

Original Article - Year 2015 - Volume 30 -
Pectoralis major muscle strap in mammoplasty: personal experience
Cinta do músculo peitoral maior nas mamoplastias: experiência pessoal
ABSTRACT
INTRODUCTION: Several authors have reported on mammoplasty procedures using a pectoral muscle strap, but evaluated these techniques subjectively without a comparison group. In 2011, Swanson proposed a protocol including objective parameters that was based on standardized photographic measures for the aesthetic assessment of breast surgeries. Accordingly, this study aimed to evaluate the influence of the pectoralis major muscle strap compared to a technique that does not use a muscle strap as proposed by Swanson.
METHOD: This retrospective cohort study included 18 women who underwent primary bilateral mammoplasty to correct breast ptosis and/or hypertrophy performed consecutively by a single surgeon between March 2010 and November 2012. Thirty-six breasts were divided in two groups (18 breasts in the group with a muscle strap, Group I; and 18 in the group without a muscle strap, Group II) and the outcome was assessed in a photometric study comparing the preoperative appearance to the 6-month-postoperative appearance. The results of each breast were analyzed using SPSS version 20 for Mac software.
RESULTS: The average percentage evolution of breast projection elevation in Group I was 15.32 ± 2.41% higher than that in Group II (p < 0.001, 95% confidence interval [CI], 10.41-20.22). The same result was observed for upper pole projection, which was 24.2 ± 3.71% higher (p < 0.001, 95% CI, 16.65-31.82) in Group I than in Group II.
CONCLUSION: Use of the muscle strap effectively filled the upper pole of the breast and maintained its projection for a post-mammoplasty period up to 6 months.
Keywords: Mammoplasty; Pectoral muscle; Breast; Reconstructive surgical procedures
RESUMO
INTRODUÇÃO: Alguns autores têm divulgado resultados de mamoplastias com cinta muscular do músculo peitoral, utilizando parâmetros subjetivos e sem um grupo de comparação. Em 2011, Swanson propôs um protocolo com parâmetros objetivos e não observador dependentes, baseado em medidas fotográficas padronizadas para avaliação estética das cirurgias mamárias. Com base nestas informações, este estudo teve por objetivo avaliar a influência da cinta do músculo peitoral maior comparativamente à técnica sem uso de cinta nas mamoplastias, conforme proposto por Swanson.
MÉTODO: Coorte retrospectiva envolvendo 18 mulheres submetidas à mamoplastia bilateral primária por ptose e/ou hipertrofia mamária operadas consecutivamente por um único cirurgião de março de 2010 a novembro de 2012. As 36 mamas foram divididas em dois grupos (18 mamas no grupo em que a mamoplastia foi confeccionada com cinta muscular e 18 no grupo sem cinta muscular) e avaliadas por estudo fotométrico no pré-operatório e após seis meses da cirurgia. Os resultados de cada mama foram analisados com o uso do programa "SPSS 20 for MAC".
RESULTADOS: A evolução percentual da elevação da projeção mamária média, no grupo com cinta foi 15,32 ± 2,41% superior ao grupo sem cinta (p < 0,001, IC95% de 10,41 a 20,22). O mesmo foi observado na projeção do polo superior, que foi 24,2 ± 3,71% maior (p < 0,001, IC95% de 16,65 a 31,82) do que no grupo em que a cinta não foi utilizada.
CONCLUSÃO: A cinta muscular mostrou-se efetiva para o preenchimento do polo superior da mama e para a manutenção da sua projeção no período de até seis meses após a mamoplastia.
Palavras-chave: Mamoplastia; Músculos peitorais; Mama; Procedimentos cirúrgicos reconstrutivos.
Mammoplasty is one of the most studied plastic surgery procedures. Major advances in the standardization and concepts of this surgical procedure over time have decreased its clinical complications and provided better aesthetic results. However, mammoplasty is often associated with patient dissatisfaction due to the 2-month-postoperative recurrence of breast ptosis1.
The skin marking techniques that are widely used today were proposed by Wise2 and Pitanguy3 in the mid-20th century. To manage the breast parenchyma, these authors encouraged the removal of the lower pole of the breast, leaving the skin to support and maintain the mammary cone. However, this approach favors early sliding of the upper pole, which mainly occurs in women with sagging skin and a less dense breast parenchyma. This is subsequently followed by breast ptosis regardless of suture technique or overlapping with dermoglandular flaps3-7.
To prevent premature breast ptosis and improve upper pole projection (UPP), in 1975 Ribeiro8 proposed, in combination with skin marking techniques suggested by Wise2, the use of a dermoglandular flap of the inferior pole with a vascular pedicle based on perforating vessels of the pectoralis major muscle and de-epidermized dermis fixed to the superior fascia in the central region. Although this approach contributed significantly to improving upper-pole projection, we still observed a high incidence of breast ptosis 2 months postoperatively in women with predominantly fatty breasts. This is due to breast parenchyma sliding from the flap itself, which is associated with the descent of the lipoglandular component from the skin flap. As an alternative, Silveira-Neto9 and Losken & Holtz10 proposed the rotation of a thick areolar flap with the superomedial vascular pedicle, which allows the tissue to advance in the direction of the upper breast portion as previously described by Schwartzmann1 in 1930. Although this approach seems to be a good option for breasts with a high degree of ptosis, low parenchymal density, and pronounced sagging skin, it has not yet provided the results expected by many patients and surgeons.
Given the good projection of the upper pole achieved in the early postoperative period in patients with dense breast parenchyma using the flap reported by Ribeiro8, who simulated an implant and aimed to achieve longer-lasting filling results, Daniel11 and Caldeira & Lucas12, following the concept initially described by Göbell13 in 1927, proposed the use of flaps of the entire thickness of the pectoralis major muscle that can sustain the projection results and induce muscle tension. This was considered a way to limit sliding of the lipoglandular content from this inferior pole flap. However, these techniques were not very well accepted due to the aesthetic changes produced by the voluntary movement of the pectoral muscles, possible interference of muscle tissue in mammography images, and potential compromising of breast cancer evolution, which would impair cancer treatment plans.
Graf et al.14-18 proposed modifications and standardized the superficial use of two-thirds of the pectoralis major muscle shaped as a muscular bipedicled strap with closure of the posterior third. The aim was to avoid compromising the lymphatic muscular drainage and maintain glandular and muscular plane integrity to increase the procedure's oncological safety.
In the last decade, several authors15-21 disclosed aesthetic results of mammoplasty procedures using a muscle or fascial strap of the pectoralis major muscle. The evaluation of these techniques used subjective parameters and included no comparison group. Until 2011, there was no model for a standardized objective evaluation of aesthetic breast results and their subsequent postoperative evolution, and notes resulting from a visual and/or photographic analysis with randomly defined scales and even radiographic comparisons assessing evolution using radiopaque markers were used. To prevent this limitation, Swanson22-24 proposed a protocol in which objective parameters that did not rely on the subjective evaluator's opinion were clearly defined. These parameters were based on measures outlined in standardized profile photographs and compared the pre- and postoperative periods using a photographic software.
OBJECTIVE
Since no studies to date have compared mammoplasty procedures with versus those without a muscle strap using photographic measures as proposed by Swanson22,23, this study aimed to evaluate the influence of the pectoralis major muscle strap in relation to techniques that did not use a muscle strap in mammoplasty. The evaluation was performed by photographic measurements within a 6-month postoperative period.
METHOD
Study design and cohort
This retrospective cohort study included 18 women who consecutively underwent primary bilateral mammoplasty for the correction of breast ptosis and/ or hypertrophy performed by a single surgeon between March 2010 and November 2012. All patients met the required inclusion criteria. A total of 36 breasts were evaluated by the photometric study recommended by Swanson22-24 that was performed preoperatively and 6 months postoperatively. The surgical procedure performed in both groups was similar, except for the preparation of a bipedicled strap of the pectoralis major muscle as follows:
As inclusion criteria, patients who underwent primary mammoplasty for the specific correction of breast ptosis or hypertrophy, had no previous history of breast surgeries, and had benign preoperative radiological findings (Breast Imaging-Reporting and Data System 1 and 2) participated in the study. Patients who provided informed consent and for whom photographic records of the preoperative and 6-monthpostoperative period according to the standardization adopted by the surgeon were also included.Group I, nine patients (18 breasts) who underwent mastopexy without a strap between March 2010 and December 2011. Group II, nine patients who underwent mastopexy with a strap between January 2012 and November 2012.
Mammoplasty surgical procedure using a muscle strap
Skin marking follows the recommendations of Wise2 and Pitanguy3 (inverted "T"). With the patient sitting, we marked the "A" point on a vertical line, drawn from the mid-clavicular distance to the areola at the mid-humeral level (usually at a distance of 18-21 cm from the sternal wishbone). Using the "bimanual pinch test," points B and C are defined at 10 cm from point A. The lower amount of breast tissue to be medially resected is defined using a manual pinching maneuver of point B to the point marked on the midline of the hemothorax at the level of the mammary groove. The same maneuver is applied at point C to define the lower amount of breast to be laterally resected (Figure 1).
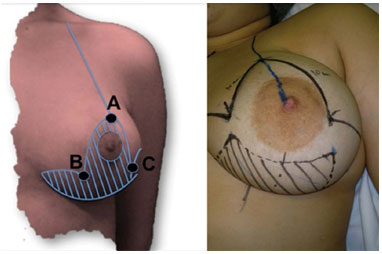
Figure 1. Preoperative skin marking.
After being marked, the skin is removed from the area around the areola and the central region of the inferior pole of the breast (Figure 2A, left breast). The lateral triangles of the dermoglandular flap are resected as well as the deep layer of these flaps, leaving a thickness of 1.5-3 cm from the second costal arch.
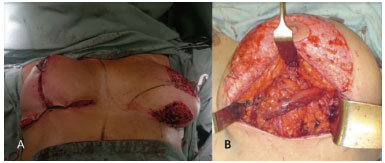
Figure 2. A: Left breast: De-epidermized skin around the areola and in the inferior dermoglandular pedicle. The skin areas marked between the de-epidermized skin and the ink markings were ultimately removed. Right breast: Final appearance of the inverted "T" scar. B: Lower dermoglandular pedicle under the muscle strap of the pectoralis major muscle.
Next, an area of bipedicled fascia 3 cm wide and approximately half of the pectoralis major muscle thick is elevated in the direction of its muscle fibers and close to the dermoglandular flap in the inferior central region of the breast. The deep half of the pectoralis major muscle is closed with continuous and non-absorbable sutures to ensure the integrity and precise delimitation of the muscular and glandular planes. The dermoglandular flap is passed beneath the bipedicled strap and fixed to the muscular fascia superiorly and centrally with non-absorbable sutures (Figure 2B).
The areola is laterally released and maintained by the superficial mediosuperior vascular pedicle. It follows a lateral and superior rotation to its lateral end on the previously marked point A (Figure 3).
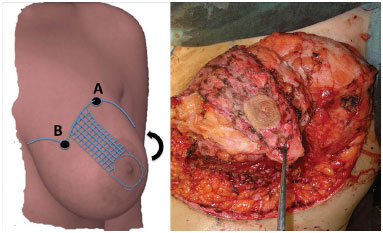
Figure 3. Marking of the mediosuperior pedicle, which will be rotated laterally and superiorly and then fixed to point A after de-epidermization of the skin containing the vascular pedicle (left figure, checkered blue area). The entire skin area marked between the de-epidermized skin of the pedicle and the ink marking was ultimately removed.
Finally, the medial and lateral pillars of the breast parenchyma are approached with two non-absorbable sutures and the skin is closed by moving points B and C to the hemithorax midline in the mammary groove (Figure 2A, right breast).
Data collection
The spreadsheets were created in Excel for Mac 2011 (Microsoft; Redmond, WA, USA) and a database was constructed. Information pertaining to patients and surgical procedures was initially collected. Data referring to postoperative evaluations were obtained by the author through standardized images recorded by a Sony-α290 (Sony Corporation, Tokyo, Japan) photographic camera positioned on a tripod at the patient's mid-humeral level at a fixed distance of 1.5 meters with a focal length of 35 mm, using a Sony-α DT3.5-5.6/18-55 mm SAM lens (Sony Corporation). These pictures were taken in the preoperative and 6-month postoperative period from each patient's right, left, right oblique, left oblique, and frontal directions.
Using Photoshop CS4 for Mac (Adobe, San Jose, CA, USA), following the conversion of pixels into centimeters of all 72 pictures recorded in the profile, the parameters previously defined by Swanson22-24 were studied as described below.
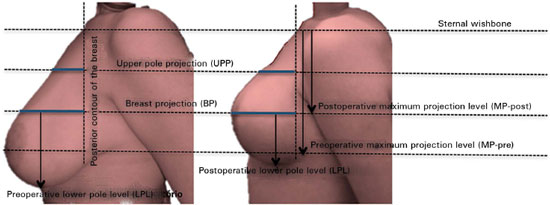
Collected measurements of each breast studied with photographs in the preoperative and postoperative profile (Figure 4)
Maximum postoperative projection level (MPpost): vertical distance measured in the posterior breast line from the sternal wishbone to the level where the highest postoperative breast projection is observed;
Upper pole projection (UPP): horizontal measure taken from the posterior breast line to the anterior thorax line at the mid-distance drawn between the sternal wishbone to the MP-post;
Breast projection (BP): horizontal measure taken from the posterior to the anterior breast line at the MP-post;
Maximum preoperative projection level (MPpre): vertical distance measured in the posterior breast line from the sternal wishbone up to the MP-post;
Lower pole level (LPL): vertical distance from the maximum postoperative projection (MP-post) to the inferior breast line;
Upper pole area (UPA): area delimited posteriorly by the posterior breast line, anteriorly by the anterior breast line, and in the lower region by the horizontal line drawn at the MP-post;
Lower pole area (LPA): area posteriorly delimited by the posterior breast line, anteriorly and in the lower region by the anterior and inferior breast lines, respectively, and superiorly by the horizontal line drawn at the MP-post;
Convexity: ratio between the UPP and BP (UPP/ BP);
Parenchyma ratio (PR): ratio between the UPA and LPA (UPA/LPA);
Elevation of the BP (EP): difference between the MP-pre and MP-post (MP-pre - MM-post).
Statistical analysis
To describe the characteristics of the breasts included in the study and data collected during the performed procedures, descriptive statistics of average, standard deviation, minimum, and maximum for continuous variables and frequencies for categorical variables was used. The statistical analysis of continuous variables initially used the Kolmogorov-Smirnov test to analyze whether the results followed a normal distribution. Continuous variables with a normal distribution were compared using Student's t test with average, standard deviation, and 95% confidence interval, while non-normally distributed variables were evaluated by the Mann-Whitney U test with median and quartiles. Categorical variables were statistically analyzed by Fisher's exact test.
To compare the average values resulting from the photometric study, we analyzed the values corresponding to the percentage EP (%EP), percentage convexity (%conv), and PR of each breast between the preoperative and 6-month postoperative periods. The 5% level of significance was adopted. SPSS 20 for Mac was used for the data analysis (IBM; Armonk, NY, USA).
RESULTS
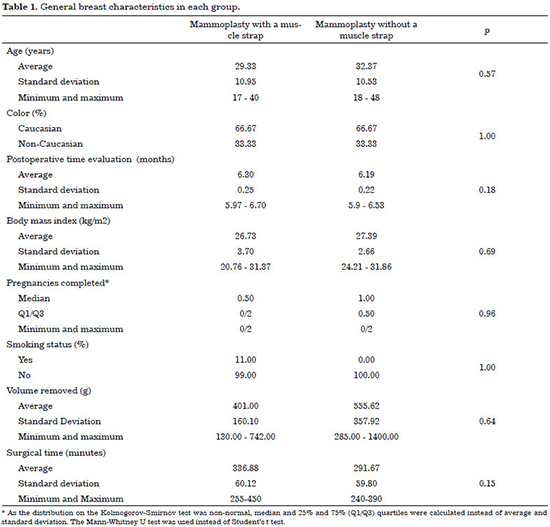
The study population was predominantly Caucasian and the distribution was similar in the two groups (33.33% of non-Caucasians in each group). The average age was 29.33 ± 10.95 years in the group treated with a muscle strap (Group I) and 32.37 ± 10.52 in the group treated without a muscle strap (Group II) (Table 1).
The body mass index (BMI) did not differ between groups at 26.73 ± 3.7 kg/m2 and 27.39 ± 2.66 kg/m2 for the group with and without a muscle strap, respectively. The number of pregnancies completed in both groups was similar, with median and quartiles of 0.5 (Q1 = 0 and Q3 = 2) in Group I and 1 (Q1 = 1 and Q3 = 2) in Group II. The average volume removed from each breast was 401.00 ± 160.10 g in mammoplasty with a muscle strap and 555.62 ± 257.92 g in mammoplasty without a strap, which did not represent a statistically significant difference. The average time of surgery in the groups with and without a muscle strap was 336.88 ± 60.12 minutes and 291.67 ± 59.80 minutes, respectively, without any significant difference (Table 1).
Regarding clinical complications, Group I and Group II each included one patient with scar hypertrophy in both breasts (Figure 5) and one patient with partial areolar epitheliosis in one breast (Figure 6). The two patients with epitheliosis in one breast each were clinically treated, and they experienced good healing without the need for a surgical procedure or tattoo. Therefore, the percentage of complications observed in this study included three mild (one epitheliosis and two hypertrophy) in the 18 breasts of each group (16.66%).

Figure 5. Pre- and 6-month-postoperative time points showing the efficacy of the muscle strap in increasing upper pole projection and enabling effective breast projection elevation. In this patient, the skin areolate flaps are maintained with a thickness of approximately 1.5 cm. This patient is a representative case of bilateral scar hypertrophy that was due to a possible reaction to the surgical suture that manifested from a 1-month postoperative period (more severe in the right breast).

Figure 6. Pre- and 6-month-postoperative time points in an obese patient. In this case, a thicker skin areolate flap (approximately 3 cm) is left despite increased upper pole projection and the greatly increased breast projection elevation provided by the muscle strap. Increased sliding is observed here compared to that in breasts with thinner cutaneous flaps. The patient presented with epitheliosis of the right nipple that resulted in local hypochromia that the patient did not wish to correct or cover with a tattoo.
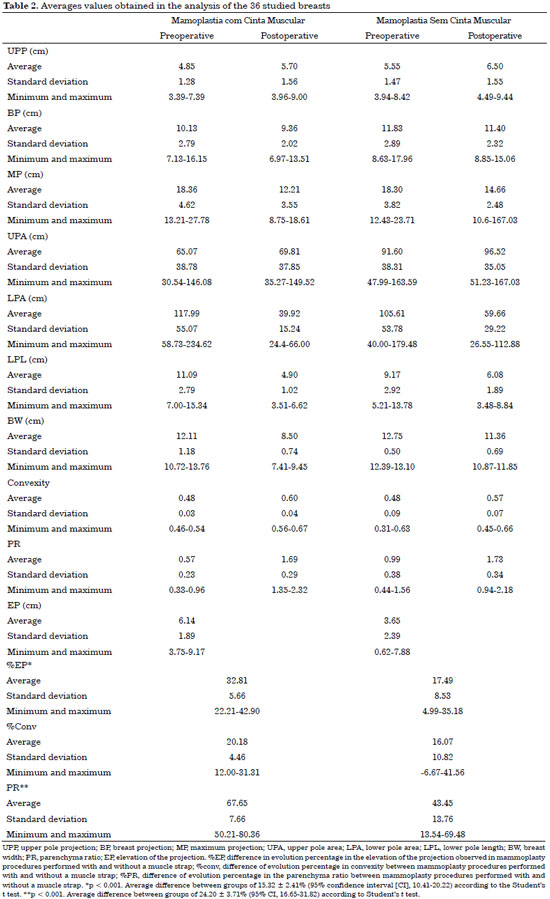
In the analysis of the results studied with each technique, the distribution of the values appeared normal in both groups according to the Kolmogorov-Smirnov test (Figure 7). Table 2 shows that the convexity improvement was 4.11% higher in patients in Group I compared to those in Group II. However, this difference was not statistically significant. Regarding %EP, the improvement was 17.49 ± 8.53% in Group I vs. 32.81 ± 5.66% in Group II, representing a significant average improvement of 15.32 ± 2.41% (p < 0.001, CI95% of 10.41 to 20.22) when using muscle strap. The same was observed in the UPP, represented by the average improvement in PR, which was 24.2 ± 3.71% higher (p < 0.001, 95% CI of 16.65 to 31.82) in Group I than in Group II (Table 2).

Figure 7. Normal distribution between dependent variables analyzed accordingly to the Kolmogorov-Smirnov test, which identified the maintenance of a proper standard in each group and consistency of photometric measurements obtained. A, Percentage of breast projection elevation improvement in the group treated with muscle strap; B, Percentage of breast projection elevation improvement in the group treated without a muscle strap; C, Percentage of breast convexity improvement in the group treated with a muscle strap; D, Percentage of breast convexity improvement in the group treated without a muscle strap; E, Percentage of improvement in the ratio between the upper and lower breast poles in the group treated with a muscle strap. F, Percentage of improvement in the ratio between the upper and lower breast poles in the group treated without a muscle strap.
DISCUSSION
The general variable analysis of the study population was similar between the groups with regards to age, BMI, race, smoking status, number of pregnancies, and breast volume resected during surgery. Therefore, in both groups, the influence of any characteristic of the women themselves other than the variable studied (muscle strap) can be considered low and the number of cases studied is sufficient since an important statistically significant difference between variables such as %EP and PR was found. The results followed a normal distribution, which seems characteristic of each group and confirms the consistency of the photometric values and discards the probability that these results were obtained by chance.
The 6-month-postoperative time point was the same used by many authors in different case series and considered suitable for this study20,23-25. As this study included a comparative analysis (mammoplasty without a muscle strap), it allowed for refining of the evaluation and comparison of the independent variable studied (muscle strap) within a 6-month postoperative period.
Although the surgical time was longer in Group I, the difference was not significant. In addition, the procedure performed with the muscle strap presented the exact same complication percentages and types as the group without.
The photometric results of Group I showed that this procedure effectively contained the dermoglandular pedicle of the inferior pole within a 6-month postoperative period. This study showed a significantly higher difference in the ratio between the upper and lower breast poles in Group I as well as a greater breast projection height (Table 2, Figures 5 and 8). Regarding the ptosis that persisted in the breasts of Group I, we believe that this was mainly due to sliding of the lipoglandular components of the skin flaps covering the lower pole pedicle and the superomedial areolate pedicle. Therefore, it is important that these flaps not be very thick and that the post-mammoplasty breast volume be predominantly comprised of the inferior pedicle enclosed within the muscle strap.

Figure 8. Pre- and 6-month-postoperative time points of a patient treated with a muscle strap with a predominantly fat parenchyma and intense sagging skin as well as a great number of stretch marks. In this patient, skin flaps are left with a thickness of approximately 3 cm. The muscle strap provides good filling of the upper pole and great elevation of the breast projection as assessed by the photometric results.
Our preference of using a superolateral areolate pedicle flap is not due to the initial purposes described, namely for filling of the upper pole9,10; as in the technique reported in this study, it is prepared with a thickness of 1.5-3.0 cm, which is sufficient to maintain skin vascularization26. This is mainly due to the extensive vascularization observed in this areolar segment (presenting as a dominant vascular pedicle with the perforating vessels of internal breast arteries/veins and a higher risk of areolar necrosis26,27) and the fact that it enables great areolar mobility, mainly in large and dense breasts, thus enabling the prevention of their tension and deformation1.
Regarding evaluation of the results, in 2011, Swanson22-24 developed an objective instrument that did not rely upon an evaluator's subjective opinion and allowed for the analysis and comparison of measurements obtained in breast surgeries. This instrument enabled the comparison of different mammoplasty techniques used to treat the same breast deformity and proved to be a versatile and reliable tool that provided accurate results by properly comparing different times (pre- and postoperative appearance of the same breast) and techniques (with and without a muscle strap). This was confirmed in the present study when the cases subjectively defined as having good results were not positively evaluated by Swanson's photometric assessment22-24; rather, this was subsequently confirmed using a more detailed visual evaluation (Figure 9).
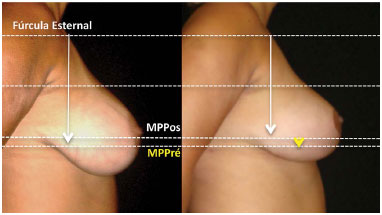
Figure 9. Pre- and 6-month-postoperative time points of a patient who presented with a fat breast that was treated without a muscle strap. On subjective photographic visualization, due to shape improvement, the evolution of the breast could have been considered satisfactory. The patient is quite satisfied with the results; however, the objective photometric analysis method proposed by Swanson22-24 identified it as the worst breast of the study. Careful examination shows that, despite the improved lower pole length obtained by surgery, the evolution is minimal in the projection elevation (MP-pre - MPpost, represented by the yellow arrow) and breast convexity (the upper pole is concave due to the lack of filling), probably due to sliding of the lipoglandular component of the inferior pedicle despite its dermal component remaining fixed to the upper pole.
In a subjective evaluation of patients and/or pictures, the evaluators focused their attention mainly on the breast shape and less on projection and the correlation between the upper and lower poles. It is rarely possible to only visually compare the evolution of the breasts from the pre- to postoperative period. Therefore, breast shape improvement over projection positioning and the correlation between the upper and lower poles (breast ptosis) are valued (Figure 9).
The main limitation of this study was its retrospective nature in addition to its non-controlled and randomized design. A postoperative period > 1 year might bring additional information regarding the influence of a muscle strap on late maintenance of the result presented herein, which was not the main objective of this study. Therefore, a higher number of patients might provide further details, such as the confirmation of improved breast convexity with muscle strap treatment and the detection of a longer surgical time required by this technique.
CONCLUSION
This study's findings proved that the use of a muscle strap effectively fills the upper pole of the breast and maintains its projection at the highest level, significantly reducing the degree of breast ptosis for up to 6 months after mammoplasty.
REFERENCES
1. Sinder R. História da mamoplastia redutora. In: Mélega JM, Baroudi R, eds. Cirurgia plástica: fundamentos e arte. Rio de Janeiro: Medsi; 2003. p.435-69.
2. Wise RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg (1946). 1956;17(5):367-75. DOI: http://dx.doi.org/10.1097/00006534-195605000-00004
3. Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20(1):78-85. PMID: 5339723 DOI: http://dx.doi.org/10.1016/S0007-1226(67)80009-2
4. Goulian D Jr. Dermal mastopexy. Plast Reconstr Surg. 1971;47(2):105-10. PMID: 4925049 DOI: http://dx.doi.org/10.1097/00006534-197102000-00001
5. Hinderer UT. The dermal brassiere mammaplasty. Clin Plast Surg. 1976;3(2):349-70.
6. Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97(2):373-80. DOI: http://dx.doi.org/10.1097/00006534-199602000-00015
7. Lockwood T. Reduction mammaplasty and mastopexy with superficial fascial system suspension. Plast Reconstr Surg. 1999;103(5):1411-20. PMID: 10190437 DOI: http://dx.doi.org/10.1097/00006534-199904020-00009
8. Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55(3):330-4. DOI: http://dx.doi.org/10.1097/00006534-197555030-00010
9. Silveira-Neto E. Mastoplastia redutora setorial com pedículo areolar interno. XIII Congresso Brasileiro de Cirurgia Plástica. Porto Alegre; 1976.
10. Losken A, Holtz DJ. Versatility of the superomedial pedicle in managing the massive weight loss breast: the rotation-advancement technique. Plast Reconstr Surg. 2007;120(4):1060-8. DOI: http://dx.doi.org/10.1097/01.prs.0000278004.24650.e6
11. Daniel MJB. Mamoplastia com Músculo Peitoral. XXXI Congresso Brasileiro de Cirurgia Plástica. Curitiba; 1993.
12. Caldeira AM, Lucas A. Pectoralis major muscle flap: a new support approach to mammaplasty, personal technique. Aesthetic Plast Surg. 2000;24(1):58-70. DOI: http://dx.doi.org/10.1007/s002669910011
13. Goebell R. Ueber autoplastische freie Fascien- und Aponeurosentransplantation nach Martin Kirschner. Arch Klin Chir. 1927;146:462-509.
14. Graf R, Auersvald A, Bernardes A, Biggs TM. Reduction mammaplasty and mastopexy with shorter scar and beter shape. Aesth Surg J. 2000;20(2):99-106.
15. Graf R, Biggs TM, Steely RL. Breast shape: a technique for better upper pole fullness. Aesthetic Plast Surg. 2000;24(5):348-52. DOI: http://dx.doi.org/10.1007/s002660010057
16. Graf R, Biggs TM. In search of better shape in mastopexy and reduction mammoplasty. Plast Reconstr Surg. 2002;110(1):309-17. DOI: http://dx.doi.org/10.1097/00006534-200207000-00053
17. Graf R, Reis de Araujo LR, Rippel R, Neto LG, Pace DT, Biggs T. Reduction mammaplasty and mastopexy using the vertical scar and thoracic wall flap technique. Aesthetic Plast Surg. 2003;27(1):6-12. DOI: http://dx.doi.org/10.1007/s00266-002-0111-5
18. Graf R, Araujo LRR, Rippel R, Graça Neto L, Pace DT, Biggs T. Mamaplastia vertical com retalho de parede torácica. Rev Soc Bras Cir Plást. 2005;20(3):148-54.
19. Ritz M, Silfen R, Southwick G. Fascial suspension mastopexy. Plast Reconstr Surg. 2006;117(1):86-94. PMID: 16404254 DOI: http://dx.doi.org/10.1097/01.prs.0000194919.22522.63
20. Hall-Findlay EJ. The three breast dimensions: analysis and effecting change. Plast Reconstr Surg. 2010;125(6):1632-42. PMID: 20517086 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181ccdb97
21. Tolazzi ARDO, Graft RM, Freitas RS, Cruz GAO. Avaliação da influência da cinta muscular peitoral na sustentação do retalho dermolipoglandular mamário após mamoplastia vertical. Rev Bras Cir Plást. 2010;25(1):141-52.
22. Swanson E. A measurement system for evaluation of shape changes and proportions after cosmetic breast surgery. Plast Reconstr Surg. 2012;129(4):982-92. DOI: http://dx.doi.org/10.1097/PRS.0b013e3182442290
23. Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011;128(6):1282-301. DOI: http://dx.doi.org/10.1097/PRS.0b013e318230c884
24. Swanson E. Prospective photographic measurement study of 196 cases of breast augmentation, mastopexy, augmentation/ mastopexy, and breast reduction. Plast Reconstr Surg. 2013;131(5):802e-19e. PMID: 23629120 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182865e20
25. Strombeck JO. Mammaplasty: report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79-90. PMID: 13835285 DOI: http://dx.doi.org/10.1016/S0007-1226(60)80014-8
26. le Roux CM, Pan WR, Matousek SA, Ashton MW. Preventing venous congestion of the nipple-areola complex: an anatomical guide to preserving essential venous drainage networks. Plast Reconstr Surg. 2011;127(3):1073-9. PMID: 21364409 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182044bb2
27. Başaran K, Ucar A, Guven E, Arinci A, Yazar M, Kuvat SV. Ultrasonographically determined pedicled breast reduction in severe gigantomastia. Plast Reconstr Surg. 2011;128(4):252e-9e.
1. Instituto de Cirurgia Plástica Santa Cruz, São Paulo, SP, Brazil
2. Universidade Estadual de Campinas, São Paulo, SP, Brazil
3. Consultório Dr. Francisco Claro Jr., São Paulo, SP, Brazil
Institution: Consultório Dr. Francisco Claro Jr. São Paulo, SP, Brazil.
Corresponding author:
Francisco Claro de Oliveira Jr
Av. Indianópolis, 2244
São Paulo, SP, Brazil Zip Code 04062-002
E-mail: drfrancisco@franciscoclaro.com
Article received: July 16, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter