

Original Article - Year 2015 - Volume 30 -
Use of the myocutaneous latissimus dorsi flap with fat extension in breast reconstruction: an option for filling the upper pole
Utilização do retalho miocutâneo de grande dorsal, com extensão adiposa, nas reconstruções mamárias: uma opção para preenchimento do polo superior
ABSTRACT
INTRODUCTION: The sequelae of mastectomy presents in numerous ways, requiring the experience and creativity of the surgeon to achieve the best result in the reconstruction of a new breast. One of the difficulties in achieving this objective is the challenge of adequately filling the upper pole of the breast. The objective of this work was to present an alternative therapeutic option for correction of the upper pole of the neobreast.
METHODS: In our surgical technique, a latissimus dorsi muscle flap with fat extension is used for filling the upper pole of the neobreast during its reconstruction. The described technique was used in 8 patients during late breast reconstruction. The patients' ages ranged from 39 and 70 years. The size of the fat extension ranged from 4.0 × 10.0 cm to 7.0 × 13.0 cm. The fat component of the flap was evaluated after 3 months by using magnetic resonance imaging (MRI).
RESULTS: Breast implants that varied in volume between 270 and 435 mL were used. The follow-up period after surgery ranged from 3 months to 1 year. Two patients had epidermolysis (28%) at the junction of the cutaneous flap and the receiver area. No graft loss or other complications occurred. Our results demonstrate clinically or visually that correction of the depression in the upper pole of the neobreast was satisfactorily achieved. The viability of the fat flap, as observed on MRI, was adequate.
CONCLUSION: The proposed technique is a suitable alternative method for filling the depression in the upper pole of the neobreast in most cases of breast reconstruction.
Keywords: Breast reconstruction; Myocutaneous flap; Mastectomy; Superficial muscles of the back.
RESUMO
INTRODUÇÃO: As sequelas de mastectomia se apresentam de formas variadas exigindo, do cirurgião, experiência e criatividade para obter o melhor resultado na reconstrução de uma nova mama. Dentre as dificuldades para que este objetivo seja alcançado, está o desafio de um melhor preenchimento do polo superior da mama. O objetivo deste trabalho é apresentar uma opção terapêutica alternativa para correção do polo superior dentre as técnicas já existentes com este propósito.
MÉTODO: A técnica cirúrgica utilizou o retalho de músculo grande dorsal com extensão gordurosa para preenchimento do polo superior da neomama durante sua reconstrução. A técnica descrita foi utilizada em 8 pacientes durante a reconstrução mamária tardia, com idades variando entre 39 e 70 anos. O tamanho desta extensão gordurosa variou entre 4,0 × 10,0 e 7,0 × 13,0 cm. O componente gorduroso do retalho foi avaliado após 3 meses através de ressonância magnética.
RESULTADOS: Foram usados implantes mamários que variavam entre 270 e 435 ml. O acompanhamento pós operatório variou entre 3 meses a 1 ano. Ocorreram 2 casos de epidermólise (28%) na junção do retalho cutâneo com a área receptora. Não houve perda ou sofrimento do retalho. Os resultados demonstram clinicamente ou visualmente que a correção da depressão do polo superior da neomama foi alcançada adequadamente, bem como a viabilidade do retalho gorduroso, observada nos exames de imagem (ressonância magnética).
CONCLUSÃO: A técnica proposta é uma alternativa adequada para o tratamento da maioria dos casos de reconstrução mamária em que se busca o preenchimento da depressão existente no polo superior da mama.
Palavras-chave: Reconstrução da mama; Retalho miocutâneo; Mastectomia; Músculos superficiais do dorso.
The sequelae of mastectomy present in numerous ways, requiring experience and creativity from the surgeon in order to obtain the best results in the reconstruction of a new breast. One should consider the therapeutic option and the diversity of the anatomy, in addition to the desire and expectation of the patient.
Among these details, depression in the upper pole of the neobreast has been the target of many treatment options such as fat grafting1,2, alloplastic material implants such as aloderme3,4, and silicone implants5. During breast reconstruction using the latissimus dorsi muscle and implants, this region is filled with the inclusion of the adipose tissue segment located below the skin island. We call this a myocutaneous flap with fat extension because it encompasses the 3 segments with different functions, namely the muscle segment for the coverage of the implant, the fat to fill the upper pole of the breast, and the skin to restore the lack of skin in the mammary region.
Hokin and Silfverskiold6, in 1983, proposed a technique for breast reconstruction using a latissimus dorsi flap but without the use of prosthesis. For such, they included the adipose tissue overlaying the latissimus dorsi muscle above and below the skin segment, calling it the extended latissimus dorsi flap.
In our technique, we use only the adipose tissue compartment in the lower portion of the skin segment, called the lumbar fold, which was described by Bailey et al.7 in 2010, to fill the depression in the upper pole of the neobreast, which is often not filled by the prosthesis or volume of the latissimus dorsi muscle.
OBJECTIVE
To demonstrate that the use of the fat compartment of the lumbar area, located below the skin island of the latissimus dorsi muscle, is useful for filling the depression of the upper pole of the neobreast in breast reconstruction after mastectomy.
METHODS
We used the myocutaneous flap with fat extension of the latissimus dorsi muscle in 8 patients during late breast reconstruction. The patients attended the private clinic of the main author and underwent evaluation between 2012 and 2013.
Their ages ranged from 39 to 70 years. Among the patients, 3 underwent reconstruction of the right breast and 5 underwent reconstruction of the left breast. Six patients had undergone radiotherapy.
We demarcated the area to be excised, or incised, in the mammary region for placement of the skin segment, besides measuring the depression area on the upper pole of the neobreast (Figure 1).
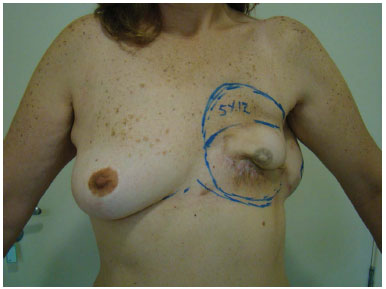
Figure 1. Marking of the area to be incised for flap placement, the area to be detached for implant placement, and the upper area for the placement of the flap fat extension.
The skin island of the latissimus dorsi muscle flap was demarcated. Below this, the fat extension in the lumbar fold region was used for the filling of the upper pole of the neobreast (Figure 2). The size of the fat extension ranged from 4.0 × 10.0 cm to 7.0 × 13.0 cm.
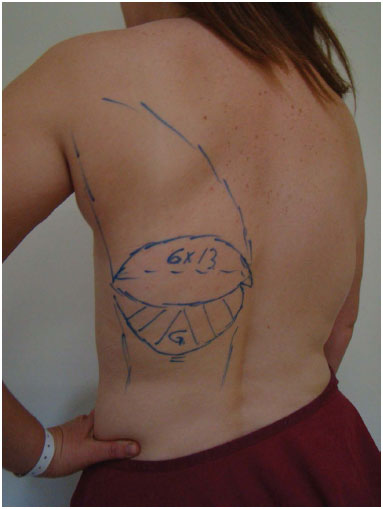
Figure 2. Demarcation of the myocutaneous latissimus dorsi muscle flap, below which (G) is the fat extension in the projection of the lumbar compartment, with dimensions corresponding to the segment to be attained in the upper neobreast pole.
After infiltration of saline solution and adrenaline (concentration, 1.1000.000 IU) in the incision lines, we incised up to the fascia of Scarpa when we began to detach inferiorly the skin island in order to construct a peninsula of adipose tissue (Figure 3).
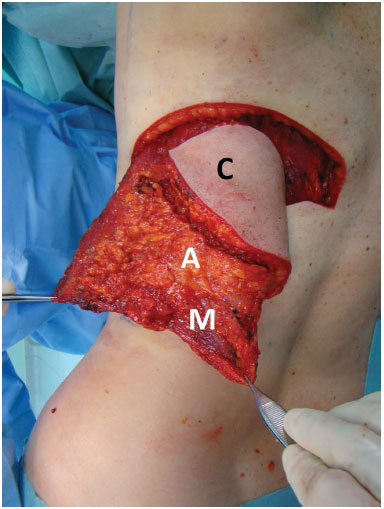
Figure 3. A flap with the 3 segments, namely the cutaneous (C), fat (A), and muscle (M) segments.
The isolation of the latissimus dorsi muscle was initiated by using its lower edge. The release of the flap was made in the cranial direction to allow migration to the mammary region without tension.
Upon closing the donor area, accession sutures were applied to the deep layers, as recommended by Baroudi and Ferreira8, together with closed drainage with aspiration. The wound was closed layer by layer, with care to compensate for the difference in height between the top and bottom flaps.
In the construction of the neobreast, we positioned the bottom of the dorsal flap in the upper pole of the mammary region, with fixation of the muscle in pectoral fascia and positioning of the adipose area under the area of the upper pole of the neobreast (Figure 4).

Figure 4. A flap positioned in the mammary region, demonstrating the adipose segment used to fill the upper neobreast pole.
From the third month, we evaluated the adipose segment by using magnetic resonance imaging (MRI).
This study was approved by our institutional ethics committee (CEP 172/2011) and conducted according to the principles of the Declaration of Helsinki.
RESULTS
The postoperative follow-up period ranged from 3 to 12 months (Figure 5A).
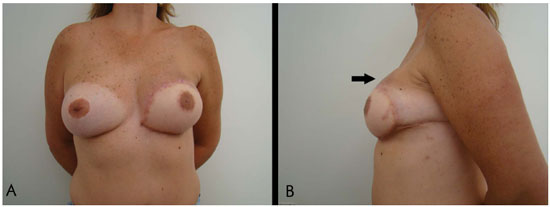
Figure 5. A: The 1-year and 4-month postoperative aspects of breast reconstruction using myocutaneous flap with fat extension and breast implant. B: The 1-year and 4-month postoperative aspects showing the projection of the upper neobreast pole due to the adipose segment of the flap positioned in the upper pole (arrow).
No graft loss or other complications occurred. The projection of the upper pole of the breast was maintained (Figure 5B).
The implant volume ranged from 270 and 435 cc.
The adipose segment was maintained, as observed on MRI, in all of the cases analyzed after 3 months (Figure 6).

Figure 6. A magnetic resonance image obtained in the postoperative period, demonstrating the preserved fat extension (circle).
Two patients (28%) had epidermolysis at the junction of the cutaneous flap and the receiver area. One of the patients had a prior mammoplasty scar, and the other patient had undergone local radiotherapy. Both progressed well with topical treatment. We observed in the dorsum the difference in thickness between the upper and lower flap, which resulted from the withdrawal of fat from the lower portion. In the first case, due to excess thinning of the skin flap, distress of the lower edge of the scar in the dorsal region, which was resolved with topical therapy. The outcome showed no graft impairment. Seroma occurred in the donor area in 2 patients (28%) but was resolved with fine-needle aspiration only.
DISCUSSION
Mastectomy causes loss of adipose tissue, which results in depression and adherence of the skin to the pectoral muscle, mainly in the upper pole. Reconstruction with a myocutaneous latissimus dorsi flap and implant provides projection of the breast but not enough projection in the upper pole to avoid depression in this area. The importance of implementing this surgical procedure is due to the following considerations:
- The use of a fat graft is not possible at the moment and usually requires more than one surgery.
- The use of a dermal matrix is costly, besides not being available globally.
- An additional silicone implant has immediate effects but is palpable and perceptible.
The inclusion of an adipose tissue segment in the body of the latissimus dorsi myocutaneous flap fills the depression, or at least reduces the need of volume in fat grafts later. Patients should have sufficient volumes of these fat deposits or compartments of lumbar fat in order to fill the upper pole of the neobreast. Some publications reported an experience with the use of the extended latissimus dorsi flap, that is, using only the fat of the dorsum (without including a silicone prosthesis) to provide volume to the neobreast. However, none of these mentioned the inclusion of part of this fat in a prosthesis or its use to fill an upper pole depression. Some of these studies reported different types of complications6,9.
Bailey et al. described an anatomical study of fat compartments in the dorsal region, dividing them into parascapular, thoracolumbar, and lumbar segments, in patients with body mass indices (BMIs) ranging from 30.6 to 51.2 kg/m2. They used flaps that included the thoracic and lumbar areas, with lengths ranging from 24 × 12 cm to 28 × 17 cm, for breast reconstruction without implants. Partial wound dehiscence associated with small infections in the donor area occurred without affecting the final result.
Our proposal is to use a myocutaneous flap with fat extension for filling the depression in the upper breast pole and a silicone prosthesis to provide volume. We observed one disadvantage, which is the difference in thickness between the upper and lower dorsal flaps in the donor area, which resulted in an unevenness in the scar region. This difference and the possibility of resolution with liposuction of the upper flap were explained to the patients.
Partial necrosis of the bottom edge of the scar in the dorsal region occurred only in the first case. This could be due to the initial inexperience in the procedure and the excess thinning of the lower flap, which was later modified by making an incision up to the fascia of Scarpa.
We believe that patients need not be obese or have a high BMI for the proposed technique to be feasible but need only to present a lumbar compartment, as the breast volume is provided by the implant.
CONCLUSION
The use of the fat compartment of the lumbar area, located below the skin island of the latissimus dorsi, is an effective and immediate approach for filling the depression of the upper pole of the neobreast in breast reconstruction after mastectomy.
REFERENCES
1. Spear SL, Wilson HB, Lockwood MD. Fat injection to correct contour deformities in the reconstructed breast. Plast Reconstr Surg. 2005;116(5):1300-5. PMID: 16217471 DOI: http://dx.doi.org/10.1097/01.prs.0000181509.67319.cf
2. Rigotti G, Marchi A, Stringhini P, Baroni G, Galiè M, Molino AM, et al. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthetic Plast Surg. 2010;34(4):475-80. PMID: 20333521 DOI: http://dx.doi.org/10.1007/s00266-010-9481-2
3. Newman MI, Samson MC, Berho M. AlloDerm in breast reconstruction: 2 years later. Plast Reconstr Surg. 2009;123(6):205e-6e. PMID: 19483545
4. Uflacker AB, Janis JE. The use of acellular dermal matrix in the correction of visible parasternal deformities after breast reconstruction. Plast Reconstr Surg. 2010;126(1):34e-36e.
5. Tavares Filho JM, Bererique M, Franco D, Arbex G, Arnaut Junior M, Franco T. Implantes complementares na reconstrução mamária. Rev Bras Cir Plást. 2012;27(2):290-3. DOI: http://dx.doi.org/10.1590/S1983-51752012000200020
6. Hokin JA, Silfverskiold KL. Breast reconstruction without an implant: results and complications using an extended latissimus dorsi flap. Plast Reconstr Surg. 1987;79(1):58-66. PMID: 3797518 DOI: http://dx.doi.org/10.1097/00006534-198701000-00010
7. Bailey SH, Saint-Cyr M, Oni G, Wong C, Maia M, Nguyen V, et al. The low transverse extended latissimus dorsi flap based on fat compartments of the back for breast reconstruction: anatomical study and clinical results. Plast Reconstr Surg. 2011;128(5):382e-94e.
8. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41. PMID: 19328174 DOI: http://dx.doi.org/10.1016/S1090-820X(98)70073-1
9. Germann G, Steinau HU. Breast reconstruction with the extended latissimus dorsi flap. Plast Reconstr Surg. 1996;97(3):519-26. DOI: http://dx.doi.org/10.1097/00006534-199603000-00004
Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Institution: HUCFF - Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
João Medeiros Tavares-Filho
Rua Buenos Aires, 255
Petrópolis, Rio de Janeiro, Brazil Zip Code 25610-141
E-mail: clinicajoaomedeiros@gmail.com
Article received April 22, 2015.
Article accepted June 07, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter