

Original Article - Year 2015 - Volume 30 -
Application of fat grafting in craniofacial deformities: an INTO-RJ experience
Aplicação da lipoenxertia nas deformidades craniofaciais: experiência do INTO-RJ
ABSTRACT
INTRODUCTION: The fat graft is currently widely used in aesthetic plastic and reconstructive surgery as a natural filler. In cranio-maxillofacial surgery, fat grafting can be very beneficial for patients with various congenital and acquired deformities.
METHODS: We included patients who had undergone fat grafting for reconstruction and correction of defects in the face during 2012 and 2013 by using a standard technique. Our assessment was both clinical and subjective, taking into account the patient's opinion. In patients with late enophthalmos secondary to trauma sequelae, we conducted exophthalmometry with an exophthalmometer (Hertel) and preoperative and postoperative CT to objectively evaluate our results.
RESULTS: Twenty-two patients were treated. Most were female (77%). The volume of fat grafted varied from 1 ml to 37 ml, with a mean of 15 ml per session. The number of sessions ranged from 1 to 4. Fat grafting was used as a single treatment in only 30% of cases. We performed retrobulbar fat grafting ranging from 6 to 10 ml in volume; in one patient, the grafting was carried out over two sessions. There was a gain of 3 to 7 mm in projection of the eyeball. In tomographic evaluation, an increased eye projection of between 2.2 mm and 4 mm was found. However, the clinical outcome was poor.
CONCLUSION: Fat grafting is a simple, inexpensive and reproducible procedure that should be part of the plastic and craniofacial surgeons' inventory. It may be an alternative in difficult cases of late enophthalmos.
Keywords: Grafts; Enophthalmos; Fat; Plastic, surgery.
RESUMO
INTRODUÇÃO: O enxerto de gordura, atualmente, é usado amplamente na cirurgia plástica estética e reparadora como um preenchimento natural. Na cirurgia crânio-maxilofacial há uma diversidade de pacientes com deformidades congênitas e adquiridas que podem ser muito beneficiados com a lipoenxertia.
MÉTODOS: Os pacientes foram submetidos à lipoenxertia para reconstrução e correção de defeitos da face no INTO em 2012 e 2013 utilizando uma técnica padronizada. Nossa avaliação foi clínica e subjetiva, levando em conta a opinião do paciente. Especificamente nos pacientes com enoftalmo tardio secundário à sequela de trauma, realizamos exoftalmometria com o exoftalmômetro de Hertel e tomografia no pré e no pós-operatório para avaliar objetivamente nossos resultados.
RESULTADOS: Vinte e dois pacientes receberam tratamento. A maioria foi do gênero feminino (77%). O volume do gordura aplicado variou de 1 ml até 37 ml, com média de 15 ml por sessão. A quantidade de sessões variou de 1 a 4. A lipoenxertia foi usada como tratamento único em apenas 30% dos casos. Fizemos lipoenxertia retrobulbar variando de 6 a 10 ml o volume enxertado, sendo que em um paciente realizamos duas sessões. Houve um ganho de 3 a 7 mm de projeção do globo ocular. Na avaliação tomográfica constatamos também aumento da projeção ocular de 4 mm e 2,2 mm. O resultado clínico foi pobre.
CONCLUSÃO: A lipoenxertia é um procedimento simples, barato e reprodutível que deve fazer parte do armamentário do cirurgião plástico e do cirurgião craniofacial. Pode ser uma alternativa nos difíceis casos de enoftalmo tardio.
Palavras-chave: Enxertos; Enoftalmia; Gordura; Cirurgia plástica.
The fat graft is currently widely used in plastic surgery and aesthetic restorative surgery as a natural filler, and is preferred over synthetic products on the market by many surgeons1-3. The preference for fat to treat volume defects and contour is because of it is an autologous tissue that is usually available and easy to obtain. A US survey showed that approximately 57% of American plastic surgeons perform at least 10 fat grafts annually, and that the vast majority of patients are satisfied with the short and long term results4. A major concern in fat grafting is the variability of graft integration into the recipient bed, making the results unpredictable; in general, engraftment varies from 40% to 80%5-10.
Cranio-maxillofacial surgery is a plastic surgery practice area with a diversity of patients with congenital and acquired deformities, which can benefit from procedures that restore craniofacial volume and contour.
This study aims to demonstrate the use of fat grafting in craniofacial deformities at the National Institute of Traumatology and Orthopedics (INTO-RJ) as an isolated treatment alternative or in combination with other surgical strategies, and to present our application methodology of fat grafting.
METHODS
Patients who underwent fat grafting for face reconstruction and defects correction at INTO-RJ in 2012 and 2013 using a standard technique were included in the study.
We did not conduct any examination of pre and postoperative imaging in order to quantify the engraftment or our results. Our assessment was both clinical and subjective, taking into account the patient's opinion. In patients with late enophthalmos secondary to trauma sequelae, we additionally conducted exophthalmometry with an exophthalmometer (Hertel) and preoperative and postoperative CT to objectively evaluate our results.
Extraction
We collected fat from the anterior abdomen and flanks with the patient in the supine position. These areas offer easily accessible fat, avoiding unnecessary increases to the surgical time and, in addition, using these areas may result in some improvement in body contour of the patient. The literature does not list any donor areas with increased viability for fat grafting. The quantity of suctioned fat is 50% higher than the estimated requirements for grafting. We do not collect more than anticipated to obtain further aesthetic results in the donor area.
The incisions are made into folds, previous scars, stretch marks, or hairy regions, whenever possible. We administer (using a Klein cannula) an epinephrine solution 1:500,000 in donor areas in a 1:1 ratio (1 ml solution per 1 ml of suctioned fat). Fat aspiration is performed with a blunt cannula of 2.5 or 2.7 mm attached to a 10 ml syringe (Figure 1).

Figure 1. Fat extraction from the flank and anterior abdomen.
Processing
The syringes with 10 ml of suctioned fat are capped with a silicone stopper and centrifuged for 3 minutes at 3,000 rpm (Figure 2). The upper layer, composed of oil, is collected. The lower one composed of "water" is discarded. The fat is kept in the syringes without further manipulation (Figure 3).
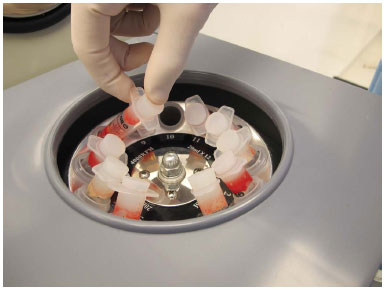
Figure 2. Processing with fat centrifugation.
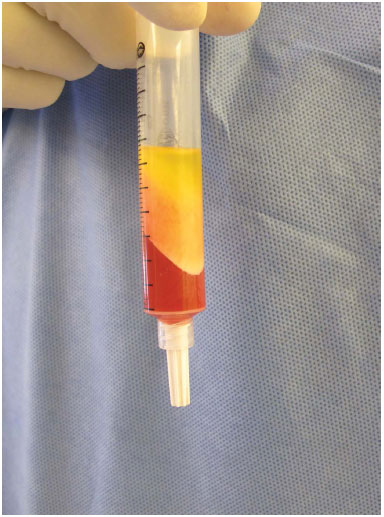
Figure 3. Centrifuging the product with a well-defined fat layer.
Grafting
The fat contained in the 10 ml syringe is transferred to a 1 ml syringe through exchangers (Figure 4). Grafting is accomplished with blunt cannulas of 0.7 to 1.4 mm (15 to 21 G) on the receiver tissue in multiple layers from pre-periosteal plane to the subdermal plane, depending on the area to be treated.
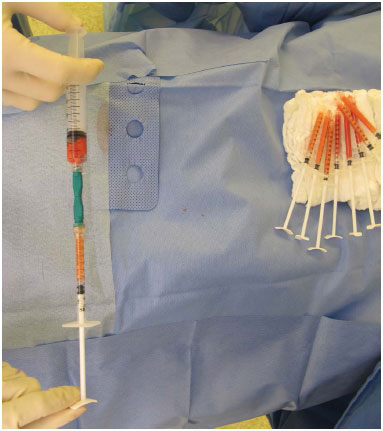
Figure 4. Fat transfer to subsequent grafting.
We incised the skin with a simple Jelco 16 perforation without further need for closure. After advancement of the cannula to the desired recipient area, the surgeon begins its gradual withdrawal, injecting fat whenever there is resistance in the receptor tissue created in the tunnel. Where there is no such resistance, fat is not injected because the assumption is that this area has already been grafted. The amount of fat injected ranges from 1/10 to 1/50 ml. That is, to inject 1 ml of fat, 10 to 50 cannula tunnels are needed in the tissue (Figure 5). The intention is that tiny particles of fat tissue in multiple intersecting tunnels ensure that each is in a compartment with as much contact as possible with the receptor tissue (Figure 6).
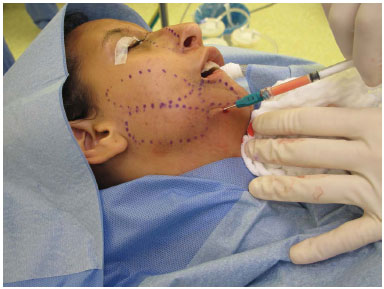
Figure 5. Fat grafting in multiple layers in a case of Romberg syndrome.

Figure 6. Particles of fat should be in contact with the recipient tissue as much as possible.
Retrobulbar grafting
The procedure in these cases has already been described. The difference is that the that the grafting cannula is advanced to the orbital apex cone through eyelid access in the inferolateral regions and superomedial orbit (Figure 7).

Figure 7. A: Retrobulbar fat grafting performed in the inferolateral region of the orbit. B: Retrobulbar fat grafting performed in the superior-medial region of the orbit.
Postoperative
We do not apply cold compresses or bandaging, and we also avoid pressure in the grafted area for two weeks (paying attention to sleeping position). Massage is not performed. We re-evaluate the need for further fat grafting sessions between 3 and 4 months postoperatively.
RESULTS
During the study period, 22 patients were treated with fat grafting strictly following the described method. Most patients were female (77%). The volume of fat applied varied from 1 ml to 37 ml, with a mean of 15 ml per session. The number of sessions ranged from 1 to 4, with the majority of patients having only one session (82%). Fat grafting was used as the sole treatment in 30% of cases and was associated with other surgical procedures in 70% of patients, including mandibular distraction, orthognathic surgery, mentoplasty, cranioplasty, orbital reconstruction, reconstruction cheekbone and canthoplasty. The most common diagnoses were trauma sequelae (10), Romberg syndrome (5), hemifacial microsomia (2), oncologic resection sequelae (2), Treacher-Collins syndrome (1), Goldenhar syndrome (1), and Meckel-Wagner syndrome (1) (Figures 8 to 12).
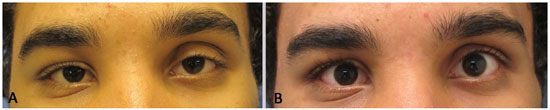
Figure 8. A: Meckel-Wagner syndrome. Pre-operative, before grafting of 1 ml of fat in the upper eyelid. B: Meckel-Wagner syndrome. Postoperative, after grafting of 1 ml of fat in the upper eyelid.

Figure 9. A: Hemifacial microsomia. Preoperative, before a 10 ml fat graft in the hemiface and bilateral mandibular distraction. B: Hemifacial microsomia. Postoperative, after fat grafting of 10 ml in the hemiface and bilateral mandibular distraction.
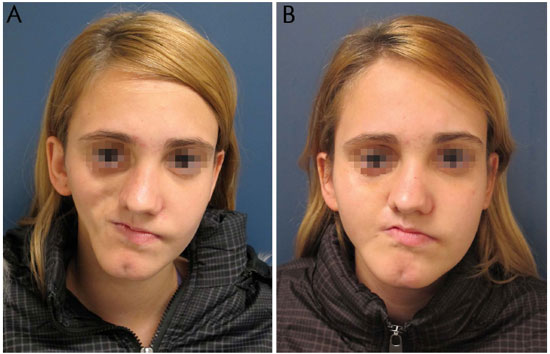
Figure 10. A: Romberg syndrome. Preoperative, before grafting of 37 ml of fat in the hemiface. B: Romberg syndrome. Postoperative, after grafting 37 ml of fat into the hemiface.

Figure 11. A: Goldenhar syndrome. Preoperative, before 10 ml of fat grafting in the hemiface and mentoplasty advancement. B: Goldenhar syndrome. Postoperative, after 10 ml of fat grafting in hemiface and mentoplasty advancement.

Figure 12. A: Sequelae following jaw tumor removal. Pre-operative, before orthognathic surgery. B: Sequelae following jaw tumor removal. Postoperative, after orthognathic surgery. C: Sequelae to the jaw tumor removal. Serial postoperative fat grafting in the hemiface (15, 18, 15 and 30 ml).
Of the patients with trauma sequelae, four had late enophthalmos, i.e., patients who had already undergone a surgery to balance and restore the volume of the orbit. All patients were amaurotic in the affected eye, and one had a scleral lens. We performed retrobulbar fat grafting ranging from 6 to 10 ml in the grafted volume, which in one patient was carried out over two sessions. In the other 3 patients, just one session was performed (Figure 13). There was a gain of 3 to 7 mm projection of the eyeball in the patients without scleral lens (Figure 14) (Table 1). In the patient with a scleral lens, it was necessary to refine the prosthesis in order to adjust it better to the new volume of the orbit. In the tomographic evaluation, through overlapping preoperative and postoperative images using the Dolphin® software, we also found increased eye projection in patients 2 and 3 (Table 1), and patient 2 (Figure 15) had a 4 mm increase (vs. exophthalmometry of 3 mm) and Patient 3 (Figure 16) had a 2.2 mm increase (vs. 3 mm of exophthalmometry), which caused further protrusion of the operated eye than the sound eye (66.3 vs. 65.4 mm, respectively).
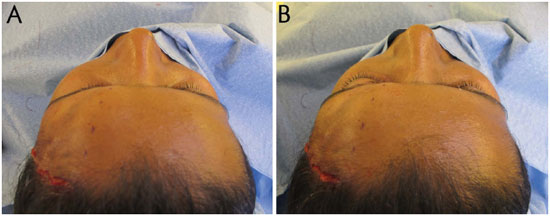
Figure 13. A: Retrobulbar fat grafting. Preoperative, immediately before fat injection. B: Retrobulbar fat grafting. Immediate postoperative period of fat injection.

Figure 14. Evaluation of projection of the eyeball with a Hertel exophthalmometer.
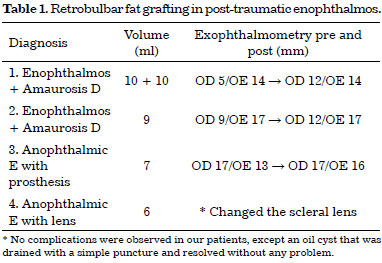
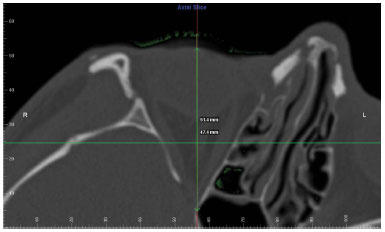
Figure 15. Patient 2. Overlapping CT slices performed by Dolphin® showing a 4mm increase in projection of the eyeball.

Figure 16. Patient 3. Overlapping CT slices by Dolphin® showing an increase of 2.2 mm in the projection of the eyeball.
Although the Hertel exophthalmometer results and CT scans found increased projection of the eyeball, upon inspection we did not observe marked improvements in aesthetics. The clinical outcome was therefore regarded as poor (Figure 17).

Figure 17. A: Patient 3. Preoperative, before retrobulbar fat grafting. B: Patient 3. Postoperative, after retrobulbar fat grafting of 7 ml, presenting a clinical outcome inferior to CT and exophthalmometric findings.
We found no complications in our patients, except an oil cyst that was drained with a single puncture and resolved with no further problems.
DISCUSSION
Despite the fact that fat grafting is a procedure enshrined in the practice of reconstructive and cosmetic plastic surgery, there is currently no scientific evidence regarding which techniques are superior in relation to the aspiration, processing or application of autologous fat11. At INTO-RJ, we perform fat grafting based on the Coleman precepts12, a technique used by many surgeons who perform fat grafting. As mentioned, there is currently no consensus on the best technique, but we think that it is important to follow a standard protocol.
In the cranio-maxillofacial surgery service at INTO-RJ, fat grafting has been performed both in isolation and associated with other surgical strategies. It is often the only treatment needed to correct volume defects and contouring of the face: for example, in patients with Romberg syndrome, we perform serial fat grafting rather than use free flaps13. Some advantages of adipose tissue use are unequivocal. Because it is autologous, its application minimizes problems such as rejection and extrusion. There are plenty of areas from which to obtain donor tissue and the easy capture of adipose tissue involves low morbidity to patients with minimal complication rates.
The surgical team noted an improved quality of skin grafted areas where fat grafting was performed. Mojallal et al.14 in 2009 demonstrated the same finding in experimental studies. An improvement in the quality of skin grafted areas would be an additional advantage of fat grafting in patients with craniofacial deformities, as these patients present with true skin hypoplasia in addition to a lack of volume.
We did not objectively assess engraftment using radiological examinations or software images, but we believe our engraftment rate was similar to that in the literature, between 40% and 80%5-10. However, we realize that the engraftment rate on the eyelids is higher or almost complete. Therefore, we do not recommend overcorrectionin the periorbital region, unlike that for the rest of the face. For the rest of the face, it is important to clarify to the patient that no matter how small the deformity, usually, more than one fat grafting session will be required to achieve a good result.
We found a high level of satisfaction among our patients, sometimes to a greater degree than that of the surgical team. It is not uncommon that these patients would question the timing of the next fat grafting session. We think that fat grafting is a procedure that can be offered to mitigate facial deformity, for the mildest to the most severe cases. The possibility of a minor improvement, or the wait for ideal conditions for major surgery, is important to the psychological wellbeing of some patients undergoing treated. At other times, fat grafting not only mitigates symptoms but is the treatment of choice, as in some cases of Romberg syndrome.
In cases of late enophthalmos, despite increased objective projection of the eyeball found using the Hertel exophthalmometer and CT, clinically, we observed no improvement in the appearance of these patients. Moses et al.15 found a pattern of normality in exophthalmometry of 10-23 mm, and a difference of only 3 mm projection between the two eyeballs would be significant and noticeable16. However, our three patients who did not have scleral lens showed significant gain in projection, although there was no great clinical significance. We believe that as these patients had already been operated several times previously and with other periorbital arrangements, the gain in the projection did not have the desired aesthetic effect. Retrobulbar fat grafting is still a rarely used procedure, with only four publications on this subject until now17-20. Bradycardia may occur during retrobulbar grafting, and the anesthetist and the surgeon should be aware of this complication.
CONCLUSION
Fat grafting is a simple, inexpensive and reproducible procedure that should be part of the plastic surgeon's and craniofacial surgeon's inventory. It provides good results, has a low complication rate, and may be performed in isolation or with another procedure. It may be an alternative in difficult cases of late enophthalmos. In addition, it improves the skin quality of the grafted area.
ACKNOWLEDGMENTS
We thank Dr. Roberto Sebastiá for his help in our first cases of retrobulbar fat grafting.
REFERENCES
1. Bucky LP, Kanchwala SK. The role of autologous fat and alternative fillers in the aging face. Plast Reconstr Surg. 2007;120(6 Suppl):89S-97S. DOI: http://dx.doi.org/10.1097/01.prs.0000248866.57638.40
2. Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001;28(1):111-9. PMID: 11248861
3. Kanchwala SK, Holloway L, Bucky LP. Reliable soft tissue augmentation: a clinical comparison of injectable soft-tissue fillers for facial-volume augmentation. Ann Plast Surg. 2005;55(1):30-5. DOI: http://dx.doi.org/10.1097/01.sap.0000168292.69753.73
4. Kaufman MR, Bradley JP, Dickinson B, Heller JB, Wasson K, O'Hara C, et al. Autologous fat transfer national consensus survey: trends in techniques for harvest, preparation, and application, and perception of short- and long-term results. Plast Reconstr Surg. 2007;119(1):323-31. DOI: http://dx.doi.org/10.1097/01.prs.0000244903.51440.8c
5. Zocchi ML, Zuliani F. Bicompartmental breast lipostructuring. Aesthetic Plast Surg. 2008;32(2):313-28. PMID: 18188638 DOI: http://dx.doi.org/10.1007/s00266-007-9089-3
6. Wolf GA, Gallego S, Patrón AS, Ramírez F, de Delgado JA, Echeverri A, et al. Magnetic resonance imaging assessment of gluteal fat grafts. Aesthetic Plast Surg. 2006;30(4):460-8. DOI: http://dx.doi.org/10.1007/s00266-005-0202-1
7. Niechajev I, Sevćuk O. Long-term results of fat transplantation: clinical and histologic studies. Plast Reconstr Surg. 1994;94(3):496-506. PMID: 8047602 DOI: http://dx.doi.org/10.1097/00006534-199409000-00012
8. Delay E, Garson S, Tousson G, Sinna R. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29(5):360-76. DOI: http://dx.doi.org/10.1016/j.asj.2009.08.010
9. Park S, Kim B, Shin Y. Correction of superior sulcus deformity with orbital fat anatomic repositioning and fat graft applied to retro-orbicularis oculi fat for Asian eyelids. Aesthetic Plast Surg. 2011;35(2):162-70. DOI: http://dx.doi.org/10.1007/s00266-010-9574-y
10. Rubin A, Hoefflin SM. Fat purification: survival of the fittest. Plast Reconstr Surg. 2002;109(4):1463-4. DOI: http://dx.doi.org/10.1097/00006534-200204010-00049
11. Gir P, Brown SA, Oni G, Kashefi N, Mojallal A, Rohrich RJ. Fat grafting: evidence-based review on autologous fat harvesting, processing, reinjection, and storage. Plast Reconstr Surg. 2012;130(1):249-58. PMID: 22743888 DOI: http://dx.doi.org/10.1097/PRS.0b013e318254b4d3
12. Coleman SR, Mazzola RF, eds. Fat injection: from filling to regeneration. St. Louis: Quality Medical Publishing; 2009.
13. Tanna N, Wan DC, Kawamoto HK, Bradley JP. Craniofacial microsomia soft-tissue reconstruction comparison: inframammary extended circumflex scapular flap versus serial fat grafting. Plast Reconstr Surg. 2011;127(2):802-11. PMID: 21285784 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181fed6e4
14. Mojallal A, Lequeux C, Shipkov C, Breton P, Foyatier JL, Braye F, et al. Improvement of skin quality after fat grafting: clinical observation and an animal study. Plast Reconstr Surg. 2009;124(3):765-74. PMID: 19730294 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181b17b8f
15. Moysés NA, Lucci LMD, Fonseca Júnior NL, Rehder JRCL. Valores da exoftalmometria média na população adulta da região do Grande ABC, São Paulo/Brasil. Rev Bras Oftalmol. 2010;69(2):104-9. DOI: http://dx.doi.org/10.1590/S0034-72802010000200007
16. Fearmonti RM, Marcus JR. Orbital fractures. In: Marcus JR, Erdmann D, Rodriguez ED. Essentials of craniomaxillofacial trauma. St. Louis: Quality Medical Publishing; 2012. p.201-20. DOI: http://dx.doi.org/10.1097/SCS.0b013e3182668b4f
17. Hunter PD, Baker SS. The treatment of enophthalmos by orbital injection of fat autograft. Arch Otolaryngol Head Neck Surg. 1994;120(8):835-9. PMID: 8049045 DOI: http://dx.doi.org/10.1001/archotol.1994.01880320037009
18. Hardy TG, Joshi N, Kelly MH. Orbital volume augmentation with autologous micro-fat grafts. Ophthal Plast Reconstr Surg. 2007;23(6):445-9. DOI: http://dx.doi.org/10.1097/IOP.0b013e31815928f8
19. Cervelli D, Gasparini G, Moro A, Grussu F, Boniello R, Pelo S. Retrobulbar lipofilling to correct the enophthalmos. J Craniofac Surg. 2011;22(5):1918-22. DOI: http://dx.doi.org/10.1097/SCS.0b013e318210bbc8
20. Cakir B, Aygit AC, Omur-Okten O, Yalcin O. Retro-orbital intraconal fat injection: an experimental study in rabbits. J Oral Maxillofac Surg. 2012;70(1):242-50. PMID: 21763046 DOI: http://dx.doi.org/10.1016/j.joms.2011.02.091
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Instituto Nacional de Traumatologia e Ortopedia, Rio de Janeiro, RJ, Brazil
Institution: Instituto Nacional de Traumatologia e Ortopedia (INTO), Rio de Janeiro, RJ, Brazil
Corresponding author:
Pablo Maricevich
Av. Antônio de Góes, 275, Pina
Recife, PE, Brazil Zip Code 51110-000
E-mail: jpmaricevich@gmail.com
Article received March 26, 2014.
Article accepted August 31, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter