

Case Report - Year 2015 - Volume 30 -
Reconstruction of the nasal dorsum: a case report
Reconstrução de dorso nasal: relato de caso
ABSTRACT
INTRODUCTION: The nasal dorsum is a common location for the development of cutaneous tumors, predominantly basal cell epithelioma. In 1964, Barsky recommended a quadrangular flap for coverage of the nasal dorsum, taken from the glabellar region, to most closely match the skin of the dorsal region. This was based on a simple procedure for covering raw areas up to the nasal tip, resulting in less noticeable scars.
CASE REPORT: An 82-year-old woman presented to the Plastic Surgery Service of the University Hospital Maria Aparecida Pedrossian with a lesion on the nasal dorsum of approximately 3 x 2 cm, ulcerated with an erythematous base, and ill-defined limits. A fronto-glabellar sliding flap was used to correct the loss of substance. The patient progressed with flap viability, restoration of the nasal dorsum, and satisfactory esthetic results.
CONCLUSION: Owing to the color and texture of the skin from this region, the fronto-glabellar flap is an excellent donor area for coverage of the nasal dorsum.
Keywords: Surgical flaps; Basal cell epithelioma; Nose anatomy & histology; Acquired nasal deformities; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O dorso nasal é um local comum para o desenvolvimento de neoplasias cutâneas, predominantemente o epitelioma basocelular. Em 1964, Barsky preconiza um retalho quadrangular do dorso nasal, com base na região glabelar, utilizando somente pele da região dorsal. Baseava-se em um procedimento simples recobrindo áreas cruentas até a ponta nasal, resultando em cicatrizes pouco perceptíveis.
RELATO DE CASO: Paciente de 82 anos procurou o Serviço de Cirurgia Plástica do Hospital Universitário Maria Aparecida Pedrossian apresentando lesão em dorso nasal de aproximadamente 3 × 2 cm, ulcerada com base eritematosa e limites mal definidos. A técnica utilizada para correção da perda de substância foi o deslizamento de um retalho frontoglabelar com pedículo randomizado. A paciente evoluiu com viabilidade do retalho, apresentando restauração do dorso nasal e resultado estético satisfatório.
CONCLUSÃO: Em decorrência da cor e textura adequadas da pele desta região, o retalho frontoglabelar é reconhecidamente uma excelente área doadora para cobertura do dorso do nariz.
Palavras-chave: Retalhos cirúrgicos; Epitelioma basocelular; Nariz/anatomia & histologia; Deformidades adquiridas nasais; Procedimentos cirúrgicos reconstrutivos.
The nasal dorsum is a common location for the development of cutaneous neoplasms, predominantly basal cell carcinoma.
The indications for partial nasal reconstruction result from multiple causes, including the resection of benign or malignant nasal tumors, infections, and trauma. Nevertheless, the most common indication is the resection of nasal tumors, especially basal cell carcinoma.
Nasal reconstruction was one of the first plastic procedures practiced in the history of medicine, first mentioned in the Edwin Smith Papyrus in ancient Egypt, circa 3000 B.C.1,2. The first reports of nasal reconstruction techniques date from approximately 600 B.C., in ancient India. For centuries, various nasal reconstruction techniques have been proposed and improved upon. Moderate to extensive skin defects of the nasal dorsal are a challenge for reconstruction, as irregularities in color, texture, and skin thickness are easily noticed in this location.
The front flap was first used in the western world by Joseph Carpue in England, who published two case reports in 1816. In the 20th century, Gillies, Converse, and Millard were pioneers in this modality of surgical treatment3,4. In 1964, Barsky recommended a quadrangular flap of the nasal dorsum, based on the glabellar region, using only skin from the dorsal region. This method was based on a simple procedure, overlaying the raw surface up to the nasal tip, resulting in barely perceptible scars. The withdrawal of two compensation triangles near the eyebrows enlarges the range of action of this flap2.
Currently, the aesthetic properties of the nasal subunits and the understanding of the various techniques available for the reconstruction of each one are of vital importance to achieve a satisfactory nasal reconstruction2-5. In general, the coverage modality is chosen based on surgical experience and the patient's clinical condition, especially in view of the possibility of recurrence of the lesion. In the dorsal region, the skin is thicker and mobile and is more firmly adhered to underlying cartilage, so skin grafts tend to produce aesthetic distortions, especially in the absence of sustaining cartilage. Neighboring flaps allow restoration of shape and feature a more similar color, without the need for harvesting donor skin grafts from more distant sites. There is a consensus that the best tissue for reconstruction of the nose is the closest to the defect, as this more closely matches the characteristics of lost skin. The flap described in this case report demonstrates quite favorable functional and aesthetic results for lesions in these locations.
The present report aims to demonstrate how the sliding fronto-glabellar flap is a valid solution, because with one operation we can achieve restoration and full coverage of the nasal dorsum and a repair close to the desired aesthetic.
CASE REPORT
An 82-year-old woman presented with a 10-year excision history for a nasal tumor. She remained without medical follow up for five years, after which she presented with a new lesion in the resected area. The patient sought treatment at the Plastic Surgery Service of the University Hospital Maria Aparecida Pedrossian with an ulcerated injury in the nasal dorsum, approximately 3 x 2 cm, with an erythematous base and poorly defined limits (Figure 1).

Figure 1. Pre-operative frontal view of the patient with basal cell carcinoma in the nasal dorsum and demarcations of the incision, limit of the detachment and compensatory triangles on eyebrows.
The patient was operated on under general anesthesia, with antiseptic and aseptic techniques. The technique used was a sliding fronto-glabellar myocutaneous flap with subperiosteal detachment of the frontal region, up to the limit of detachment at the superficial temporal septum laterally and the parietal region superiorly.
During the surgical planning, first the donor area of the flap was demarcated (Figure 2) over the fronto-glabellar region. We then proceeded with an incision in the demarcated area and the withdrawal of two compensatory triangles on the brow. The flap was dissected to full thickness, including the epidermis, dermis, hypodermis, and muscle. After detachment, the donor area was approximated using polyamide 5.0 suture (Mononylon® 5.0 - Johnson & Johnson Laboratories - Ethicon/Brazil).
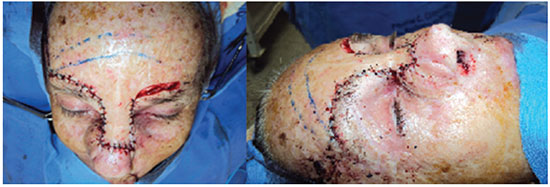
Figure 2. Aspect of the flap in the intraoperative period. A slight elevation of the nasal tip and the way the flap is accommodated on the dorsum resembling the skin lost by tumor resection can be observed.
The patient progressed with a viable flap, with restoration of the nasal dorsum and a satisfactory aesthetic result (Figure 3).

Figure 3. The patient on the 14th postoperative day, with the flap of the dorsal region presenting its own contour of the region and a barely noticeable scar.
DISCUSSION
The versatility and usefulness of the sliding fronto-glabellar flap are well recognized in nasal reconstruction. The advantages of the use of the flap include the simplicity of its implementation, low morbidity, reduced surgical time, and practically no scars in the donor area.
In nasal reconstructions requiring wide resection, the use of adjacent flaps has the advantages of better matching the coloring of the skin, better filling of the removed area in terms of depth, and better possibility for reconstruction of the mutilated area.
The forward flap has the advantages of maintaining the contour of the region and of a good scar location, with the disadvantage of requiring a large detachment, which may be in the subcutaneous (more bleeding and increased risk of nerve injury), or subgaleal tissue planes (good vascularization and lower distensibility).
The vertical advance of a rectangular sliding flap of the skin of the dorsum can resolve minor defects in the middle third and possibly even in the nasal tip, especially in elderly patients in whom there is a drop of the nasal tip. To facilitate this process and better accommodate the overhang formed proximally, two compensatory triangles can be removed from its base6.
The nasal appendage, with its anatomical, morphological, and functional complexity, is one of the more difficult organs to repair. We advocate the use of adjacent flaps as the best treatment to achieve the desired form and maintain the importance that the nose offers to the functional aesthetic harmony.
CONCLUSION
The choice of nasal reconstruction technique aims essentially to heal the injury, restore the nasal function, maintain a good respiratory airway, and finally, achieve an aesthetic nasal unit close to the natural form. Owing to the adequate color and texture of the skin in this region, the fronto-glabellar flap is recognized as an excellent donor area for coverage of the nasal dorsum.
REFERENCES
1. Whitaker IS, Karoo RO, Spyrou G, Fenton OM. The birth of plastic surgery: the story of nasal reconstruction from the Edwin Smith Papyrus to the twenty-first century. Plast Reconstr Surg. 2007;120(1):327-36. DOI: http://dx.doi.org/10.1097/01.prs.0000264445.76315.6d
2. Destro MWB. Reconstrução do nariz. In: Mélega JM, ed. Cirurgia plástica fundamentos e arte - princípios gerais. Rio de Janeiro: Medsi; 2002. p.912-29.
3. Gillies HD. Plastic surgery of the face. London: Oxford Medical; 1920.
4. Millard DR Jr. Reconstructive rhinoplasty for the lower two-thirds of the nose. Plast Reconstr Surg. 1976;57(6):722-8. PMID: 775518 DOI: http://dx.doi.org/10.1097/00006534-197606000-00007
5. Rohrich RJ, Barton FE, Hollier L. Nasal reconstruction. In: Aston SJ, Beasley RW, Thorne CHM, eds. Grabb and Smith's plastic surgery. 5th ed. Philadelphia: Lippincott-Raven; 1997. p.513-29.
6. Morais J. Reconstrução da pirâmide nasal. In: Carreirão S, Cardin V, Goldenberg D. Cirurgia Plástica, Sociedade Brasileira de Cirurgia Plástica. São Paulo: Atheneu; 2005. p.409-23.
1. Universidade Federal de Mato Grosso do Sul. Campo Grande, MS, Brazil
2. Santa Casa de Campo Grande-MS. Campo Grande, MS, Brazil
3. Hospital Regional de Mato Grosso do Sul. Campo Grande, MS, Brazil
4. Hospital Santa Rosa de Cuiabá, MT, Brazil
Institution: Associação Beneficiente Santa Casa de Misericórdia de Campo Grande, MS, Brazil.
Corresponding author:
Gustavo de Sousa Marques Oliveira
Av. Primeiro de maio, 335 - Sao Bento
Campo Grande, MS, Brazil Zip code 79004-620
E-mail: gustavomo49@hotmail.com
Article received: December 20, 2011.
Article accepted: September 2, 2012.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter