin graft total6-8. Tumors were operated on the scalp, face, eyelids, eyebrows, forehead, nose, ear, cheek, lips, chin, neck, chest, abdomen, back, buttocks, thigh, leg and foot (Figure 3).

Figure 3. Use of patent blue and technetium for surgery of sentinel lymph node research. A: Congenital melanocytic nevus. B, F: Acral Lentiginous Melanoma. C: Merkel cell carcinoma. D: Sentinel lymph node. E: Forearm melanoma. G: Chest melanoma with axillary sentinela. H: Probe.
RESULTS
A total of 404 patients underwent surgery. Their age ranged from 1 to 90 years, and mean was 62 years. The majority of patients were women 217 (53.71)% vs. 187 (46.29%) men.
Demographic (Table 2)
Histopathologic and clinical classification of tumors
The histopathological evaluation of tumors based on classical criteria of cytologic atypia and architectural showed that 385 (95.29%) were malignant and 19 (4.7%) were benign.
Malignant tumors were of basal cell carcinoma 214 (53%), 103 (25.5%) were melanoma, 61 (15.1%) were squamous cell carcinoma, 4 (1%) were dermatofibrosarcoma protuberans, 3 (0.75%) were carcinoma merckel, other type and other less frequent type.
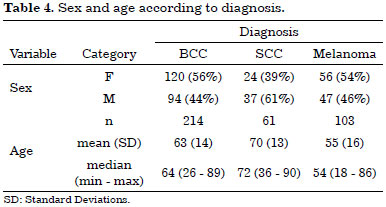
Distribution by tumors type between men and women was similar in basal cell carcinoma and melanoma, with a slight predominance of squamous cell carcinomas in men (62%) (Table 3).
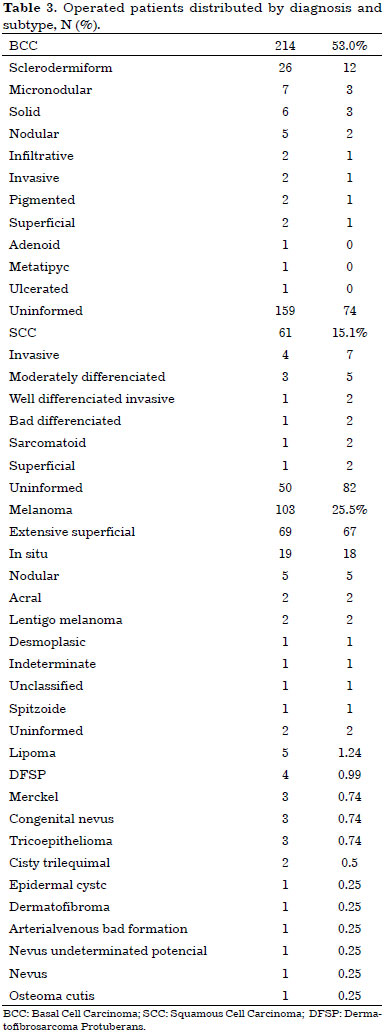
Among women there were a predominance of basal cell carcinomas (56%) and melanomas (54%). Men were more affected by squamous cell carcinomas in 61% of cases (Table 4).
Distribution of tumors by location
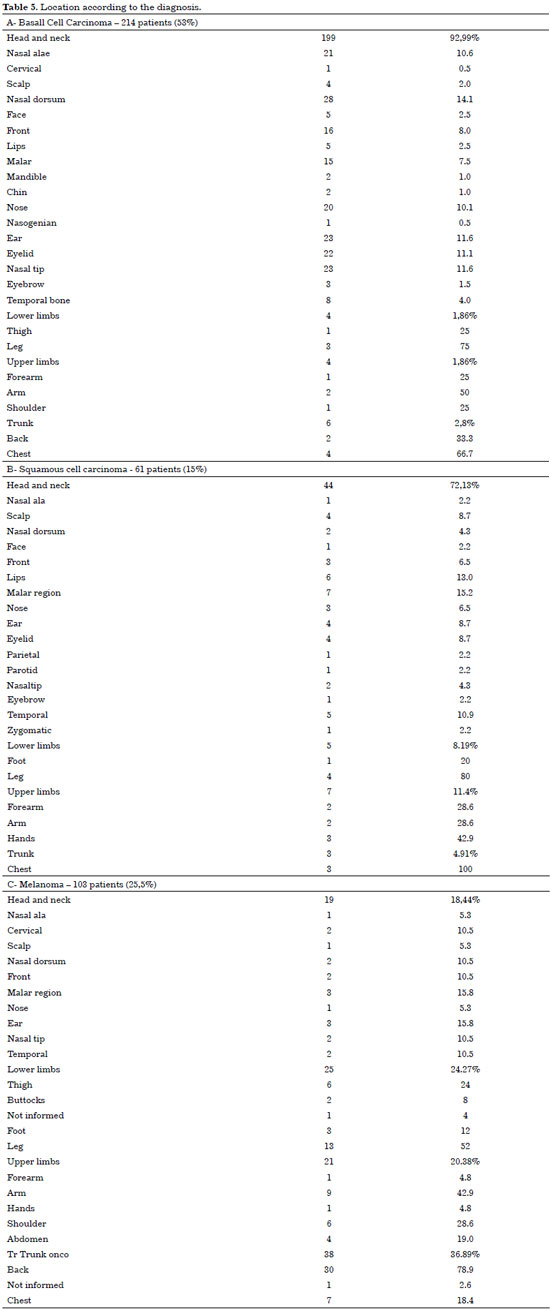
Basal cell carcinoma was mainly located on the head and neck of 199 cases (92.99%) with high incidence in regions such as nose, ear, frontal and malar. Squamous cell carcinomas also had high incidence on the head and neck of 44 cases (72.13%), it also showed high incidence in nose, cheek, lip, temporal, ear, eyelid and scalp (Figure 4).
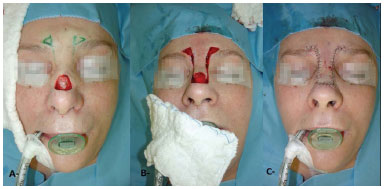
Figure 4. Resection of basal cell carcinoma with reconstruction using advancement flap. A: Defect caused by the tumor. B: intraoperative. C: Immediate postoperative.
The incidence of melanoma was higher on trunk region of 38 patients (36.89), followed by 25 patients (24.27%) with tumors in lower limbs, and 19 patients (18.44%) with tumors on head and neck region (Table 5).
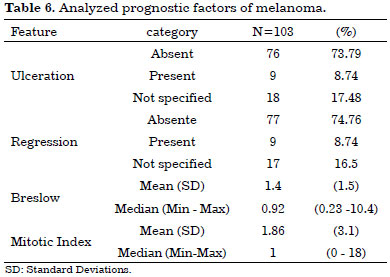
Melanoma
A total of 103 patients (67%) underwent surgery for superficial spreading melanoma followed by 18% operated on for melanomas in situ, 5% and 2% for nodular type sacral, lentigo 2% and 1% desmoplastic melanoma, 1% had spitzoid melanoma. Most cases had thin melanoma and median was 0.92. Of these, 8.74% were ulcerated and 8.74% had regression, there were no cases reported related with melanoma in situ cases which did not present specification as ulceration and regression. The mitotic index showed an average of 1.86 and median of 1 (Table 6).
Sentinel lymph node
We performed 67sentinel lymph node procedures, and lymph node involvement was obtained in 10 patients with a positivity rate of 14.93%. All cases were positive for melanoma. There was no case of positive sentinel lymph node in carcinoma of Meckel (Table 7).
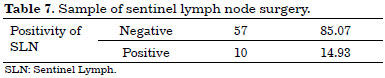
Of the 10 patients (14.93%) with sentinel lymph node compromised micrometastases who underwent lymphadenectomy, only one had other regional lymph nodes involved by tumor (Table 8).
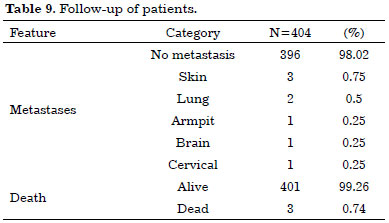
Follow-up
Patients with basal cell carcinoma and squamous cell carcinoma were followed-up according to the classification low or high risk of recurrence, with consultation return from 6 months to one year. Patients with melanoma were followed-up every 3 month for 2 years and every 6 months for 5 years, then and once a year (Figure 5). A total of 8 (7.76%) patients had metastases and 3 (2.91%) died (Table 9).
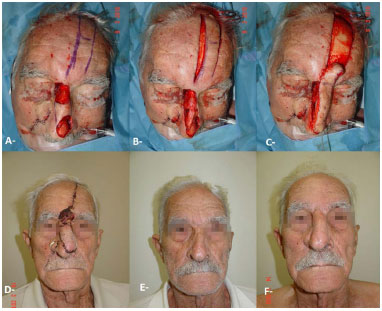
Figure 5. Resection of basal cell carcinoma with reconstruction using frontal and nasolabial flap. A, B, C: Intraoperative. D: 2nd waiting time. E: Preoperative. F: Postoperative.
Surgical complications
We used grafts and flaps in all patients who underwent surgical treatment for skin cancer, and had flap necrosis, hematoma, wound dehiscence, and seroma. Most patients with skin cancer were older than 60 years and had comorbidities. Necrosis in flaps or grafts was chosen as second intention healing in its most behavior. In some cases, granulation was awaited and covered after a surgery for skin graft. Cases with hematoma and seroma were subsequently approached and drained (Figure 6).
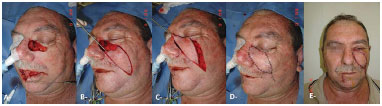
Figura 6. Resection of basal cell carcinoma and squamous cell carcinoma with reconstruction using V-Y advancement flap and lower lip flap. A; Defected caused by the tumor. B, C: Intraoperator. D: Immediate postoperative. E: Late postoperative.
Histopathological evaluation of margins
The analysis of margins was performed by the pathologist and classified as free, compromised and confined. All operated cases had diagnostic confirmation by histopathological examination and were classified as free margins, confined and compromised. All cases with inadequate and compromised margins were resubmitted to surgery until they become free.
The frozen cases were later examined by paraffin embedding, and 3 cases were considered free during freezing and subsequently the compromised margins were waxed, and reoperated until they become free. All cases of melanoma were reviewed before surgery (Figure 7).

Figure 7. Resection of basal cell carcinoma with reconstruction using bilobed flap. A: Defect after tumor resection. B: Immediate postoperative. C: Preoperative. D: Late postoperative.
Recurrence tumor
Only one patient had a local recurrence in squamous cell carcinoma invading the region of the ear canal and lymph node metastasis in cervical region. We did not receive any recurrence of basal cell carcinoma, but 69 patients (15%) had a second or more skin tumors, which required a second and even a third surgery (Figure 8).

Figure 8. Resection of basal cell carcinoma with reconstruction of nasolabial flap in two different times. A: Preopeative. B,D: Intraoperative. E: Immediate postoperative. C, F: Late postoperative.
DISCUSSION
Skin cancer is the most common neoplasm in Brazil. If diagnosed early, the disease shows high rates of cure.
This study analyzed the effectiveness of surgical procedures performed by plastic surgeon along with a multidisciplinary team to treat skin cancer.
We included 404 patients with skin tumors who were admitted at our service and underwent surgery. Those with positive lymph nodes were referred to oncological surgeon and excluded from the sample. Participants' age ranged from 1 to 90 years, their mean was 62 years. The mean age agrees with findings reported in the literature which shows a higher incidence of patients over 60 years, a rising incidence of people under 50 years and women aged 40 years9.
Basal cell carcinomas (56%) and melanomas (54%) were common among women, while 61% of squamous cell carcinomas cases were seen among men. Literature shows that majority of basal cell and squamous cell carcinoma occurs in men, but melanoma is predominantly in women before 40 years old, this type of cancer incidence increases in men over 40 years9.
Skin cancer types were divided into non-melanoma and melanoma. The most common non-melanoma were basal cell carcinoma that accounted for 70% of diagnoses, followed by squamous cell carcinoma accounting for 25%. The melanoma type had incidence of 5%1. Tumors were first evaluated histopathologically. We observed that 385 (95.29%) were malignant and 19 (4.7%) were benign. Of malignant tumors, 214 (53%) were basal cell carcinoma, 103 (25.5%) melanoma, 61 (15.1%) squamous cell carcinoma, 4 (1%) dermatofibrosarcoma protuberans, 3 ( 0.75%) merckel carcinoma and remaining were other less frequent cancer types. Because the study was carried out at a specialized cancer center, we believe that the high number of melanoma cases was due to the fact that our center received patients referred from other services and from a variety of regions in the country where there are no conditions for sentinel lymph node surgery.
Basal cell carcinomas (92.99%) and squamous cell carcinomas(72.13%) were predominant on head and neck region, more specifically on the nose and face. Melanoma was more common on trunk (36.89%) and lower limbs (24.27%). There are also reports in literature showing high incidence of basal cell carcinomas and squamous in the nasal region, the incidence described is 20.9% 9.
In the literature Mohs surgery efficacy reported is about 98% to 99% for basal cells carcinomas6. The rate of positive margins in the study were seen in 3 cases (1.4%) of basal cell carcinomas that presented clear margins after freezing and histopathology processed by paraffin embedding which showed positive margins. All participants with compromised margins underwent reoperation until margins become free. Patients who did not have clinical conditions for the surgery were submitted to the procedure with local anesthesia or were referred to radiotherapy. In our study, margins of the basal cell carcinomas were examined by a pathologist. All margins were frozen, including deep margins (Figure 9).

Figure 9. Resection of squamous cell carcinoma and reconstruction using Karapandzic flap. A, E: Preoperative. B: After tumor resection. C: Preservation of vessels and nerves. D: Immediate postoperative. F: Late postoperative.
Prognostic factors for melanoma include multivariate analysis of primary melanoma such as patient's age, sex, site of primary tumor thickness, ulceration and index mitotic4. In melanoma type, we analyzed patient's age, sex, site of the tumor, thickness, ulceration, regression, however, there was no enough follow-up data to indicate the prognosis.
The melanomas types that were operated on (103) were superficial spreading (67%) followed by melanomas in situ(18%), nodular (5%), acral(2%), lentigo (2%), desmoplastic melanoma (1%), and spitzoid (1%). Most tumors were thin and median measurement of 0.92.
In our sample, 8.74% of tumors had ulceration and 8.74% regression. These cases do not refer to the melanomas in situ which no specification for ulceration and regression was seen. The mitotic index showed a mean of 1.86 with compared with literature median of 1. We included only patients who underwent surgery with a plastic surgeon, and did not have palpable lymph node. Because of criteria applied to select patients, those who had lymph nodes were referred for surgery and/or follow-up with cancer surgeon and oncologist. Our study does not represent a random sample with incidence or prevalence of melanoma cases.
The presence or absence of metastases in local lymph nodes that drain the primary tumor is the main prognostic factor in patients with early stage melanoma, which constitutes a powerful predictor of recurrence and survival10. Patients with melanoma and Merckel cell carcinoma underwent sentinel lymph node staging .
A total of 67 surgeries were performed with sentinel lymph node by using a combination of techniques with patent blue and radioisotope technetium injection one day before the surgery. The only identification with blue dye was 87% against 99% associated with blue and technetium11. Experienced professionals can identify in lymphatic mapping the sentinel node in 98-100% of cases. The sentinel lymph nodes were found in 100% of operated cases in our study. All positive cases in our sample were melanoma.
Indexes literature suggested melanomas between 0.76 mm and 1mm and with mitotic index greater than or equal to 1 mm2 were associated with a 10% risk of metastasis in sentinel lymph node10. Compared to the present study, in which melanomas were thin, and had median measurement of 0.92, and an average mitotic index of 1.86 and median of 1, we obtained 10 melanoma patients (9.7%) with positive sentinel nodes. Findings are quite similar to statistics reported in the literature.
In our study, of the 67 surgeries for sentinel lymph node only 2 (2.98%) had seroma and were treated with drainage and spontaneous resolution. No patient had later lymphedema. Surgery for sentinel lymph node has low morbidity, but if the patient has other comorbidities, this may constitutes a contraindication for surgery. In cases with contraindication , recommendation is surgical excision of margins. Studies indicate that this surgery does not increase the patients' survival rate 3.
The sentinel lymph node is the most important predictor for patients in early-stage melanoma and it is relevant for treatment planning of the disease. The absence of metastatic disease in sentinel lymph node is a predictive factor of longer survival and no future recurrence10.Plastic surgeons can perform sentinel lymph node surgery using two different techniques with patent blue injection and associated with radioisotope technetium. Their must understand these medication indications for follow-up of the disease.
Plastic surgeons are one of the important professionals for skin cancer treatment. These professionals are the most skilled one to perform reconstructions after tumor resections, because during education they learn repair concepts using grafts and flaps especially focused on aesthetic appearance of patients. They can also perform surgery for sentinel lymph node and offer follow-up to patients with skin cancer (Figure 10).
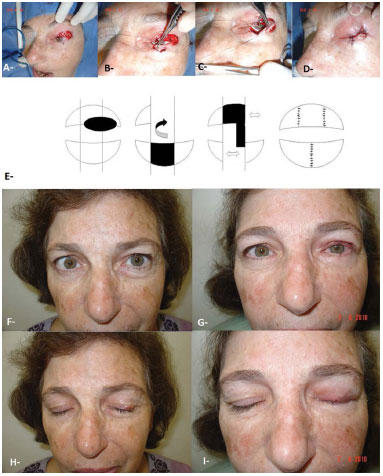
Figure 10. Resection of basal cell carcinoma and reconstruction with lower lip flap. A: After tumor resection. B, C: Intraoperative, D: Immediate postoperative. E: Didactic scheme of the flap. F, H: Preoperative. G, I: Postoperative.
CONCLUSION
Early diagnosis and early-stage surgery are still the best options for skin cancer treatment. These options have high cure rates and low mortality.
Surgical procedures performed by plastic surgeon show efficacy for skin cancer treatment and present low complications and recurrence.
Plastic surgeons are one of the important professionals for skin cancer treatment. These professionals are the most skilled one to perform reconstructions after tumor resections, because during education they learn repair concepts using grafts and flaps especially focused on aesthetic appearance of patients. They can also perform surgery for sentinel lymph node and offer follow-up to patients with skin cancer.
REFERENCES
1. Brasil. Ministério da Saúde. Instituto Nacional do Câncer. Estimativa 2012: Incidência de câncer no Brasil [Acesso 17 Nov 2015]. Disponível em: http://www2.inca.gov.br/wps/wcm/connect/1c7b8a8047f165449023dd9ba9e4feaf/estimativa-2012-incidencia-do-cancer.pdf?MOD=AJPERES&CACHEID=1c7b8a8047f165449023dd9ba9e4feaf
2. Carreirão S. Sociedade Brasileira de Cirurgia Plástica. Cirurgia Plástica. Atheneu; 2005. p.801.
3. The National Comprehensive Cancer Network (NCCN), Guidelines [Acesso 17 Nov 2015]. Disponível em: http://www.nccn.org/
4. Atkins MB, Hauschild A, Wahl RL, Balch CM. Diagnosis of Stage IV melanoma. In: Balch CM, Houghton AN, Sober AJ, Soong SJ, Atkins MB, Thompson JF, eds. Cutaneous Melanoma. 5th ed. Louis: Quality Medical Publishing; 2009.p.573-602.
5. Balch CM, Mihm MC, Gershenwald JE, Soong S-j. The revised melanoma staging system and the impact of mitotic rate [Acesso 17 Nov 2015]. Disponível em http://www.skincancer.org
6. Uptodate. Epidemiology and clinical features of basal cell carcinoma [Acesso 17 Nov 2015]. Disponível em http://www.uptodate.com
7. Mélega JM, ed. Cirurgia Plástica. Fundamentos e Arte. Princípios Gerais. Rio de Janeiro: Guanabara Koogan; 2009. p.283-383.
8. Baker SR. Local flaps in facial reconstruction. 2nd ed. Mosby; 2007.
9. Wolf K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ. Fitzpatrick's, Dermatology in general medicine. 7th ed. New York: McGraw-Hill Professional; 2006.
10. Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199-206. DOI: http://dx.doi.org/10.1200/JCO.2009.23.4799
11. De Vita VT, Hellman S, Rosenberg SA, eds. Cancer: principles and practice of oncology. Philadelphia: Lippincott-Raven; 1996.
1. A.C. Camargo Cancer Center, São Paulo, SP, Brazil
2. Cruz Vermelha Brasileira, São Paulo, SP, Brazil
Institution: A.C. Camargo Cancer Center, São Paulo, SP, Brazil.
Corresponding author:
Marcelo Norio Inada
Rua Albina Barbosa, 210
São Paulo, SP, Brazil Zip Code 01530-020
E-mail: mninada@hotmail.com
Article received: September 11, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter