

Original Article - Year 2015 - Volume 30 -
Treatment of open wounds of the leg by using local flaps
Tratamento das áreas cruentas de perna com retalhos locais
ABSTRACT
INTRODUCTION: Until the 70s, repairing loss of tissue in the leg was almost always difficult, or even impossible. Currently, only the most experienced surgeons are able to repair open wounds of the leg. Nevertheless, several reliable and simple techniques are currently available. This work aimed to evaluate repair techniques for leg wounds by using local tissues.
METHOD: The authors performed a retrospective study of cases of leg reconstruction using local flaps. Dermoadipose, fasciocutaneous, fasciosubcutaneous, and muscle flaps were used.
RESULTS: Seventy patients who had open areas in the leg due to tibial fractures, osteomyelitis, ischemic tissue loss, chronic ulcer, or skin tumor underwent surgery. Results were evaluated according to etiology, type of surgical procedure, and complications.
CONCLUSIONS: The option of treating open wounds of the lower limbs by using local flaps is very valid. Selection of the flap type depended on local conditions in the leg, and the anatomical region affected. In the upper third of the leg, we used fasciocutaneous flaps, based on the vascular network of the knee, or gastrocnemius flaps. In the middle third of the leg, we used the soleus muscle as the primary flap, and fasciosubcutaneous flaps in the calf region. In the lower third of the leg, a fasciosubcutaneous flap of the calf was primarily used.
Keywords: Gastrocnemius muscle/surgery; Soleus muscle/surgery; Leg trauma/surgery; Perforator flap/surgery.
RESUMO
INTRODUÇÃO: Até os anos 70, a reparação de perdas de substância na perna representava, quase sempre, um problema de solução muito difícil ou, até, insolúvel. Atualmente, embora ainda constitua um campo para os mais experientes, as áreas cruentas na perna já contam com várias técnicas confiáveis e algumas relativamente simples para sua reparação. Este trabalho visa equacionar condutas reparadoras de feridas de perna, utilizando tecidos locais.
MÉTODO: Estudo retrospectivo pela análise de casos de reconstrução de perna com retalhos locais realizados pelos autores. Foram incluídos os retalhos dermoadiposos, fasciocutâneos, fasciossubcutâneos e musculares.
RESULTADOS: Foram operados 70 pacientes que possuíam áreas cruentas na perna, em consequência de fratura de tíbia, osteomielite, perda tecidual isquêmica, úlcera crônica e tumoração de pele. Os resultados foram avaliados segundo etiologia, tipo de procedimento cirúrgico e complicações.
CONCLUSÕES: A opção do tratamento de áreas cruentas de membros inferiores com retalhos locais é bastante válida. A escolha do retalho vai depender de condições locais da perna e da região anatômica afetada. No terço superior da perna, utilizamos retalhos fasciocutâneos baseados na rede vascular do joelho ou retalho de gastrocnêmio. Já no médio, os principais retalhos foram o solear e o fasciossubcutâneo de panturrilha. E, por fim, no inferior, o principal retalho usado foi o fasciossubcutâneo de panturrilha.
Palavras-chave: Músculo gastrocnêmio/cirurgia; Músculo sóleo/cirurgia; Traumatismos da perna/cirurgia; Retalho perfurante/cirurgia.
The development of repair procedures used to cover open wounds of the leg has directly accompanied the evolution of plastic surgery itself. Studies on the anatomy of small vessels, concepts of flap physiology, and technology that allowed the development of microsurgery, among many other procedures, radically changed reparative surgery of the leg.
The leg has characteristics that hinder treatment of pathology. For example:
the leg is covered by the skin having poor elasticity; there is little subcutaneous tissue, and in some areas, the skin practically overlies the bone surface; constituent structures are arranged in layers and separated by rigid septa; arterial vascularization is of the terminal type, and has a high incidence of atherosclerosis; venous return is hindered due to standing posture; there is frequent trauma of various types, as well as tumors and circulatory disorders; and its structures bear considerable weight.
Until the 70s, repairing loss of tissue in the leg nearly always was difficult to treat, or even impossible. Among the existing techniques, some were ineffective, others were labor-intensive or lengthy, and these frequently failed.
Currently, only the most experienced surgeons perform these procedures; nevertheless, several reliable and simple techniques are available for the repair of open wounds of the leg.
This work aims to analyze reparative techniques used to treat leg wounds, by using tissue from nearby areas. We described the results obtained during the treatment of lesions of the lower limbs using only local flaps, conducted at the University Hospital/Federal University of Rio de Janeiro (UFRJ), the Hospital Municipal Miguel Couto (HMMC), and Hospital Agnelo Ciótola. We also conducted a non-systematic literature review on this topic.
Anatomical background
By definition, the leg is the part of the lower limb between the femorotibial and ankle articulations.
The arterial vascularization of the leg involves the popliteal artery and branches as follows: articular network of the knee, tibialis anterior, fibular, tibialis posterior, dorsal network of the foot, and plantar. This vascular system is of relatively large caliber, and several smaller vessels branch out into the muscles, fascia, subcutaneous tissue, and skin.
In 1973, Daniel and Taylor1 observed that skin vascularization was conducted through direct muscular or perforator branches, laying the foundations for the use of muscle-skin flaps that revolutionized plastic surgery in recent decades.
The importance of the fascia in dermofat flap vascularization was underscored by Pontén2, in 1981. This author observed that the inclusion of fascia in reverse flaps of the calves increased viability. In addition, other studies characterized the vascularization of the subcutaneous and common routes of the septocutaneous vessels, allowing planning of fasciocutaneous flaps.
The anatomical study of the skin and muscle neurovascular territories conducted by Taylor and Palmer3 (1987), changed the concept of the fascial or myocutaneous axial flap.
Vascular diseases of the lower limbs are rather frequent, and should be taken into account when planning a flap in the leg.
Some of the muscles in the leg may be used as muscular or myocutaneous flaps, with no detriment to limb physiology. Among these, the most important are the gastrocnemius, with its two bellies, and the soleus, due to a good radius of rotation and tissue volume.
The leg subcutaneous tissue is firm and usually thin, in particular at the medial facet of the tibia and the lower third of the region, where bone and tendon surfaces are in contact with the skin and subjected to trauma.
The skin is firm and, inelastic, dystrophic changes are frequently observed due to circulatory disorders, and there may be discoloration and scarring. Since the legs are exposed during sports activities and on other occasions, the planning of flaps in women should consider aesthetics whenever possible.
METHOD
Retrospective analysis was performed through an active search of patient records, using the databases of the plastic surgery services of the University Hospital Clementino Fraga Filho/Federal University of Rio de Janeiro (HUCFF/UFRJ), and orthopedic and traumatology services of the Hospital Municipal Miguel Couto (RJ), and Hospital Agnelo Ciátola/Santa Casa de Misericórdia de Barra do Piraí (RJ). This study was approved by the ethics committees of these institutions.
We included all patients subjected to surgical procedures on the leg involving coverage of basic open wounds, the patellar tendon, stabilizing plates, or bone exposure.
Patients who underwent other types of surgery that did not include leg reconstruction with local flaps were excluded from the study.
Initial basic treatment of open fractures was performed, on average, during the first 24 to 48 hours after trauma, and comprised, in all cases, surgical-mechanical debridement prior to trans-skeletal traction, bipolar fixation, cast immobilization, or external fixation.
In closed fracture cases, we used plates and screws, Kirschner wire osteosynthesis, or bipolar fixation.
None of the patients were treated acutely for skin lesions (except in cases of tumor resection and bridle scars). All remaining patients were directed to us for treatment after a chronic skin wound was established. The average duration of an established wound prior to evaluation by a plastic surgeon was three weeks.
The size of the areas that needed treatment varied between 2 × 3 cm and 4 × 10 cm.
RESULTS
The case series comprised 70 patients with open wounds of the leg, with surgical, posttraumatic, and other etiologies. The average age was 44 years, with 52 (74.3%) males and 18 (25.7%) females.
Table 1 shows the distribution of patients according to the etiology of lesions. Table 2 describes the treatments used.


In most cases (72.9%), tibial fracture was the main etiological factor.
The treatment varied according to which third of the leg was affected. In the upper third, the most frequent treatment was the gastrocnemius muscle flap (Figure 1, Figure 2). In the middle third, the soleus muscle (Figure 3) was used, and in the lower third, the fasciosubcutaneous flap of the calf (Figure 4, Figure 5, Figure 6). Four patients with lesions in the proximal portion of the lower third underwent a soleus flap.

Figure 1. A - Skin necrosis in patellar region; B - Saphenous graft prepared by rotation; C - Three months after surgery.
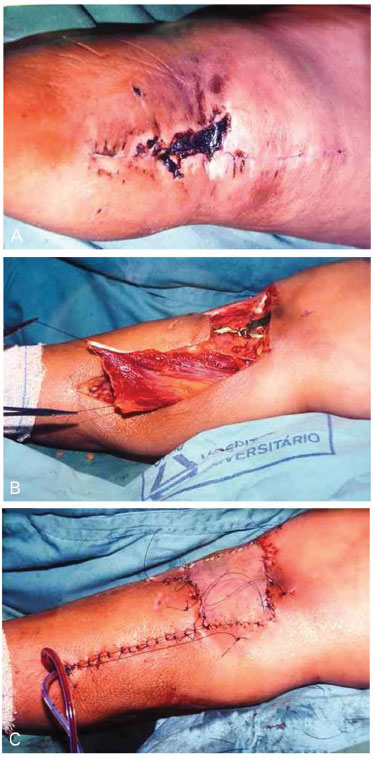
Figure 2. A - Skin necrosis in patellar region; B - Gastrocnemius muscle medial venter prepared by rotation and covering of stability plate of the fracture; C - Immediate postoperative with covering of muscle using a skin graft.
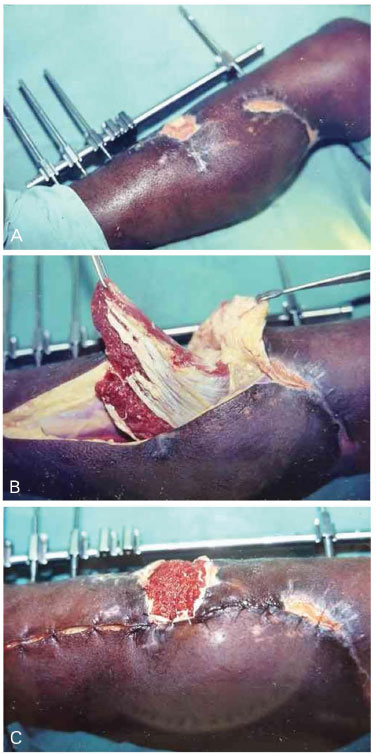
Figure 3. A - Exposed bone in middle third of the leg; B - Soleus muscle prepared for covering the raw area; Placed and prepared soleus to receive the skin graft.

Figure 4. A - Chronic ulcer in patellar region; B - Rotated subcutaneous fascia flap for covering the wound; C - Three months after surgery.
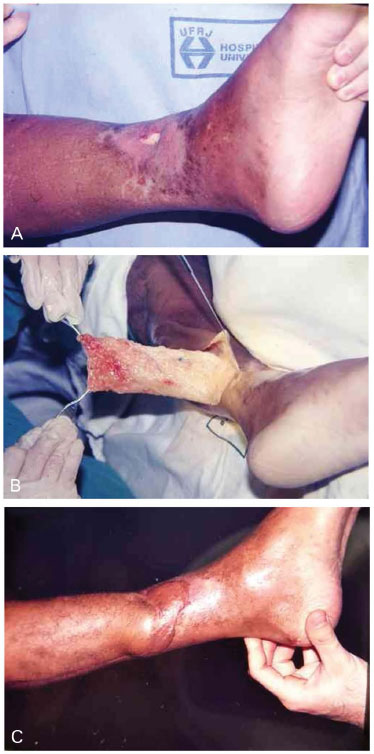
Figure 5. A - Exposed bone in the lower third of the leg; B - Elevated subcutaneous fascia flap; C - One year after surgery.

Figure 6. A - Calcaneal tumors; B - Subcutaneous fascia flap of the hamstring marking with distal pedicle; C - Rotated flap for covering the defect; D - Three months after surgery.
In one patient, there was extensive bone exposure in the upper and middle thirds, and combined soleus and gastrocnemius flaps were used. The lateral belly of the gastrocnemius was preserved. Walking abilities were maintained, but there was partial loss of limb strength.
The desired result was to cover the open area and protect deep structures, and all patients progressed adequately in this regard. Nine patients (12.9%) had mostly minor complications, which resolved in the immediate postoperative period (small hematoma), or in the late postoperative period (chemical debridement of superficial segmental necrosis).
A gastrocnemius flap was used to cover a 10 cm area over an exposed orthopedic metal plate in the middle third of the leg. There was distal failure of the flap and new exposure of approximately 2 cm of the plate. A fasciosubcutaneous flap of the calf with a distal pedicle solved the problem.
DISCUSSION
Few areas of the body have undergone as many radical changes in surgical treatment of skin lesions as the leg. Conceptual changes have been more significant than technical changes. Some concepts were antiquated, but knowledge acquired over time contributed to current insights about the vascular system, with its segmental and layered distribution; this allows the preparation of flaps containing very small pedicles, which overlap in some cases.
Progressive knowledge benefited other regions of the body, but only the leg presented so much difficulty and benefited so much3-10.
The initial landmark was the knowledge gained about the anatomy of small vessels, which was not addressed in the great anatomy or surgery treatises. The pioneering studies by Manchot (1883)10 and Salmon (1936)11 about skin vascularization remained forgotten for decades. When the occasion arose, a growing number of modern authors added more specific knowledge to these works3,7,12-15.
Curiously, microsurgery, which is a sophisticated procedure, preceded muscle and myocutaneous flaps. Fasciocutaneous flaps, which are simpler to perform, were the last to appear.
Integration of knowledge is possible from simple facts. Of utmost importance was the understanding that vascularization is layered in the limbs; although independent from each other, the layers maintain important connections. Wounds caused by crushing or compartment syndrome may destroy muscles through ischemia, while surface structures may remain intact. This also may occur in electrical burns2.
Knowledge about vascular pedicles of muscles, fascia, subcutaneous areas, and skin, as well as the segmental and layered distribution of this vascularization, led to use of each of these structures as independent units transformable into flaps.
Currently, leg flaps are almost always axial. As long as the anatomy of the region is known, it is possible to adapt the planned flap to the vascular axis.
Flaps using perforator vessels (vessels that perforate deep fascia, and are responsible for the vascular supply of specific skin or fasciocutaneous areas) were created to improve muscle salvage.
Schaverien and Saint-Cyr (2008) mapped perforator vessels from the three main vascular bundles of the lower limbs, identifying specific regions of greatest predictable use for the creation of pedicle flaps from perforators16.
This proposed individualization of perforator vessels led to free-style flaps. With the aid of a Doppler, it is possible to map local perforators in the limb for use as vascular pedicles, with flap planning based on the presence of these vessels, which may also be used for microsurgical procedures17. Rezende et al. 18 described a case series of 20 patients with defects in the lower third of the leg, who were treated with free-style flaps, with a cure rate of nearly 80%.
Of course, elasticity is low and extension from available tissues is limited; however, the constancy of pedicles and the layout of tissues in layers that are easily dissected allowed creation of flaps with great mobility. The use of expanders in the leg has limitations and specific contraindications, and was not within the scope of this study.
Nevertheless, there are some specific aspects associated with this region that may result in either good or bad results. Although the reluctance to perform reparative surgery in the leg has faded, care must be maintained. Mistakes in flap planning usually result in failure, and cause great morbidity.
Both arterial and venous vascular conditions should be carefully evaluated before and after surgery. Circulatory disorders are common, and may impair flaps that were apparently well-planned. On the other hand, immobilization after surgery, which is fundamental in most cases, is a predisposing factor for thromboembolic complications.
The role of microsurgical reconstruction in saving limbs depends greatly on vascular conditions, since it is possible to perform end-to-side anastomoses, avoiding loss of blood supply19.
As a basic principle that should guide any type of plastic surgery, the simplest procedures should be selected whenever possible, as long as they are efficient and reliable. Grafts should be used in superficial lesions, if the receptor bed permits, and when filling in over bone is not required. These may sometimes be used, even in cases where flaps are preferable, in patients who have clinical conditions that do not permit more extensive procedures.
Fasciocutaneous flaps are preferable to dermofat flaps, because of better vascularization, and to muscle flaps, because of lesser invasion. From an aesthetic point of view, however, fasciocutaneous or muscle flaps covered by partial skin grafts are less mutilating.
For well-trained teams, microsurgical flaps may be a good option due to local aesthetic appearance, in particular for extensive lesions in the leg and plantar region. However, these mutilate the donor area, and usually require a degreasing step in a second surgery.
The conditions of the receptor area constitute part of the healing process. Although muscle flaps can improve local vascularization, the bed must allow neovascular penetration. The presence of devitalized tissue or infection prevents the integration of the flap.
In an extensive case series of microsurgical reconstruction of the extremities, Godina20 demonstrated that the preparation of the receptor area becomes more difficult 72 hours after trauma, due to fibrosis and devitalized tissue resulting from incomplete debridement.
The reverse pedicle flap (distal), similar to the reverse sural flap, has revealed its great utility and versatility, especially for lesions in the lower third of the leg.
The dressing is a factor in success or failure; excessive compression leads to necrosis, whereas insufficient compression may lead to a hematoma. Drainage by aspiration is recommended, but not in all cases, since there may not be adequate space for the drain. Careful hemostasis and efficient immobilization are always recommended. Dressing must only be performed by trained personnel. Inappropriate procedures and inadequate dressings are responsible for many losses.
Reparative surgery of leg wounds currently relies on a wide range of procedures that are able to resolve most cases. The most simple and least invasive procedures should be chosen whenever possible.
Leg vascularization is segmental and layered, which enables creation of several types of flaps. Dividing the leg into three segments facilitates planning for flap preparation. The plastic surgeon should be familiar with different, equally effective techniques for each of these segments.
CONCLUSIONS
Trauma was the primary etiology of lesions in this study, responsible for approximately 73%, since the treating hospitals had a high volume of emergency cases.
For lesions in the upper and middle third of the leg, gastrocnemius and soleus muscle flaps were primarily used.
For lesions in the lower third of the leg, the fasciosubcutaneous flap was most commonly used, preserving the skin of the donor area.
Although reparative leg surgery no longer intimidates surgeons, it should still inspire respect.
REFERENCES
1. Daniel RK, Taylor GI. Distant transfer of an island flap by microvascular anastomoses. A clinical technique. Plast Reconstr Surg. 1973;52(2):111-7. PMID: 4578998
2. Pontén B. The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg. 1981;34(2):215-20. PMID: 7236984 DOI: http://dx.doi.org/10.1016/S0007-1226(81)80097-5
3. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41. PMID: 3567445 DOI:http://dx.doi.org/10.1016/0007-1226(87)90185-8
4. Barclay TL, Cardoso E, Sharpe DT, Crockett DJ. Repair of lower leg injuries with fascio-cutaneous flaps. Br J Plast Surg. 1982;35(2):127-32. PMID: 7044458 DOI:http://dx.doi.org/10.1016/0007-1226(82)90148-5
5. Lin SD, Lai CS, Chiu YT, Lin TM, Chou CK. Adipofascial flap of the lower leg based on the saphenous artery. Br J Plast Surg. 1996;49(6):390-5. PMID: 8881786 DOI:http://dx.doi.org/10.1016/S0007-1226(96)90008-9
6. Hartwell SW Jr, Evarts CM. Secondary coverage of pretibial skin defects. Report of four representative cases. Plast Reconstr Surg. 1970;46(1):39-42. PMID: 4914404
7. Mathes SJ, McCraw JB, Vasconez LO. Muscle transposition flaps for coverage of lower extremity defects: anatomic considerations. Surg Clin North Am. 1974;54(6):1337-54. PMID:4610850
8. Gumener R, Zbrodowski A, Montandon D. The reversed fasciosubcutaneous flap in the leg. Plast Reconstr Surg. 1991;88(6):1034-41. DOI: http://dx.doi.org/10.1097/00006534-199112000-00013
9. Franco T, Couto P, Gonçalves LFF, Franco D, Silva CC. Tratamento das exposições ósseas e tendinosas no terço distal da perna e no pé utilizando retalho fasciossubcutâneo reverso de panturrilha. Rev Bras Ortop. 1996;31(3):247-52.
10. Manchot C. The cutaneous arteries of the human body. In: Ristic J, Morain WD, eds. New York: Springer-Verlag; 1983.
11. Salmon M. Artères de la peau. Paris: Masson; 1936.
12. Carriquiry C, Aparecida Costa M, Vasconez LO. An anatomic study of the septocutaneous vessels of the leg. Plast Reconstr Surg. 1985;76(3):354-63. PMID: 3898166 DOI:http://dx.doi.org/10.1097/00006534-198509000-00003
13. Haertsch PA. The blood supply to the skin of the leg: a post-mortem investigation. Br J Plast Surg. 1981;34(4):470-7. DOI: http://dx.doi.org/10.1016/0007-1226(81)90061-8
14. McCraw JB, Dibbell DG. Experimental definition of independent myocutaneous vascular territories. Plast Reconstr Surg. 1977;60(2):212-20. PMID: 329302 DOI:http://dx.doi.org/10.1097/00006534-197708000-00007
15. Whetzel TP, Barnard MA, Stokes RB. Arterial fasciocutaneous vascular territories of the lower leg. Plast Reconstr Surg. 1997;100(5):1172-83. DOI: http://dx.doi.org/10.1097/00006534199710000-00016
16. Schaverien M, Saint-Cyr M. Perforators of the lower leg: analysis of perforator locations and clinical application for pedicled perforator flaps. Plast Reconstr Surg. 2008;122(1):162-70. DOI:http://dx.doi.org/10.1097/PRS.0b013e3181774386
17. Wei FC, Mardini S. Free-style free flaps. Plast Reconstr Surg. 2004;114(4):910-6. PMID:15468398 DOI: http://dx.doi.org/10.1097/01.PRS.0000133171.65075.81
18. Rezende MR, Rabelo NTA, Benabou JE, Wei TH, Mattar Junior R, Zumiotti AV, et al. Cobertura do terço distal da perna com retalhos de perfurantes pediculados. Acta Ortop Bras. 2008;16(4):223-9. DOI: http://dx.doi.org/10.1590/S1413-78522008000400007
19. Engel H, Lin CH, Wei FC. Role of microsurgery in lower extremity reconstruction. Plast Reconstr Surg. 2011;127 Suppl 1:228S-238S. DOI:http://dx.doi.org/10.1097/PRS.0b013e3182008e12
20. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78(3):285-92. DOI: http://dx.doi.org/10.1097/00006534-198609000-00001
1. Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
2. Sociedade Brasileira de Ortopedia e Traumatologia, Rio de Janeiro, RJ, Brazil
3. Sociedade Brasileira de Cirurgia Plástica, Rio de Janeiro, RJ, Brazil
4. Universidade Severino Sombra, Vassouras, RJ, Brazil
Institution: Serviços de Cirurgia Plástica do Hospital Universitário Clementino Fraga Filho da Universidade Federal do Rio de Janeiro (HUCFF/UFRJ), de Ortopedia e Traumatologia dos Hospitais Municipal Miguel Couto (Rio de Janeiro/RJ) e Agnelo Ciótola - Santa Casa de Misericórdia (Barra do Piraí/RJ), Rio de Janeiro, RJ, Brazil.
Corresponding author:
Diogo Franco
Rua Ramon Franco, 98, Urca
Rio de Janeiro, RJ, Brazil Zip code 22290-290
E-mail: contato@diogofranco.com
Article received: May 7, 2014.
Article accepted: March 15, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter