

Original Article - Year 2015 - Volume 30 -
Sexuality after breast augmentation
Sexualidade após mamoplastia de aumento
ABSTRACT
INTRODUCTION: The breasts are symbol of femininity, motherhood and sexuality. Breast augmentation is the second most performed cosmetic surgery in Brazil, and it is related to improvement of body image, self-esteem and quality of life. Sexuality is a significant component of quality of life. The female sexual quotient questionnaire (FS-Q) was validated as an evaluation tool for sexuality, and it is used to evaluate the impact of many treatments for sexual health. The questionnaire entails 10 questions, which assess four domains of sexuality: sexual desire, sexual arousal, comfort and sexual satisfaction. To evaluate sexuality after breast augmentation.
METHODS: We selected 47 patients with interest in breast enlargement. During treatment patients completed the FSQ questionnaire before and after 2, 4 and 18 months of the surgery. The surgical technique used was the same for all patients: inframammary incision, subglandular pocket, round implant, volume 260 to 325 mL. There were four groups: with or without stable relationship, and with or without striae.
RESULTS: A total of 45 patients were considered for the study. Patients' mean age was 26 years. Complications observed were: symmastia (1), galactorrhea (1), and striae distensae(10). Significant improvement was observed between the total FSQ score at preoperative, 4 months (p = 0.001), and postoperative, 18 months (p = 0.001), and also related with the significant increase in arousal scores (p < 0.001), and sexual satisfaction (p = 0.001). Patients with striae did not show significant improvement in sexuality (p = 0.627), differently of patients without striae (p < 0.001). No significant difference in sexuality was seen between the group with or without stable relationship.
CONCLUSION: Sexuality increases significantly after breast augmentation.
Keywords: Sexuality; Breast; Mammaplasty; Quality of life.
RESUMO
INTRODUÇÃO: A mama é símbolo de feminilidade, maternidade e sexualidade. Mamoplastia de aumento é a segunda cirurgia estética mais realizada no Brasil, e está relacionada à melhora da imagem corporal, autoestima e qualidade de vida. Sexualidade é importante componente da qualidade de vida. O quociente sexual feminino (QS-F) é questionário desenvolvido e validado que avalia sexualidade, aplicado para avaliar o impacto do tratamento na saúde sexual. Consiste em 10 questões, que avaliam quatro domínios: desejo, excitação, conforto e satisfação sexual. O objetivo é avaliar a sexualidade após mamoplastia de aumento.
MÉTODOS: 47 candidatas a aumento das mamas foram selecionadas, tratadas cirurgicamente, e responderam ao questionário QS-F no pré e no pós-operatório de 2, 4 e 18 meses. A técnica adotada foi semelhante para todas pacientes: incisão no sulco mamário, loja subglandular, implante redondo entre 260 e 325 mL. Foram formados os grupos: com ou sem relacionamento estável; e com ou sem estrias.
RESULTADOS: 45 pacientes concluíram o estudo, com idade média de 26 anos. As complicações observadas foram: simastia (1), galactorreia (1), e estrias (10). Houve melhora significante entre o escore total do QS-F no pré e no pós-operatório de 4 (p = 0,001) e 18 meses (p = 0,001), relacionado ao significante aumento da pontuação dos domínios excitação (p < 0,001) e satisfação sexual (p = 0,001). Nas pacientes que apresentaram estrias não houve melhora significante da sexualidade (p = 0,627), ao contrário das que não apresentaram (p < 0,001). Não houve diferença significante na sexualidade entre o grupo com ou sem relacionamento estável.
CONCLUSÃO: A sexualidade aumentou significantemente após mamoplastia de aumento.
Palavras-chave: Sexualidade; Mama; Mamoplastia; Qualidade de vida.
According to the World Health Organization, the term "health" encompasses many different aspects, including physical and psychological well-being1. In women, breast cancer represents social and cultural values, and is a symbol of femininity, motherhood and sexuality2.
Hypomastia is a common complaint. Patients who are candidates for breast augmentation have different characteristics in relation to body structure and breast tissues: height and weight, thickness of skin and subcutaneous tissue, degree of sagging, parenchyma thickness, and inter-papillary muscle distance. Three measurements are important to estimate volume of the implant to be used: base width of breast, nipple-to-inframammary fold distance and thickness of skin and subcutaneous (pinch test)3.
The breast augmentation is the second most commonly plastic surgery performed in Brazil. In 2011, in Brazil, approximately 148,000 surgeries for breast enlargement were performed, which accounted for 16.45% of total cosmetic plastic surgeries performed in this year4.
The popularity of cosmetic breast augmentation has surged, and with it, the interest in the psychological aspects of the procedure5. The results of surgery should be done not only through clinical examinations and assessment, but also by the patient's own opinion about the results6. Some instruments have been developed and used to assess the quality of life, body image, self-esteem and sexuality.
Dissatisfaction with body image is considered to be the central motivation for the surgery. The breast augmentation surgery is related to improved body image, self-esteem and quality of life7. Sexuality is an important component of quality life8. We can evaluate the result of treatment from the patient's point of view by means of questionnaires on quality of life, body image, self-esteem and sexuality.
In Brazil, 8.2% of women complain of absolute lack of sexual desire, 26.2% do not reach orgasm, 26.6% have difficulty in arousal and 17.8% have had pain during intercourse. Sexual dysfunction is the inability to participate with satisfaction in sexual relationship. In women, sexual dysfunctions are characterized by absence, excess, discomfort and/ or pain in the development of the sexual response cycle, which may impair one or more phases of this cycle (sexual desire, sexual arousal and/or orgasm). In 1998, a multi-disciplinary international consensus of female sexual dysfunction was developed, This consensus classified sexual dysfunction in four major categories: disorders of desire, sexual arousal, orgasm, and pain during intercourse sexual9. The earlier the cycle commitment occurs, the greater the damage of sexual response10.
OBJECTIVE
Assess sexuality in patients undergoing breast augmentation.
METHODS
Forty-seven patients for breast augmentation were selected and invited to participate in the study. We included patients aged 18 to 45 years with a steady partner or not, not including patients with decompensated systemic diseases, breast ptosis grade II or III (Regnault)11, pregnant women, or women who breastfed within the last six months. Patients who agreed to participate in the study, signed an informed consent.
In the preoperative period, demographic data, and photographic documentation were registered The clinical evaluation were performed by two plastic surgeons with more than two years of experience in the field. Subsequently, the questionnaire Female Sexual Quotient (FS-Q) was applied. The F-QS is a validated Brazilian questionnaire to assess sexual activity of women, an assessment tool for sexuality. This questionnaire is applied in several areas to assess the impact of treatment on the sexual health of patients. The questionnaire entails 10 questions with answers score ranging from 0 to 5, where 0 is never and 5 always. The FS-Q can be interpreted in terms of the total score, assessing sexual satisfaction, or you can evaluate each of the four domains: desire and sexual interest (questions 1, 2 and 8); foreplay, sexual arousal and personal harmony with the partner (questions 3, 4 and 5), comfort (question 7), orgasm, and satisfaction (questions 9 and 10)9. Each patient received a protocol number from 1 to 47, and the questionnaires were placed in envelopes numbered 1 through 47. The form of the questionnaire was assisted by self-administration: the questionnaire was self-administered in a private room and the researcher remained in a room next door in order to answer, if necessary, any questions regarding the questionnaire.
Clinical examination was performed by two plastic surgeons who evaluated the patients individually. Three measures were used to estimate the volume of the implant to be used: base width of breast, distance from papilla to inframammary fold and thickness of skin and subcutaneous tissue through pinch test3.
Surgeries were performed at a general hospital, all procedures were done by the same surgeon, under general anesthesia and hospitalization time were about 24 hours. The technique was standardized: the inframammary fold incision of about 3.5 to 4.5 cm, subglandular pocket, as indicated by clinical examination (Figura 1). Drains were not used in any patient. The closure was standardized in three steps: subcutaneous tissue with 3-0 nylon; subdermal points with 4-0 nylon colorless, and intradermal points with 4-0 nylon black. A tape was placed on the wound, and the dressing was done with gauze. In addition, all patients used postoperative bra immediately after the surgery until two months after surgery. Patients return were scheduled with 7, 14 days, 1, 2, 4, 6, 12 and 18 months, and FS-Q questionnaire was administered postoperatively at 2, 4 and 18 months.
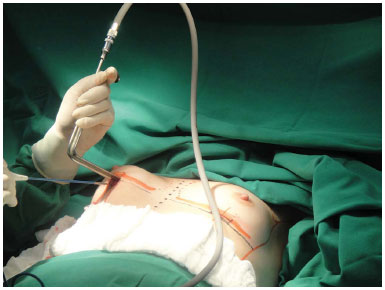
Figure 1. Standardize technique - incision in inframammary sulcus, dissection of anterior chest pocket.
Some patients had sriae rubra (acute) on the breasts after surgery (Figure 2). There was a group of patients with stretch marks and another group without. Patients with striae were treated with non-ablative fractional laser erbium glass for eight months, one session per month. Excellent results were showed after treatment12.

Figure 2. Complication: 9 weeks after surgery, recent red striae in breast augmentation 3 months after surgery. Round textured silicone implant, super high profile implants, 280 mL.
Statistical analysis was carried out using the SPSS software (version 17.0, SPSS, Inc., Chicago, III). Results were submitted to the Friedman test, Mann-Whitney test and Dunn's multiple comparison. P value < 0.05 was considered statistically significant.
RESULTS
Patients' mean age was 26 years, median of 25 years. One patient lost the follow-up and did not answer all questionnaires. Another patient developed symmastia and required further surgery, improvement was seen after this new approach. A total of 45 patients completed the follow-up of 18 months. The implants used were Eurosilicone, high and ultrahigh profile, with volume ranging from 260 to 325ml, 285ml average (Figures 3 to 10).

Figure 3. Preoperative 1.

Figure 4. Post-operative 1, 4 months, round textured implant, 260 mL to left and 280 mL to right, high profile implant.
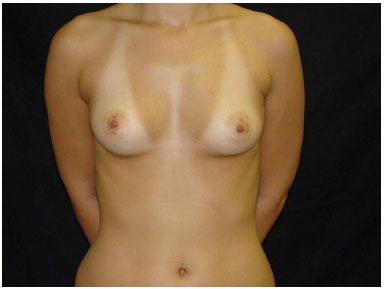
Figure 5. Preoperative 2.

Figure 6. Post-operative 2, 12 months, round textured implant, 280 mL, high profile implant.
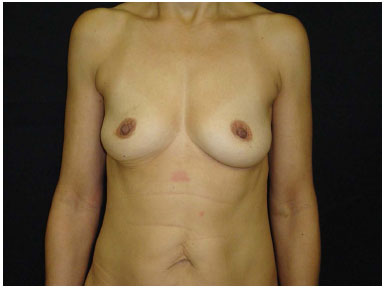
Figure 7. Preoperative 3.
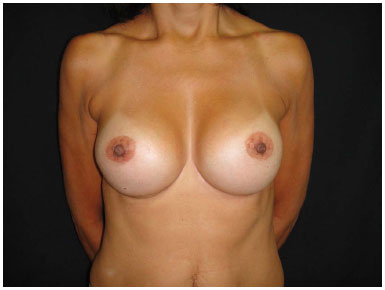
Figure 8. Post-operative 3, 18 months, round textured implant, 280 mL, super high profile implant.
Figure 9. Preoperative 4.

Figure 10. Post-operative 4, 12 months, round textured implant, 300 mL, high profile implant.
After the surgery, the following complications were seen: a case of galactorrhea (Figure 11), which started ten days after surgery, and were presented as output of milky secretion from the surgical wound and from the papilla; the patient was treated with parlodel® for 15 days and had improvement of symptoms (Figure 12) followed by monitoring and research with gynecology team; another case of symmastia (Figure 13) occurred in the second postoperative month; the patient underwent a new surgical approach and surgical team changed the plan for posteropeitoral pocket (Figure 14). In addition, there were ten cases of striae distensae in the early postoperative period.

Figure 11. Galactorrhea. Milky discharge by papillae and by operative wound after 2 days of the surgery.

Figure 12. Galactorrhea - After clinical treatment, 4 months after surgery.

Figure 13. Symmastia, complaint on the 2nd month after surgery.

Figure 14. Symmastia, after new surgical approach and planning change, posterior chest pocket.
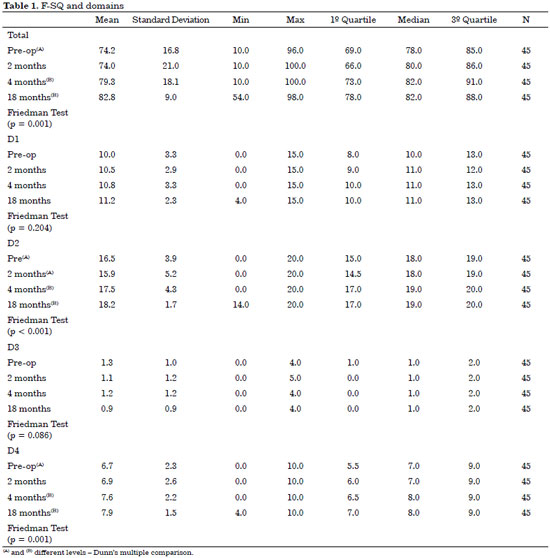
Comparing scores of questionnaires applied before and after surgery, a significant improvement in the total score of the F-QS was observed in postoperative period at 4 and 18 months (p = 0.001) related to the significant increase in the scores of arousal (p <0.001) and sexual satisfaction (p = 0.001) domains at the same time postoperatively (Table 1).
The study by Figueroa-Haas evaluated sexuality after breast augmentation using the Female Sexual Function Index (FSFI). He results showed high correlation between sexuality and breast augmentation. Furthermore, it also reported the relationship between self-esteem and sexuality, and self-esteem and surgery. Based on analysis of the fields/domains of human sexuality, there was no statistical difference with significant improvement in all domains assessed, but the most striking difference was in the field of sexual arousal8.
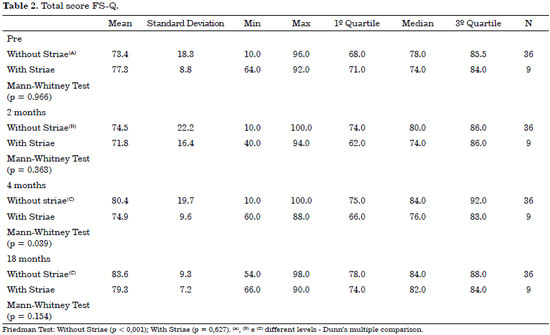
Ten patients developed stretch marks on breasts from the second postoperative month, so there were a group of patients with striae rubra (n = 10) and one without (n = 35). We treated ten patients with striae for eight months with non-ablative fractional laser erbium glass, and had excellent results12. Stretch marks have emerged from the 9th week and 16th week after surgery (mean 11.7 weeks), between the 2nd and 4th month. The laser treatment ended around the 10th to 12th month, before the end of our study.
Only the group with striae showed no significant increase (p < 0.001) in the total score of the F-SQ (Table 2).
We compared patients with or without stable relationship during the period of the study, but no statistical difference was seen in different areas and/or periods of data collection. Menezes assessed patient's sexuality through FSFI after mastectomy and after breast reconstruction, he observed an improvement of sexuality in patients who had their breast reconstructed compared with those who did not rebuilt. In addition, no relationship was seen between sexuality improvement and time of surgery, or ever in terms of socio-economic level, stable relationship or age range13.
CONCLUSION
We observed significant improvement of sexuality in patients undergoing breast augmentation after 4 and 18 months of the surgery. There was improvement in the sexual arousal and sexual satisfaction of participants, which corresponded to improvement of total score.
REFERENCES
1. The WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403-9. DOI: http://dx.doi.org/10.1016/0277-9536(95)00112-K
2. Harris DL. Self-consciousness of disproportionate breast size: a primary psychological reaction to abnormal appearance. Br J Plast Surg. 1983;36(2):191-5. PMID: 6831099 DOI: http://dx.doi.org/10.1016/0007-1226(83)90091-7
3. Tebbetts JB. A system for breast implant selection based on patient tissue characteristics and implant-soft tissue dynamics. Plast Reconstr Surg. 2002;109(4):1396-409. DOI: http://dx.doi.org/10.1097/00006534-200204010-00030
4. http://www2.cirurgiaplastica.org.br/wp-content/uploads/2012/11/sbcp_isaps.pdf
5. Crerand CE, Infield AL, Sarwer DB. Psychological considerations in cosmetic breast augmentation. Plast Surg Nurs. 2009;29(1):49-57. DOI: http://dx.doi.org/10.1097/01.PSN.0000347725.13404.5f
6. Pusic AL, Chen CM, Cano S, Klassen A, McCarthy C, Collins ED, et al. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg. 2007;120(4):823-37. DOI: http://dx.doi.org/10.1097/01.prs.0000278162.82906.81
7. Abla LEF, Sabino Neto M, Garcia EB, Ferreira LM. Quality of life and self-esteem outcomes following augmentation mammaplasty Rev Bras Mastologia. 2010;20(1):22-6.
8. Figueroa-Haas CL. Effect of breast augmentation mammoplasty on self-esteem and sexuality: a quantitative analysis. Plast Surg Nurs. 2007;27(1):16-36. DOI: http://dx.doi.org/10.1097/01.PSN.0000264159.30505.c9
9. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191-208. DOI: http://dx.doi.org/10.1080/009262300278597
10. Abdo CHN. Quociente sexual feminino: um questionário brasileiro para avaliar a atividade sexual da mulher. Diagn Tratamento. 2009;14(2):89-91.
11. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
12. Guimarães PA, Haddad A, Sabino Neto M, Lage FC, Ferreira LM. Striae distensae after breast augmentation: treatment using the nonablative fractionated 1550-nm erbium glass laser. Plast Reconstr Surg. 2013;131(3):636-42. PMID: 23446573 DOI: http://dx.doi.org/10.1097/PRS.0b013e31827c7010
13. Sabino Neto M, de Aguiar Menezes MV, Moreira JR, Garcia EB, Abla LE, Ferreira LM. Sexuality after breast reconstruction post mastectomy. Aesthetic Plast Surg. 2013;37(3):643-7. DOI: http://dx.doi.org/10.1007/s00266-013-0082-8
Universidade Federal de São Paulo, São Paulo, SP, Brazil
Institution: UNIFESP - Escola Paulista de Medicina, São Paulo, SP, Brazil.
Corresponding author:
Paulo Afonso Monteiro Pacheco Guimarães
Rua Pedro de Toledo, 544, Vila Clementino
São Paulo, SP, Brazil Zip Code 04039001
E-mail: contato@drpauloguimaraes.com.br
Article received: July 14, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter