

Articles - Year 2004 - Volume 19 -
Multifunctional Abdominoplasty
Abdominoplastia Multifuncional
ABSTRACT
The present study approaches the description of a procedure that combines mixed incisions(1-4) and associated, oblique, side and upper tractions that are meant to treat patients with large abdominal aprons that underwent massive weight loss after clinical methods or by means of vertical bariatric surgery(5). The technique has been employed since September 2002 and was used in 15 patients. Weight losses ranged from 50 to 145 kg. In vertical bariatric surgery, the correction by plastic surgery was conducted within a year and a half to two postoperative years. In cases of weight loss by clinical means, this time went down to a year, on average. In regard to patients' gendet; the procedure was carried out in 7 men and 8 women. In regard to the causes of weight loss, 13 cases were after vertical bariatric surgery and 2 after clinical methods. In this procedure we approached the abdominal apron, peiformed anterior and posterior trunk modeling, and elevated the pubis and, in some cases, the thighs as well.
Keywords: Abdominoplasty for abdominal apron; abdominal dermolipectomy for the correction of abdominal apron; abdominoplasty after massive weight loss
RESUMO
O presente artigo aborda a descrição de um procedimento que combina incisões mistas(1-4) e trações associadas, oblíquas, laterais e superiores, que se destinam a tratar pacientes que sofreram grandes perdas ponderais com grandes aventais, pós-métodos clínicos ou por cirurgia bariátrica vertical(5).
A técnica vem sendo empregada desde setembro de 2002 e foi efetuada em 15 pacientes e as perdas ponderais variaram entre 50 e 145 kg.
Nos casos de cirurgia bariátrica vertical, a correção pela cirurgia plástica foi efetuada em um ano e meio a dois anos do pós-operatório. Já nos casos de perda ponderal por meios clínicos, esse tempo foi, em média, de um ano.
Quanto ao sexo dos pacientes, o procedimento foi feito em 7 homens e 8 mulheres. E, quanto às causas de perdas ponderais, 13 casos foram após cirurgia bariátrica vertical e 2 pós-métodos clínicos.
Neste procedimento tratamos do avental, realizamos as modelagens anterior e posterior do tronco, além da elevação do púbis e, em alguns casos, das coxas.
Palavras-chave: Abdominoplastia em avental; dermolipectomia abdominal para correção de avental; abdominoplastia pós-grandes perdas ponderais
Morbid obesity is a disease of known etiology that has recently had a freguent, almost epidemic occurrence.
With the advent of gastroplastic techniques(5), morbid obesity has finally begun to be handled in a safe effective manner, with results that can reach 90% of reduction in excess weight, where patients lose from 60 to 150 kg (our study). This has led to a new problem: patients start to presem major deformities due to excess skin as a result of weight loss, and large aprons with abundance of circumferential skin. This leads to serious conflict, because patients fail to accept the new body image.
Conventional abdominoplasty techniques that use circumferential incisions presem results that fali short in regard to the patient's final appearance, in addition to causing severe adverse events such as: seromas, hematomas, dehiscence, necroses, need for blood transfusions, lengthy drainage procedures, etc.
By observing such cases, we developed a technique using traction vectors with multiplying effects that could model not only the abdomen but also the flanks, dorsum, pubis and even, very often, the upper portion of the thighs, in such a way that there would be no detachment of tissue, thereby successively reducing blood loss, seromas, dehiscence, etc.
SURGICAL PLAN
MARKING THE INCISIONS TO REMOVE THE LARGE ABDOMINAL APRON
With the patient standing, we draw a line whose starting point is the xiphoid process (point "A"). From this line, two other convex lines are drawn towards the mid clavicular lines. These will descend to a point that is determined by bi-manual maneuvers, similar to those employed in the marking of mammoplasty used in the Pitanguy technique(6).
These will be our points "B" and "C".
a) Marking a pubic line, point "D", that follows bilaterally to the antero-superior iliac spines.
After this procedure, once are points are marked, a supplementary convex line is made, uniting it to the ends of the corresponding antero-superior iliac spines (Figs. l a-d).
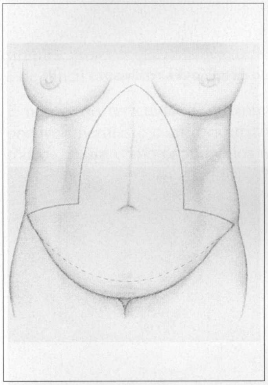
Fig. 1a - Drawing of the technique with block resection. Front view.
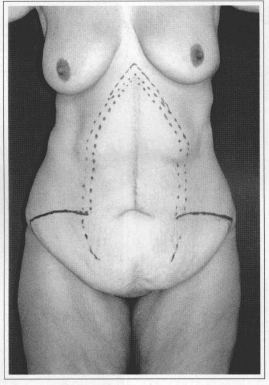
Fig. 1b - Marking the technique on the patient. Front view.
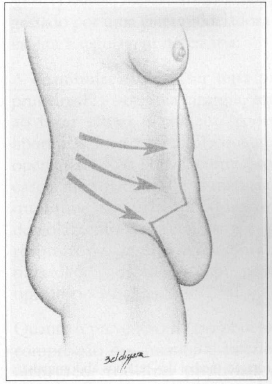
Fig. 1c - Drawing of side view showing tractions.
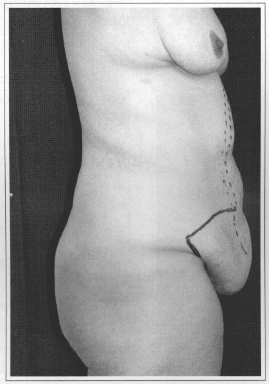
Fig. 1d - Patient in side view.
SURGICAL DESCRIPTION
Surgical resection should start with the upper marked lines. This is a simpler procedure, since it is difficult to handle up to 14 kg of abdominal apron (Figs. 2a-i).
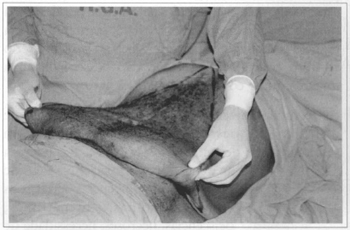
Fig. 2a - Bi-digital maneuver delimiting flap resection.

Fig. 2b - Flap traction.
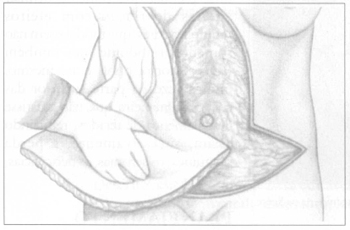
Fig. 2c - Drawing of monoblock removal.
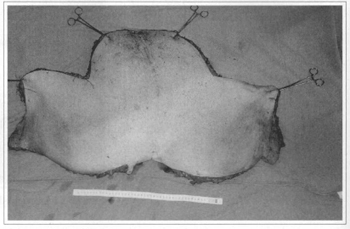
Fig. 2d - Surgical specimen resected in monoblock, weighing 14.25 kg.

Fig. 2e - Bloody area resulting from resection, before medial plicature.
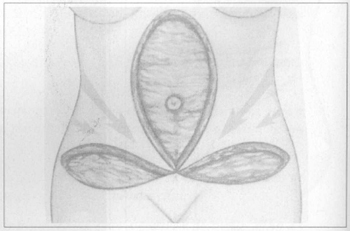
Fig. 2f - Drawing of medial rotation of abdominal flaps.
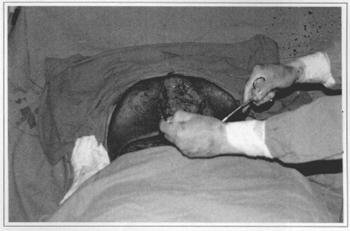
Fig. 2g - Medial rotation of abdominal flaps without detachments.
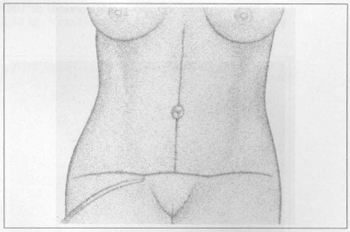
Fig. 2h - Drawing showing conclusion of inverted T-shaped suture with drainage by suction.
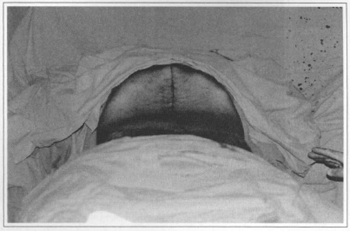
Fig. 2i - Surgery completed after suture in three planes.
During dissection, it is necessary to be alert to possible hernias and the umbilical scar(7), which is handled, as well as the anterior rectus muscles, in the conventional way.
Once this is completed, we unite points "B", "C" and "D" with a suture made by planes, without detachment, then place a thick vacuum drain, which will be removed when the drainage is below 50 ml/ day. This usually occurs in the first 48 postoperative hours.
We then use a crepe paper cast dressing, which praved very useful both for its good modeling capacity and low cost. This dressing is removed in the first exchange, which takes place in the 24 subsequem hours. At this stage, we replace the crepe paper cast dressing by a modeling strap with Velcro, which facilitates the necessary adjustments.
Patients should walk early, in the first 24 hours after surgery. Patients should sir up carefully to avoid lipothymia, a frequent intercurrence in any postoperative. Nonetheless, there was no need for blood transfusion and there were no respiratory disorders in any of the cases, probably due to the non-detachment of flaps and expanded respiratory capacity developed during the morbid obesity period.
To prevent thromboembolism, during surgery we compress lower limbs, popliteal fossa and massage the calves in the immediate postoperative. Early walking follows these procedures.
DISCUSSION
In addition to the difficulties of execution observed in abdominoplasties thraugh circumferential incisions in patients with large weight losses, the result eventually leads to major dissatisfaction among patients due to their resulting physical shape, in addition to a difficult postoperative period due to hematomas, seromas and dehiscence.
We thereby believe our technique will simplify the execution of the procedure and produce quite satisfactory results, both fram the clinical-surgical point of view and for all psychological and aesthetical aspects involved (Figs. 3 a-d, 4 a-d, 5 a-d, 6 a-d, 7 a-d, 8 a-d).
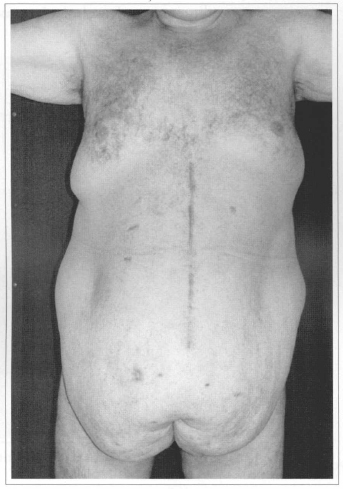
Fig. 3a - Preoperative after weight loss of 100 kg. Front view.
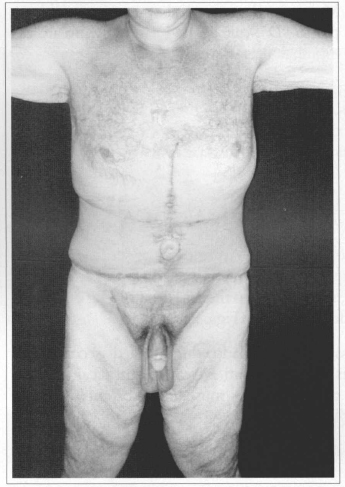
Fig. 3b - Postoperative (21 days) after resection of 14.25 kg. Front view.
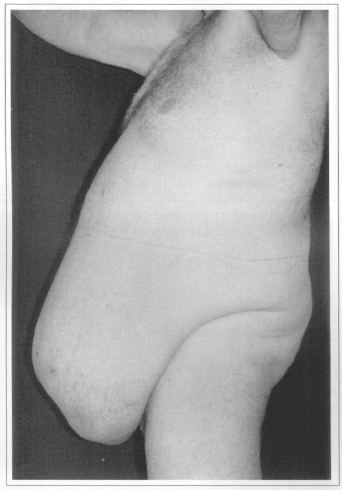
Fig. 3c - Preoperative. Side view.
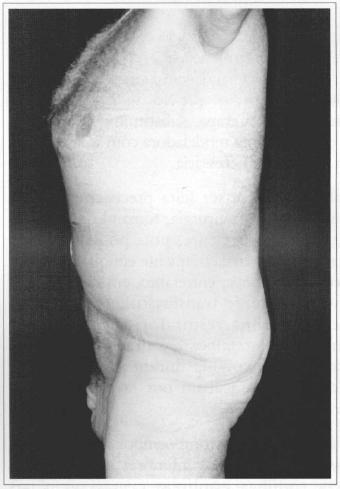
Fig. 3d - Postoperative (21 days) after resection of 14.25 kg. Side view.
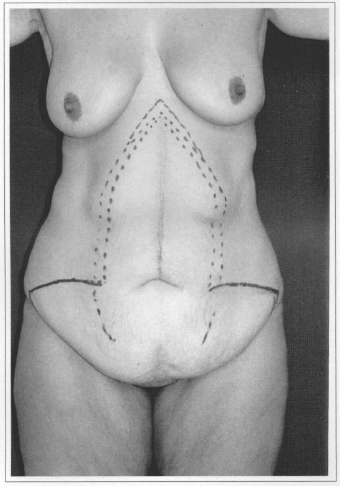
Fig. 4a - Preoperative after loss of 78 kg. Front view.
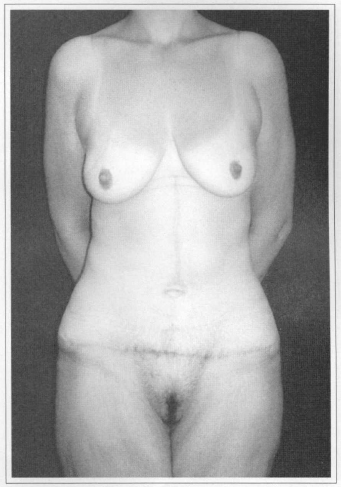
Fig. 4b - Postoperative (60 days) after resection of 3.20 kg. Front view.
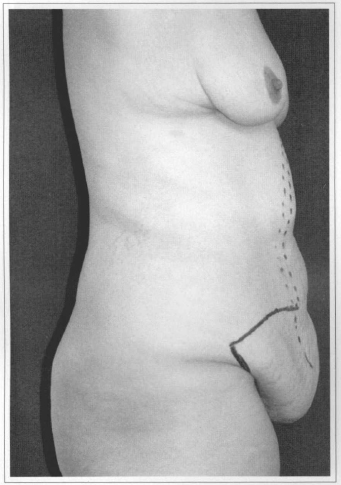
Fig. 4c - Preoperative. Side view.
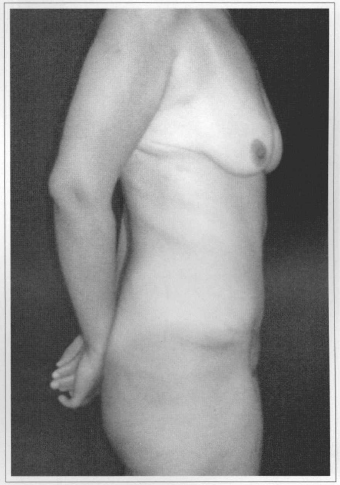
Fig. 4d - Postoperative (60 days) afrer resection of 3.20 kg. Side view.
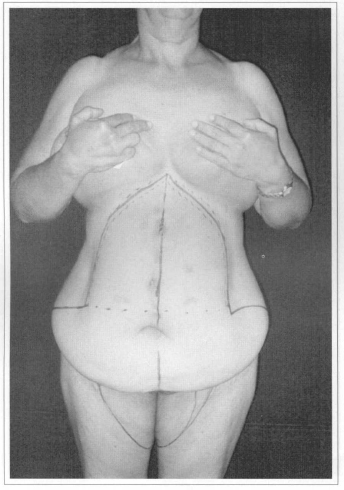
Fig. 5a - Preoperative after weight loss of 60 kg. Front view.
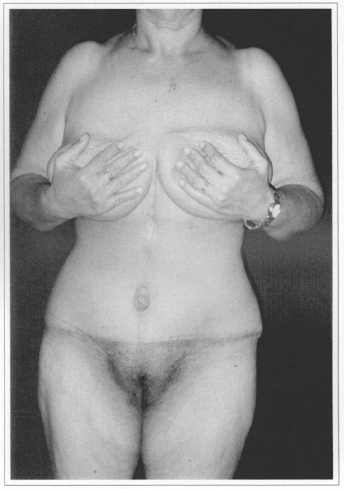
Fig. 5b - Postoperative (60 days) after resection of 3.1 kg. Front view.
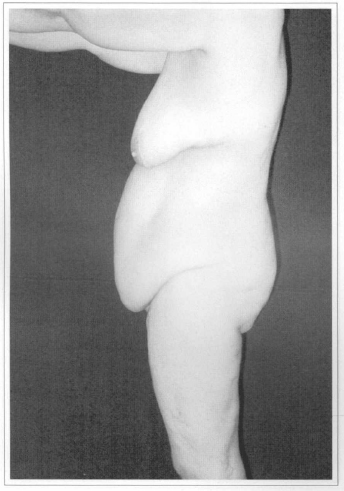
Fig. 5c - Preoperative after weight loss of 60 kg. Side view.

Fig. 5d - Postoperative (60 days) after resection of 3.1kg. Side view.
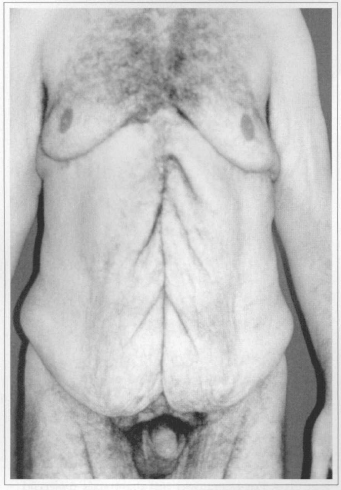
Fig. 6a - Preoperative after weight loss of 145 kg. Front view.
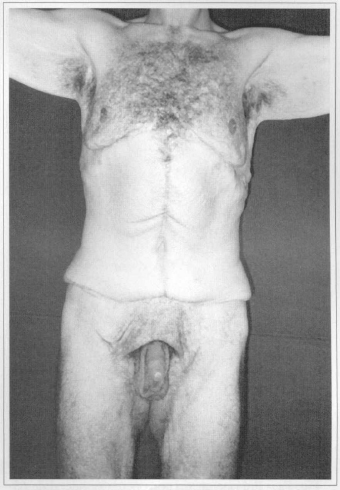
Fig. 6b - Postoperative (60 days) after resection of 3.50 kg. Front view.
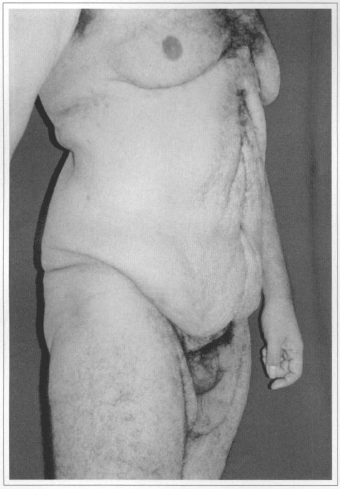
Fig. 6c - Preoperative. Side view.
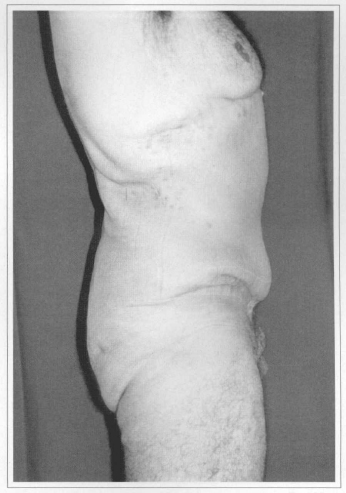
Fig. 6d - Postoperative (60 days) after resection of 3.50 kg. Side view.
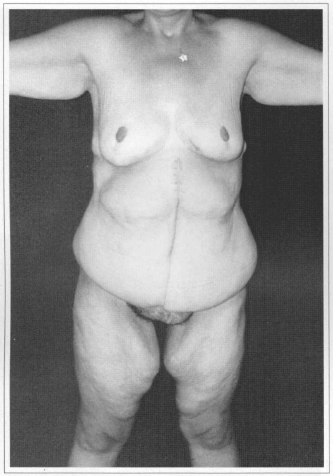
Fig. 7a - Preoperative after weight loss of 65 kg. Front view.
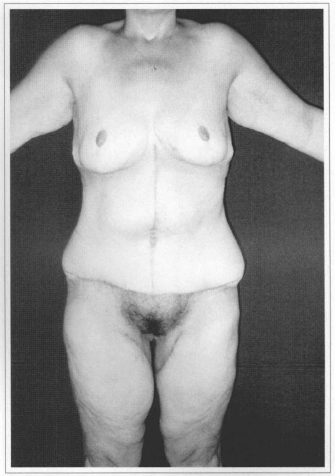
Fig. 7b - Postoperative (60 days) after resection of 4.10 kg of abdomen and thigh lifting with 2.40 kg resection (single time). Front view.
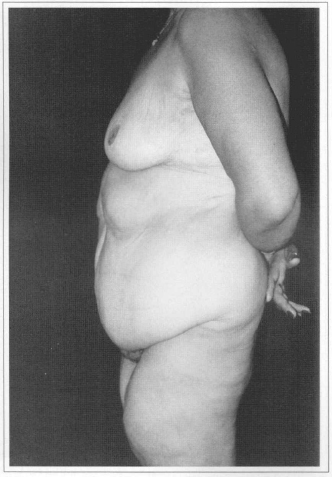
Fig. 7c - Preoperative. Side view.

Fig. 7d - Postoperative (60 days) after resection of 4.10 kg of abdomen and thigh lifting with 2.40 kg resection (single time). Side view.
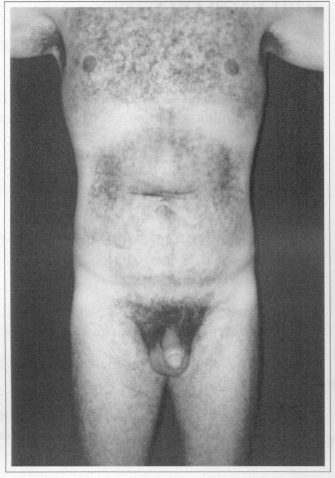
Fig. 8a - Preoperative after weight loss of 80 kg. Front view.
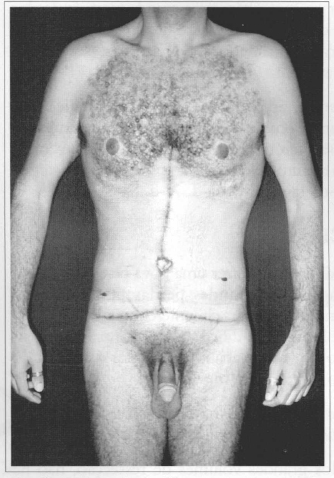
Fig. 8b - Postoperative (01 week) after resection of 2.70 kg. Front view.
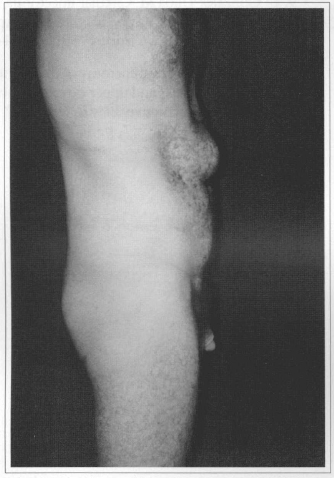
Fig. 8c - Preoperative, observe volumous incisional epigastrie hernia. Side view.
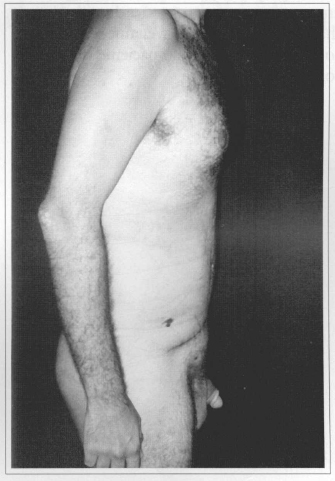
Fig. 8d - Postoperative (01 week) after reseetion of 2.70 kg and correetion of incisional epigastrie hernia.Side view.
CONCLUSIONS
This study seeks to provide a new alternative to the approach of large weight losses that produce circumferential deformity(8-10), given that this is a problem that is difticult to handle by more conventional techniques, which eventually maintain the patient's barrel- shaped trunk appearance.
Another advantage is the absence of detachment, which considerably reduces morbidity.
Despite large resection volumes, there is no substantial sequestration and, consequently, there is no need for blood transfusions.
In addition to what was written above, necroses were not observed, because vectors are distributed in a harmonie display, taking advantage of opposite forces, which gives patients back the elongated shape they desired.
REFERENCES
1. Weihold S. Bauchdeck en plastik. Zentralb F Gynak 1909; 38:1332-4.
2. Castañhares S. Goethel, J. Abdominal Lipectomy: A modification in technique. Plast Reconstr Surg 1967; 40:378-83.
3. Malbec E. Lipectomina Abdominal - Técnica Operatoria. La Prensa Médica Argentina. Vol XXXV: 243-6.
4. Kuster H. Operation bei Häungebrust und Hageleib, Monatsschr F Gebutshilfe Gynak 1926; 73:316-9.
5. Garrido JR, Arthur B. Video Atlas of Obesity Surgery. 1 ed. Guanabara Koogan; 2002.
6. Pitanguy L Mamoplastia. 1 ed. Guanabara Koogan; 1978. p. 72-6.
7. Avelas JM. Cicatriz Umbilical- da sua importância e da técnica de confecção nas abdominoplastias. Rev Bras Cir 1979; 69:41-3.
8. Somalo M. Dermolipetomia abdominal. In: Anales del primero Congreso Latinoamericano de Cirugía Plástica; 1941. São Paulo; 2:2104-6.
9. Gonzales- Ulloa M. Circular lipectomia with transposition of the umbelicus and the aponeurotic technic. Cirurj y Cirurj. 1959; 27:394-409.
10. Pitanguy I. Dermolipetomy of the abdominal wall, thighs buttocks and upper extremity, In: Converse JM. Reconstructive Plastic Surgery.2 ed. W B.Saunders; 1977. v. 7, p. 3800-23.
I - Member of the Brazilian Society of Plastic Surgery and Plastic Surgeon of the Hospital Andaraí
II - Head of the Plastic Surgery Service of the Hospital Andaraí in Rio de Janeiro - Member of the Brazilian Society of Plastic Surgery.
III - Member of the Brazilian Society of Plastic Surgery.
Study performed at the Plastic Surgery Service of the Hospital Andaraí in Rio de Janeiro, RJ - Brasil
Address for correspondence:
Carlos Del Pifio Roxo, MD
Av.Ayrton Senna, 1850 gpo. 352
22775-000 - Rio de Janeiro - RJ Brazil
Phone.: (55 21) 2430-3421
E-mail: drcroxo@rjnet.with.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter