

Original Article - Year 2015 - Volume 30 -
Therapeutic options in the management of giant congenital nevus: Experience of the Plastic and Reconstructing Service at Hospital de Clínicas, Federal University of Paraná
Opções terapêuticas no manejo do nevus congênito gigante, experiência do Serviço de Cirurgia Plástica e Reaparadora HC-UFPR
ABSTRACT
INTRODUCTION: Several modalities are available for the treatment of giant congenital nevus (GCN). The surgical approach includes partial serial resection or total excision. Objective: To demonstrate the main therapeutic modalities in the treatment of GCN and to assess the incidence of location, age, and size of this lesion at the Plastic and Reconstructive Surgery Service of the Hospital de Clínicas, Federal University of Paraná.
METHODS: This retrospective study included patients who had undergone surgical treatment for GCN between January 2004 and January 2010. We collected data such as age, sex, treatment performed, number of surgeries carried out, evolution, and complications.
RESULTS: We evaluated 11 patients (8 female and 3 male). The average age was 12.4 years (range, 3-25 years). The GCN subtype most commonly found was intradermal melanocytic nevus, which accounted for 90.9% of cases, with melanocytic nevus accounting for the remaining 9.1%. No cases of melanoma were identified. The most common location was the head and neck. The average diameter of the lesions was 9.1 cm. The techniques used for the reconstruction included primary suture, local flaps, skin graft, and the use of expanders. In the follow-up period, 63.6% of the patients still presented a residual nevus, 27.3% underwent complete resection, and 9.1% were not monitored.
CONCLUSION: A higher incidence of GCN was observed in patients aged 3-25 years. The most common location was the face, and the average size was 9.1 cm. The main treatment of patients with GCN was splitting resection, which resulted in satisfactory outcomes.
Keywords: Nevus; Treatment; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O nevus congênito gigante (NCG) possui diversas modalidades de tratamento. A abordagem cirúrgica inclui a ressecção parcial seriada ou excisão total. Objetivo: Demonstrar as principais modalidades terapêuticas utilizadas para o tratamento do NCG e avaliar a incidência da localização, idade e tamanho destas lesões no Serviço de Cirurgia Plástica e Reparadora do Hospital de Clínicas da Universidade Federal do Paraná.
MÉTODOS: Estudo retrospectivo dos pacientes submetidos a tratamento cirúrgico do NCG no período de janeiro de 2004 a janeiro de 2010. Foram coletados dados como: idade, gênero, tratamento realizado, número de cirurgias realizadas, evolução e complicações.
RESULTADOS: Foram avaliados 11 pacientes, sendo 8 mulheres e 3 homens. A média de idade foi de 12,4 anos (3 a 25 anos). O subtipo mais encontrado foi o nevus melanocítico intradérmico correspondendo a 90,9% dos casos e 9,1% com nevus melanocítico composto. Não foram identificados casos de melanoma. A localização mais comum foi a região da cabeça e pescoço. O diâmetro médio das lesões foi de 9,1 cm.As técnicas utilizadas para reconstrução foram: sutura primária, retalhos locais, enxerto de pele e uso de expansores. No seguimento, 63,6% dos pacientes apresentavam ainda nevus residual, 27,3% apresentaram ressecção completa e 9,1% perderam seguimento.
CONCLUSÃO: Foi observada maior incidência de NCG na faixa etária de 3 a 25 anos, sendo a localização mais comum na face e com tamanho médio de 9,1cm. O principal tratamento instituído para os pacientes com NCG foi a ressecção parcelada, com bons resultados.
Palavras-chave: Nevo; Tratamento; Procedimentos cirúrgicos reconstrutivos.
Giant congenital nevus (GCN) is a rare and disfiguring disease, with an incidence of approximately of one case per 20,000 births. GCN causes psychological distress for both patient and family. This condition results from an abnormal abundance of neuroectodermal melanocytes in ectopic locations1,2. The risk of malignant transformations is controversial, varying between 1.8% and 45% of cases, and depends on the number and size of lesions and the age of the patient. However, there is an ongoing debate about the magnitude of this risk and whether it applies to all congenital nevi or only larger congenital nevi. In a meta-analysis, the average risk of GCN malignant transformation was 8.2%. Small congenital nevi present cumulative risks when people are aged at least 60 years and become malignant in 4.9% of cases3,4.
The treatment of GCN aims for the complete excision of ectopic nevus cells and includes surgical and non-surgical approaches. The surgical approach relies on partial serial resection or total excision. When possible, complete resection and closure using primary suture should be performed. Grafts or skin flaps can be used to cover the wound due to resection. The use of tissue expanders is an alternative for severe cases and requires at least two surgeries2.
OBJECTIVE
The aim of this study was to assess the main therapeutic approaches used for the treatment of GCN and to evaluate the incidence of location, age, and size of these lesions at the Plastic and Reconstructive Surgery Service of the Hospital de Clínicas, Federal University of Paraná.
METHODS
This was a cross-sectional study included patients with GCN who had undergone surgical treatment at the Hospital de Clínicas, Federal University of Paraná, between January 2004 and January 2010. The patients were identified in the record books in which the performed surgeries were registered. The following data were collected after reviewing the medical records: age, sex, type of treatment performed, number of surgeries, evolution, and complications. This project was registered in the National Information System on Research Ethics Involving Human Beings.
RESULTS
We evaluated 11 patients (eight female [72.7%] and three male [27.3%] patients), for a total of 17 lesions. The average age of the patients at the time of the surgery was 12.4 years, ranging from 3 to 25 years. Regarding the histology, the GCN subtype of intradermal melanocytic nevus most commonly found, detected in a total of 10 patients (90.9%). One patient (9.1%) presented a compound melanocytic nevus. No cases of melanoma were identified. The most common location of the lesions was the head and neck (Figure 1). Three patients presented with more than one nevi, varying from two to four. The average size of the lesions, measured according to the largest diameter, was 9.1 cm (range, 2.1-30 cm).

Figure 1. A: Congenital melanocytic nevus on the left Malara; B: Aspect after positioning the expander for the preparation of the flap; C: Aspect after nevus excision and frontal flap rotation to close the resected area and maintain the vascular pedicle of the flap; D: Aspect after the release of the flap's pedicle.
The surgical technique most commonly used was local flap rotation (Figure 2). The average number of surgeries performed per patient was two and varied from one to five.
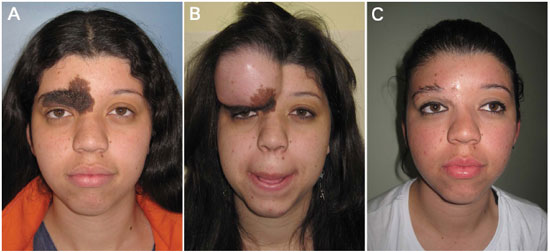
Figure 2. A: Congenital melanocytic nevus in the forehead and brow area; B: Aspect after positioning the expander for the preparation of the flap; C: Aspect after nevus excision and frontal flap rotation, to close the resected area.
We detected the occurrence of two complications: a mild hypertrophic scar on the left armpit in one patient, and an unaesthetic scar on the face in another patient. However, these patients had previously undergone a dermabrasion procedure at another service. The evolution of the patients is illustrated in Figure 3.
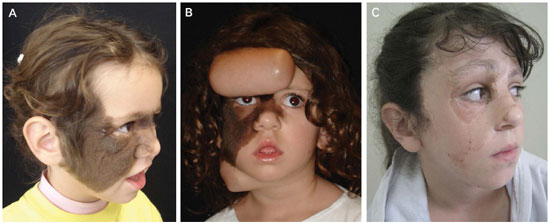
Figure 3. Congenital melanocytic nevus in the region of the right hemiface and nasal dorsum; B: Aspect after positioning the expander for the preparation of the flap; C: Aspect after nevus excision and frontal flap rotation to close the resected area.
DISCUSSION
Melanocytic lesions with a diameter larger than 20 cm in adults or occupying over 1% of the head and neck area or 2% of the body surface in other locations are known as GCN1,5. We approach these lesions at an early stage, mainly in childhood and pre-puberty, to avoid the risk of malignancy, which occurs in 50% of cases until the third year of life and in 75% until puberty. In our service, treatment is begun at puberty because of difficulty in accessing the lesion and the delay in receiving proper care.
Multiple lesions are common and require a more detailed evaluation of the therapeutic approach. Multiple nevi occurred in approximately one-third of the cases we analyzed. However, we did not change our approach on this basis. The minimally invasive methods, such as dermabrasion procedures, curettage, laser therapy, shave excision, and chemical peeling, are less traumatic therapeutic approaches. However, they do not decrease the risk of malignant transformation of the lesions and may hinder clinical monitoring, since the melanocytic cells are not removed8. Therefore, they are indicated in our service.
There are multiple approaches to this disease, and the approach can be individualized for each patient. In our service, we performed serial partial resection of these lesions and obtained satisfactory long-term aesthetic results and acceptable adherence during the follow-up period. Only two patients have not been monitored. In the other three cases, complete resection was performed. Combined treatment modalities are often necessary, especially for head and neck lesions, since these involve different anatomical structures. In this case, we used split resections associated with tissue expanders.
It is necessary to acquire an extensive knowledge for GCN using studies focused on the natural history, complications, and even genetics. When required, it is important to obtain a strict control of residual lesions, new advances in forms of treatment, and development of new techniques. Improvements in surgical technique, including that in tissue expanders, synthetic grafts, and the association of non-surgical and surgical treatments, ameliorated the quality of the scars and decreased residual lesions.
CONCLUSION
We observed a higher incidence of GCN in patients aged 3-25 years. The most common location of these lesions was the face, and the average size was 9.1 cm. The main treatment in patients with GCN was splitting resection, which resulted in satisfactory outcomes.
REFERENCES
1. Williams ML, Pennella R. Melanoma, melanocytic nevi, and other melanoma risk factors in children. J Pediatr. 1994;124(6):833-45. DOI: http://dx.doi.org/10.1016/S0022-3476(05)83168-3
2. Castilla EE, da Graça Dutra M, Orioli-Parreiras IM. Epidemiology of congenital pigmented naevi: I. Incidence rates and relative frequencies. Br J Dermatol. 1981;104(3):307-15. PMID: 7213564 DOI: http://dx.doi.org/10.1111/j.1365-2133.1981.tb00954.x
3. Krengel S, Hauschild A, Schäfer T. Melanoma risk in congenital melanocytic naevi: a systematic review. Br J Dermatol. 2006;155(1):1-8. PMID: 16792745 DOI: http://dx.doi.org/10.1111/j.1365-2133.2006.07218.x
4. Zaal LH, Mooi WJ, Sillevis Smitt JH, van der Horst CM. Classification of congenital melanocytic naevi and malignant transformation: a review of the literature. Br J Plast Surg. 2004;57(8):707-19. PMID: 15544766 DOI: http://dx.doi.org/10.1016/j.bjps.2004.04.022
5. Ruiz-Maldonado R, Tamayo L, Laterza AM, Durán C. Giant pigmented nevi: clinical, histopathologic, and therapeutic considerations. J Pediatr. 1992;120(6):906-11. PMID: 1593350 DOI: http://dx.doi.org/10.1016/S0022-3476(05)81958-4
6. Heffel DF, Thaller S. Congenital melanosis: an update. J Craniofac Surg. 2005;16(5):940-4. DOI: http://dx.doi.org/10.1097/01.scs.0000179751.29284.51
7. Clemmensen OJ, Kroon S. The histology of "congenital features" in early acquired melanocytic nevi. J Am Acad Dermatol. 1988;19(4):742-6. DOI: http://dx.doi.org/10.1016/S0190-9622(88)70231-5
8. Arneja JS, Gosain AK. Giant congenital melanocytic nevi of the trunk and an algorithm for treatment. J Craniofac Surg. 2005;16(5):886-93. DOI: http://dx.doi.org/10.1097/01.scs.0000183356.41637.f5
9. Lanier VC Jr, Pickrell KL, Georgiade NG. Congenital giant nevi: clinical and pathological considerations. Plast Reconstr Surg. 1976;58(1):48-54. PMID: 935278 DOI: http://dx.doi.org/10.1097/00006534-19760700000008
10. Kopf AW, Bart RS, Hennessey P. Congenital nevocytic nevi and malignant melanomas. J Am Acad Dermatol. 1979;1(2):123-30. DOI: http://dx.doi.org/10.1016/S0190-9622(79)70009-0
Universidade Federal do Paraná. Curitiba, PR, Brazil
Institution: Serviço de Cirurgia Plástica e Reaparadora HC-UFPR, Curitiba, PR, Brazil.
Corresponding author:
Renato da Silva Freitas
Rua General Carneiro, 191
Curitiba, PR, Brazil Zip code 80860-900
E-mail: dr.renato.freitas@gmail.com
Article received: December 21, 2011.
Article accepted: March 15, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter