

Original Article - Year 2015 - Volume 30 -
Anchor dermolipectomy after bariatric surgery: complications and patient satisfaction rate
Dermolipectomia em âncora após cirurgia bariátrica: complicações e índice de satisfação dos pacientes
ABSTRACT
INTRODUCTION: Obesity is designated by the World Health Organization (WHO) as the major pandemic of this century. Bariatric surgery is one of the most effective treatments of morbid obesity, since most patients are submitted to reconstructive plastic surgery after major weight loss. Among the surgeries carried out in the formerly obese, dermolipectomy is the procedure that is mostly associated with complications after surgery. The aim of this study was to report the experience of the author in performing anchor dermolipectomy after major weight loss, focusing on complications and patient satisfaction rate.
METHODS: The medical records of 40 patients operated between September 2011 and April 2013 were reviewed in the study. Five patients were excluded from the study, since they could not be found. The patients were asked to score their satisfaction from 1 to 4, where 1 means dissatisfied, 2 poorly satisfied, 3 satisfied, and 4 very satisfied. Trans and post-operative complications, surgical time, hospital stay, drainage time, age, and gender were considered in the study. The data obtained were submitted to a statistical analysis and descriptive statistics.
RESULTS: Among the 35 patients evaluated in our study, only one was male (2.85%). The age varied between 27 and 68 years (average age of 41.25 years). The preoperative weight varied from 58 to 108 kg (average of 73.6 kg); 94.28% of the patients declared themselves as satisfied (score 3 and 4). The main complication was the occurrence of seroma (28.5%), followed by hypertrophic scar (17.14%). No major complication was observed. The average surgical time was 103 minutes (75-140 minutes). The patient was discharged 24 hours after hospital admission.
CONCLUSION: Anchor dermolipectomy is a safe and effective body contouring procedure to be carried out in the formerly obese.
Keywords: Abdominoplasty; Bariatric surgery; Postoperative complications; Patient satisfaction.
RESUMO
INTRODUÇÃO: A obesidade é considerada pela Organização Mundial de Saúde (OMS) a principal pandemia do século. A obesidade mórbida tem como um de seus tratamentos mais efetivos a cirurgia bariátrica, e muitos pacientes necessitarão de cirurgia plástica reparadora após grandes emagrecimentos. Dentre as cirurgias em ex-obesos, a mais associada a complicações é a dermolipectomia. O propósito deste estudo foi mostrar a experiência do autor na dermolipectomia em âncora após grande emagrecimento, enfocando as complicações e a satisfação do paciente.
MÉTODOS: Revisamos 40 prontuários de pacientes operados entre setembro de 2011 e abril de 2013, cinco deles não foram localizados e, por isso, excluídos do estudo. Foi solicitado que pontuassem de 1 a 4, sendo 1 (insatisfeito), 2 (pouco satisfeito), 3 (satisfeito), 4 (muito satisfeito). Consideramos as complicações trans e pós-operatórias, tempo cirúrgico, permanência hospitalar, tempo com dreno, idade e gênero. Foi realizada análise estatística dos dados, assim como estatística descritiva.
RESULTADOS: Nosso estudo avaliou 35 pacientes, apenas um era homem (2,85%), a idade variou de 27 a 68 anos (média 41,25 anos), o peso pré-operatório variou de 58 a 108 kg (média de 73,6 kg), 94,28% dos pacientes sentiam-se satisfeitos (pontuação 3 e 4). A principal complicação foi o seroma 28,5%, seguida pela cicatriz hipertrófica (17,14%), nenhuma complicação maior foi verificada. O tempo médio do procedimento cirúrgico foi de 103 minutos (75-140 minutos). Alta ocorreu com 24h de internação hospitalar.
CONCLUSÃO: A dermolipectomia em âncora é um método seguro e efetivo para o contorno corporal do ex-obeso.
Palavras-chave: Abdominoplastia; Cirurgia bariátrica; Complicações pós-operatórias; Satisfação do paciente.
At the beginning of the 20th century, Kelly1 started to perform abdominoplasty for the treatment of excess skin in the formerly obese. In the 1960s, changes in the procedure were reported by several authors, such as Castañares and Goethel, who proposed a vertical and horizontal resection, with an anchor-shaped final scar. In 1970, Regnault encouraged the removal of excess skin, in which the markings resembled a fleur-de-lis. Pitanguy developed a transverse abdominoplasty method, consisting of a large detachment of the abdominal flap and plication of the rectus abdominis muscles, in order to correct the diastasis2.
Obesity is currently considered by the World Health Organization as the main pandemic of the century3,4. In Brazil, data from IBGE (Brazilian Institute of Geography and Statistics) show that the prevalence of overweight and obesity is of approximately 50%, in both men and women, belonging to an age group of more than 20 years5. Currently, the most effective treatment for morbid obesity is bariatric surgery3,6-8, which is performed with the aim to achieve a long-term weight control and treatment of diseases that have obesity as a main risk factor2. Weight loss occurs within 12 to 18 months and the best time to carry out body contouring plastic procedures is between 18 and 24 months8.
The frequency of these surgeries increased significantly and many of these patients will need reconstructive plastic surgery4,9 to correct excess skin and sagging3,6,10. An enormous psychosocial impact is caused by widespread dermatochalasis, due to medical implications such as intertrigo and functional limitations in walking as well as performing physical and sexual activities10,11. Many of these patients are not treated properly by traditional dermolipectomy procedures that leave a horizontal scar10 and circumferential incisions lead to high rates of severe complications such as necrosis, large dehiscence, blood transfusions, prolonged hospitalization12,13. This resulted in the revival of anchor dermolipectomy technique12.
Several controversies exist in the literature about the Predictive factors of Complications. The percentage of excess weight loss, smoking, diabetes mellitus and/ or SAH (hypertension), nutritional deficiency, ASA classification (American Society of Anesthesiology), total tissue removed, intraoperative time, combination of multiple procedures, maximum BMI (body mass index) and the change to the current BMI are variable risk factors14. Reliable data regarding the evolution and complications in this population group are still scarce in the literature.
Among the surgeries carried out in formerly obese patients, abdominoplasty is the procedure more often associated with complications14. The preoperative evaluation of these patients should include a careful study to determine anemia, electrolyte changes, and nutritional disorders. A meticulous physical examination and search for hernias and stable proper clinical, psychological and nutritional conditions3 is also required.
OBJECTIVE
The purpose of this study was to show the experience of the author in anchor-line abdominoplasty, carried out after major weight loss and after bariatric surgery. Focusing the study on possible complications, we compared the data obtained with the satisfaction rates found in the literature, verifying the degree of patient satisfaction and drawing the attention on the importance of diminishing the hospitalization stay and surgical time.
METHODS
This is a retrospective study including 35 patients who underwent bariatric surgery and abdominoplasty, performed by the same surgeon in a private hospital, between September 2011 and April 2013. Forty medical records were reviewed with the aim of observing trans- and post-operative complications, surgical time, hospital stay, suction drainage time, age, and gender. The patients were contacted to request their permission for the inclusion in the study and inquired about their satisfaction in relation to the surgery. Five patients were not found and, therefore, excluded from the study. The database was evaluated using statistical parametric and nonparametric tests as well as techniques of descriptive statistics, with the aim of comparing the results of multiple variables and obtaining valid information to address the questions associated with the objective of the study.
Statistical analysis of sample data was performed using nonparametric tests, such as Wilcoxon Mann-Whithney, G3 de Wilks test, and Association Coefficients measures. We also applied other parametric tests, such as difference ratio test and z test and t-test to evaluate single group and average differences, respectively.
Several techniques of descriptive statistics were also employed to calculate values of descriptive statistics as well as for graph construction, in view of the fact that these complement and support statistical analyses.
In the calculations performed, XLSTAT-PRO (win-upgrade) software, version 10, from ADDINSOFT was used, in addition to the resources available in Microsoft Excel.
To assess the rate of satisfaction, the patients were asked to provide a score ranging from 1 to 4, with 1 being dissatisfied, 2 poorly satisfied, 3 satisfied, and 4 very satisfied.
A minimum period of 1.5 years after bariatric surgery and more than 4 months of weight stability was required for dermolipectomy to be indicated to the patients.
All patients were monitored by a multidisciplinary team and operated only upon the consent of an endocrinologist, a nutritionist, a psychologist, a psychiatrist, and a general surgeon that performed bariatric surgery. All patients were operated when presenting a hemoglobin value higher than 11 mg/dl, vitamin B12 and folic acid within normal range, and albumin higher than 3.5 mg/dl. When patients were not meeting these requirements, they were re-directed to an endocrinologist and nutritionist for preoperative replacement. The surgical technique employed was the combination of vertical and horizontal resection with an anchor-shaped final scar; no detachment of the flaps was carried out as recommended by Roxo et al.12 and Resende15.
All surgery site markings were made before entering in the operating room, with the patient in supine position, by clamping the redundant tissue and subtracting the subcutaneous tissue thickness to prevent tension on the flaps. With the traction of the tissue, the horizontal scar was about 6 cm from the vaginal wishbone and directed towards the iliac anterosuperior spines. The plication of the aponeurosis on the rectus abdominis muscle was performed in all patients with 0 polypropylene suture and the presence of hernias were corrected by the team in the same surgery. The closure of the abdominal wall was carried out by planes: subcutaneous and subdermic, with simple altered suture carried out using 2.0 and 3.0 mononylon, respectively, and the skin with continuous simple suture carried out with 4.0 mononylon. A suction drain was placed in all patients. Dressings with padded compresses and bandages were not removed for 4 days and then exchanged for elastic strap for a period of 60 days. The sutures were removed between 10 and 17 days, and then a silicone tape was placed on the scars, while they were red.
The patients were monitored for at least 3 months, with variable frequency.
RESULTS
Thirty-five patients were evaluated and only one patient was male (2.85%). The age varied between 27 and 68 years old. The preoperative BMI varied between 21.69 and 38.84 kg/m2, the percentage of weight lost on bariatric surgery ranged from 26.5 to 53.4% (average of 41.8%) and the average weight at the time of surgery varied from 58 to 108 kg (average of 73.6 kg). The average surgical time was 103 minutes, varying from 75 to 140 minutes (Figure 1).
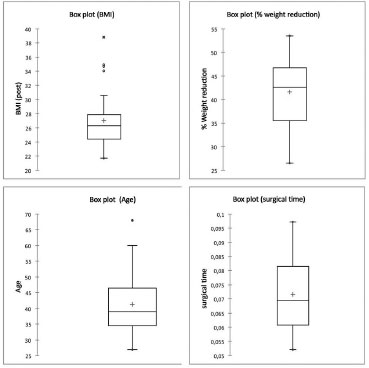
Figure 1. Distribution of the studied population. * Numerical factors replacing hours: 0.05 = 01:12 h/ 0.1 = 02:24 h. BMI: Body Mass Index.
Antibiotic prophylaxis was performed with 1 g intravenous cefazolin, for anesthetic induction, and 500 mg oral cephalexin 6/6 h per 7 days, which was administered to all patients. Deep vein thrombosis (DVT) prophylaxis was carried out with 40 mg subcutaneous clexane and administered 6 hours after the procedure, encouraging early ambulation as soon as the patient recovered from anesthesia. No case of DTV prophylaxis was observed. Catheter-delay bladder was not used. No cases of hematoma were detected or observed as needing blood transfusion. No infection of the surgical site was observed. There was no sutures dehiscence, either small or large, or the presence of flaps necrosis.
All patients were discharged 24 hours after hospital admission, with the drain removed when the flow was less than 40 ml/24 h, i.e., in about 9.6 days (3-15 days).
The main complication was the occurrence of seroma (28.5%), solved with a maximum of 4 punctures carried out in the office, followed by hypertrophic scar (17.14%) (Figure 2). Two patients required a second surgery to correct excess skin (dog ear) and was awaiting correction of residual sagging in the upper abdomen. Most of the patients (94.28%) were satisfied or very satisfied with the results obtained (Figures 3 and 4).
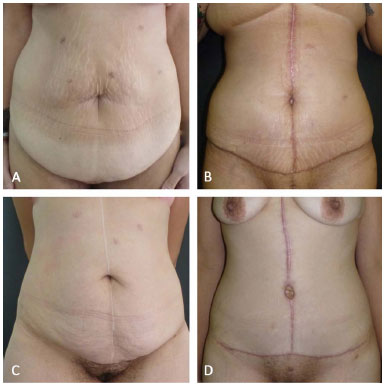
Figure 2. Hypertrophic scars (A and C - pre-operative, B and D - post-operative).
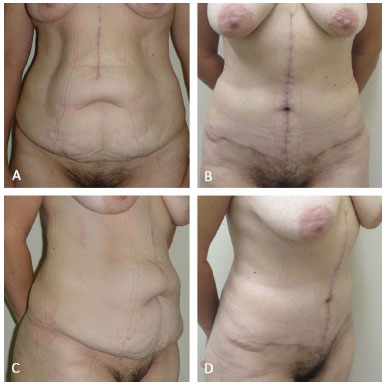
Figure 3. A and C (pre-operative); B and D (6 months after surgery).
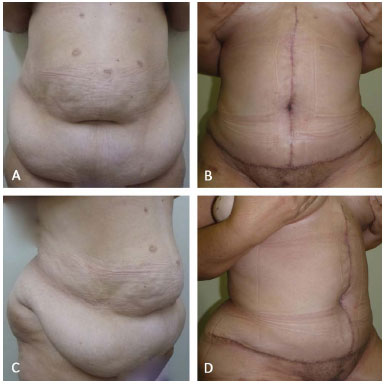
Figure 4. A and C (pre-operative); B and D (post-operative, 4 months).
DISCUSSION
Obesity is a growing global problem, with significant morbidity, mortality, and psychosocial issues. The popularity of bariatric surgery resulted in an increased demand for aesthetic and functional surgery11,14.
Plastic surgery procedures can improve the quality of life. However, the high complication rates might reverse these potential gains14. In the literature, many studies report high rates of complications in post-bariatric dermolipectomies, such as 50.4%3, 43%6, 60%16, increasing significantly the cost of the procedure17. In addressing these patients, we should be aware of the clinical peculiarities of these individuals and risk of complications, which are higher than in non-obese patients1. A stable preoperative weight for a period of 3 months is associated with a significant reduction in the complications rate14, which was also observed in our study. Further complications are also observed in patients with residual obesity, where the rates reach 35% in non-obese and up to 80% in patients maintaining some degree of obesity7.
The importance of weight maintenance is supported by van der Beek and based on the aim to avoid a hypercatabolic state of weight loss that could affect healing. Bariatric surgery can also lead to nutritional deficits18 due to malabsorption and insufficient food intake, wherein nutritional guidance is critical to avoid dehiscence and infections. In a study published by Agha-Mohammadi and Hurwitz8, nutritional supplementation was shown to reduce the complication rate from 66 to 18.9%. In this study, we observed no dehiscence, infection or hematomas, and the meticulous monitoring carried out by the nutrition and endocrinology team is of great help to these results.
Vitamin deficiencies, major changes in living standards, difficulty in performing physical activity and establishing personal relationships, caused by a shame feeling due to excess sagging skin left over18, can lead to severe psychiatric disorders. This rendered essential the monitoring and discharge of these patients by the psychiatrist and psychologist7.
In the last decade, the concept of body lifting has been developed. These procedures are based on identifying the primary deformity in the upper, medium, or lower abdomen, and sometimes on the back19.
When extensive abdominal liposuction is performed in combination with an open surgery, it might compromise skin vessels13, especially with large anchor incisions. Several studies show that liposuction procedures should be avoided in patients with biliopancreatic derivation, due to the histological changes triggered by the surgery8. It is a common procedure for us to avoid skin flaps liposuction in these patients, since we limit to carry out small suctions on the flanks after the procedure, when necessary. We also avoid flaps tension and these practices contributed to the absence of necrosis in our series.
Previous studies showed that body lifting is associated with high rates of complications, such as development of seroma, pulmonary embolism, wound necrosis, and need for blood transfusions13,14. Lengthy surgery with complete inactivity of the lower limb increases gradually the likelihood of stasis and thrombosis with an increased surgical time16. Our surgical time is significantly lower when compared to the literature (p < 0.0001), thus contributing to the absence of complications such as DVT, infection and blood transfusion. Reduction of surgical time was possible since markings and discussion regarding these prophylactic actions were carried out before the patient entered the surgical center. It is also due to the liposuction performed and not to the combination of these procedures.
Numerous surgical factors can contribute to reduce complications: short operative period (reduces infections, DVT, blood transfusions), preferential use of a cold scalpel (decreases seroma formation), meticulous hemostasis (reduces the need for blood transfusions), short hospital stay (reduces infection rates and DVT), use of pneumatic compression boots, early mobilization, and drug prophylaxis (reduces the risk of thromboembolic phenomena)13. In our patients, we identified most of these factors and the absence of major complications described in the literature. However, we observed a rate of occurrence of seroma close to the upper limits (p = 0.07) probably due to the predominant use of electrocautery scalpel. However, these comparisons are difficult to make, as there is no standardization of the data analyzed14.
The evaluation of the results is complex in plastic surgery, since it involves subjective parameters and the dependency on few publications that can be compared to in the literature. However, this is necessary to ensure further improvements. In this study we had high rate of satisfaction, higher when compared to the literature (p = 0.02328).
Many articles show that the presence of complications does not affect satisfaction. Several studies show that weight gain decreases patient's satisfaction with the surgery performed. In our analysis, satisfaction is not related to BMI (p = 0.930). However, it is dependent on the presence of residual sagging (p = 0.046), which is usually associated (contingency coefficient = 0.402) (Figure 5).
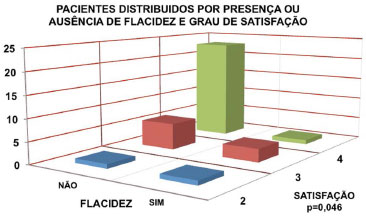
Figure 5. Patients distributed according to the presence or absence of sagging skin and degree of satisfaction.
Most patients with large weight losses present asymmetries17 in the preoperative period and the exact symmetry can be very difficult to achieve. This should be highlighted and reiterated to the patient before surgery, in order to increase the acceptance of the results. The scars and the possible complications and limitations of the procedure, such as the lack of elasticity and the possible residual sagging skin, should be very well described.
The literature is not unanimous on the linear correlation between BMI and complications. The percentage of excess weight lost before abdominoplasty is reported as an independent predictor of complications as well as the maintenance of a stable weight. Therefore, we should emphasize the importance to maintain the weight as much closer as possible to the ideal. Our study failed to prove the relationship between BMI and complications, highlighting that all patients were in stable weight for over 4 months.
CONCLUSION
Anchor dermolipectomy is a safe and effective procedure for body contouring of formerly obese patients. To optimize body contouring surgeries, it is mandatory to identify predictors of complications and satisfaction, while carefully selecting the patients. It has been demonstrated that it is possible to systematize surgical procedure with operative time and reduced hospitalization, in addition to maintaining high rates of satisfaction and absence of major complications.
REFERENCES
1. Kelly HA. Excision of the flat abdominal wall lipectomy. Surg Gynecol Obstet. 1910;10(229):18.
2. Lage RR, Amado BN, Sizenando RP, Heitor BS, Ferreira BM. Dermolipectomia abdominal pós-gastroplastia: avaliação de 100 casos operados pela técnica do "peixinho". Rev Bras Cir Plást. 2011;26(4):675-9. DOI: http://dx.doi.org/10.1590/S1983-51752011000400024
3. Cavalcante HA. Abdominoplastia após perda de peso maciça: abordagens, técnicas e complicações. Rev Bras Cir Plást. 2010;25(1):92-9.
4. Tuma Júnior P, Batista BPSN, Milan LS, Faria GEL, Milcheski DA, Ferreira MC. Abdominoplastia vertical para tratamento do excesso de pele abdominal após perdas ponderais maciças. Rev Bras Cir Plást. 2012;27(3):445-9. DOI: http://dx.doi.org/10.1590/S1983-51752012000300020
5. Brasil. Instituto Brasileiro de Geografia e Estatística. Síntese de Indicadores Sociais. Uma análise das condições de vida da população brasileira [Internet]. Rio de Janeiro: IBGE; 2012 [citado 2013 ago. 10]. Disponível em: ftp://ftp.ibge.gov.br/Indicadores_Sociais/Sintese_de_Indicadores_Sociais_2012/SIS_2012.pdf
6. Smaniotto PHS, Saito FL, Fortes F, Scopel SO, Gemperli R, Ferreira MC. Análise Comparativa da Evolução e das complicações pós-operatórias nas cirurgias plásticas do contorno corporal em pacientes idosos e jovens com perda ponderal maciça. Rev Bras Cirg Plást. 2012;27(3):441-4. DOI: http://dx.doi.org/10.1590/S1983-51752012000300019
7. Orpheu SC, Coltro PS, Scopel GP, Saito FL, Ferreira MC. Cirurgia do contorno corporal no paciente após perda ponderal maciça: experiência de três anos em hospital público secundário. Rev Assoc Med Bras. 2009;55(4):427-33. DOI: http://dx.doi.org/10.1590/S0104-42302009000400018
8. Agha-Mohammadi S, Hurwitz DJ. Potential impacts of nutritional deficiency of postbariatric patients on body contouring surgery. Plast Reconstr Surg. 2008;122(6):1901-14. PMID: 19050544 DOI: http://dx.doi.org/10.1097/PRS.0b013e31818d20d6
9. Larsen M, Polat F, Stook FP, Oostenbroek RJ, Plaisier PW, Hesp WL. Satisfaction and complications in post-bariatric surgery abdominoplasty patients. Acta Chir Plast. 2007;49(4):95-8. PMID: 18306644
10. Tardelli HC, Vilela DB, Schwartzmann GLE, Azevedo M, Mello Júnior AM, Farina Júnior JA. Padronização cirúrgica das abdominoplastias em âncora pós-gastroplastia. Rev Bras Cir Plást. 2011;26(2):266-74. DOI: http://dx.doi.org/10.1590/S1983-51752011000200013
11. Vico PG, De Vooght A, Nokerman B. Circumferential body contouring in bariatric and non-bariatric patient. J Plast Reconstr Aesthet Surg. 2010;63(5):814-9. DOI: http://dx.doi.org/10.1016/j.bjps.2009.01.075
12. Roxo CDP, Pinheiro O, Almeida D. Abdominoplastia multifuncional. Rev Bras Cir Plást. 2004;19(3):64-74.
13. Jones BM, Toft NJ. Bodylifting: indications, technique and complications. J Plast Reconstr Aesthet Surg. 2008;61(7):730-5. PMID: 18547885 DOI: http://dx.doi.org/10.1016/j.bjps.2008.04.012
14. van der Beek ES, van der Molen AM, van Ramshorst B. Complications after body contouring surgery in post-bariatric patients: the importance of a stable weight close to normal. Obes Facts. 2011;4(1):61-6. DOI: http://dx.doi.org/10.1159/000324567
15. Resende JHC. Tratamento cirúrgico complementar na obesidade mórbida. In: Mélega JM, ed. Cirurgia plástica: fundamentos e arte - cirurgia estética. Rio de Janeiro: Medsi; 2003. p.687-94.
16. Almeida EG, Almeida Júnior GL. Abdominoplastia: estudo retrospectivo. Rev Bras Cir Plást. 2008;23(1):1-10.
17. Michaels J 5th, Coon D, Rubin JP. Complications in postbariatric body contouring: postoperative management and treatment. Plast Reconstr Surg. 2011;127(4):1693-700. PMID: 21460677 DOI: http://dx.doi.org/10.1097/PRS.0b013e31820a649f
18. Highton L, Ekwobi C, Rose V. Post-bariatric surgery body contouring in the NHS: a survey of UK bariatric surgeons. J Plast Reconstr Aesthet Surg. 2012;65(4):426-32. PMID: 22015146 DOI: http://dx.doi.org/10.1016/j.bjps.2011.09.047
19. Kannan RY, Caddy CM. The 'hour-glass' abdominoplasty in massive weight loss surgery: a preliminary case series. J Plast Reconstr Aesthet Surg. 2009;62(5):e81-2. DOI: http://dx.doi.org/10.1016/j.bjps.2008.09.020
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Associação Brasileira de Cirurgia Craniomaxilofacial, São Paulo, SP, Brazil
Institution: Hospitais da Rede Particular do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Maieve Corralo Grando
Rua Santa Clara, 70/ 308, Copacabana
Rio de Janeiro, RJ, Brazil CEP 22041-900
E-mail: maieve@hotmail.com
Article received: July 8, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter