

Articles - Year 2004 - Volume 19 -
Single Digit Replantation in Outpatient Surgery: Experience of 120 Cases
Reimplante Unidigital Ambulatorial: Experiência de 120 Casos
ABSTRACT
We performed 120 single digit replantations on an outpatient surgery basis between 1994 and 2001. The levels of amputation were: proximal phalanx in 50 patients, proximal interphalanx in 21, distal interphalanx in 42 and metacarpophalanx in 7 patients. Trauma mechanism included: avulsion (31.7%) and guillotine (68.3%). The mean normothermal ischemia time was 8h (ranging between 6 -15h). Patients stayed in the hospital a maximum of 8 h after the surgery. All of them were told about the possibility of an arterial or venous thrombosis and instructed on how to identify it. Patients who believed any circulatory abnormality was occurrinq, telephoned the surgeon and were immediately assessed. Reassessment was performed in 20 patients, and circulatory deficits were confirmed in 15 patients. There was replantation loss in 12 of the latter patients. The replantation success rate was 90%, and the major determining factor was trauma mechanism and not the postoperative regimen. We suggest that single digit replantation be performed whe never there is an indication and that the availability of hospital beds should not be a decisive factor in the choice of the method of treatment of amputations and single digit devascularizations.
Keywords: Replantations; amputations; outpatient surgery
RESUMO
Realizamos 120 reimplantes unidigitais em nível ambulatorial entre 1994 e 2001. Os níveis de amputação foram: falange proximal em 50 pacientes, interfalangeana proximal em 21, interfalangeana distal em 42 e metacarpofalangeana em 7 pacientes. O mecanismo de trauma incluiu: avulsão (31,7%) e guilhotina (68,3%). O tempo médio de isquemia normotérmica foi 8 h (extremos 6-15h).
Os pacientes permaneciam em ambiente hospitalar no máximo 8 h após o término da cirurgia. Todos os pacientes foram orientados sobre as possibilidades de trombose arterial ou venosa e de que forma isso poderia ser identificado. Os pacientes que julgassem haver qualquer anormalidade circulatória ou que estivessem em dúvida telefonavam ao cirurgião que os avaliava imediatamente. A reavaliação foi realizada em 20 pacientes, mas o déficit circulatório comprovou-se em 15 pacientes. Destes, houve perda do reimplante em 12 pacientes.
A taxa de sucesso dos reimplantes foi de 90%, e o mecanismo do trauma foi o principal fator determinante e não o regime pós-operatório. Sugerimos que o reimplante unidigital seja realizado sempre que houver indicação e que a existência de leitos hospitalares disponíveis não seja o fator decisivo na escolha do método de tratamento das amputações e desvascularizações unidigitais.
Palavras-chave: Reimplantes; amputações; cirurgia ambulatorial
Finger amputations are freguent in our enviranrnent. Most result from occupational accidents. The socioeconomic impact of these wounds is extremely high, because they affect individuals in a productive age graup and lead to long periods away fram work, different degrees of seguela and, in most cases, permanent impairment.
The development of microsurgery technigues, after the work of Tamai and Komatsu(1) in 1965, was a breakthraugh in the treatment of these wounds by intraducing digit replantation into the therapeutic armamentarium of hand surgery. The functional, aesthetic and social impacts of the pracedure are remarkable, and enable individuals to return to their activities( 2,3.)
There is no consensus on the indication of single digit replantation(2-4). However, some situations, such as a thumb amputation, pose an absolute indication. Amputations in children, distal to the superficial flexor insertion and in the first and third fingers (zone III), have attained better results then other treatment modalities(2-5). Replantation may occasionally be indicated for professional or aesthetic reasons, for musicians or craftsmen, for example(2,3,6).
Patients submitted to replantations are hospitalized for observation and postoperative care by the medical and nursing staff, attentive to possible complications, such as arterial or venous thrombosis that reguire the surgical revision of anastomoses.
The major shortage of hospital beds in the Unified Health System (Sistema Único de Saúde-SUS) freguently leads to a conflicting and extremely stressful situation: a medical emergency that needs hospitalization but no beds available throughout the public SUS region. Amputations are even a more critical condition because any delay in replantation can be a determining factor in the postoperative prognosis. Working in these circumstances over many years led us to seek alternative solutions. Thus we began to reimplant single digit amputations on an outpatient surgery basis. The present article describes the experience in 120 consecutive cases.
PATIENTS AND METHODS
The study was carried out at the Plastic Surgery Service of Hospital São Lucas - PUCRS and at Clínica S.O.S. Mão - Porto Alegre - fram January 1994 to December 2001.
The levels of amputation were: praximal phalanx (PP) in 50 patients, proximal interphalanx (PIF) in 21, distal interphalanx (DIF) in 42 and metacarpophalanx (MP) in 7 patients. Injuries were more freguent in males (77 patients - 64.2%). The mean age of patients was 24 years (ranging fram 15 - 34). Trauma mechanisms were avulsion (38 patients - 31. 7%) and guillotine section (82 patients - 68.3 %). The mean normothermal ischemia time was 8 hours (ranging from 6 - 15h). The present study only included patients submitted to single digit replantation without any other associated injury, and who could not be hospitalized due to lack of available beds. All patients with reimplantations were hospitalized when beds were available. The sample was not obtained through randomization.
The anesthetic technique was brachial plexus block along with sedation and patients were monitored by an anesthetist. The postoperative hospital stay was eight hours. Some patients left the hospital with their arm still anesthetized (Figs. 1, 2, 3, 4).
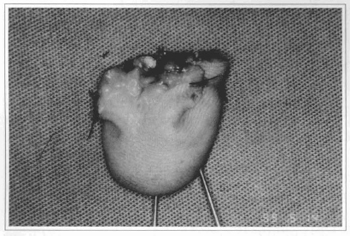
Fig. 1 - Amputated segment, volar view, 1st Finger.
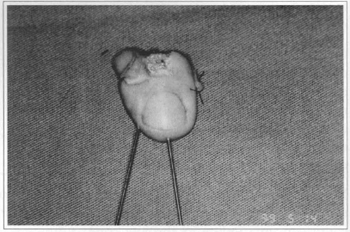
Fig. 2 - Amputated segment, dorsal view, Kirschner surures for osteosynthesis.
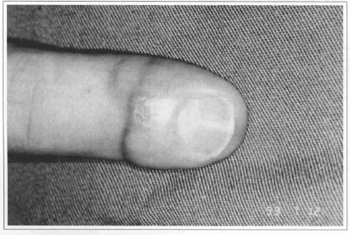
Fig. 3 - Final result.
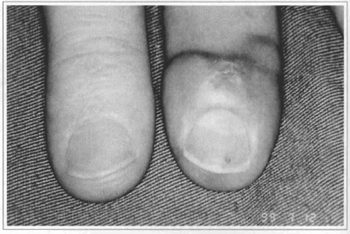
Fig. 4 - Comparative result against contralateral 1st Finger.
A postoperative pre-established protocol was followed: Immobilization with a palmar plaster splint, maintenance of raised upper limb and the body kept warm, postoperative analgesia (acetaminofen-500mg QID), oral anticoagulant (acetylsalicylicacid 150 mg, BID) and instructions to patients on possible circulatory problems. We used easily understood language, based on the color of the amputated segmento. If the finger became blue or white, the patient should immediately phone the surgeon in other to be assessed.
We concluded that patients understood instructions adequately, and were able to assess the viability of the reimplanted segment regardless of the level of schooling. All patients were reassessed immediately after they telephoned. Patients who did not consider that the reimplamed segment showed circulatory changes were reassessed one week postoperative in the outpatient clinic (Figs. 5 and 6).
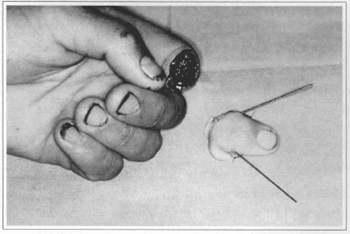
Fig. 5 - Amputation at the medium phalanx level, 1sr Finger, right hand.
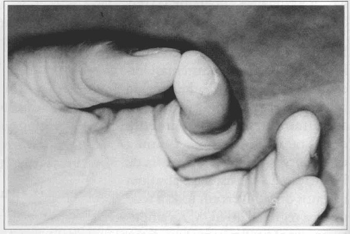
Fig. 6 - Functional Result.
RESULTS
Twenty patients telephoned in with a suspected abnormal circulatory change of the reimplanted segment (Table I). Contact was always within the first 24 hours after the surgical procedure. Re-intervention due to arterial and/or venous thrombosis was necessary for fifteen patients. Reanastomosis was successful in three patients (Table I). Again, ali re-interventions were carried out on a day-surgery basis.

In cases in which the reimplanted segment was lost, the trauma mechanism was avulsion, where the level of injury was zone 2 in eight patients and zone 3, in four patients. The final failure rate was 10 % (12 patients out of 120).
DISCUSSION
Classically, digit replantations have a specific indication for hospitalization to monitor the viability of the reimplanted segmem and for general postoperative care.
The difficulty in obtaining beds for SUS patients motivated us to perform replamations without hospitalization. Initially, it was difficult for our tearn to adopt the procedure because of uncertainty of success and due to the anxiety of leaving the postoperative monitoring of the reimp1anted segmem exclusively to the patient. As our series grew, the procedure became as regular as others in our service.
We obtained a 90% (108 patients) success rate, which is dose to that found in the literature and in our own service with hospitalized patients(4-8). All cases with loss of the reimplanted segmem were cases in which the injury mechanism was avulsion. The worst prognosis associated with this rype of amputation or devascularizarion is well described in the literature(9,11,12). The trauma mechanism was the major determinam of reimplantion success and not postoperative conditions (Figs. 7, 8,9,10).
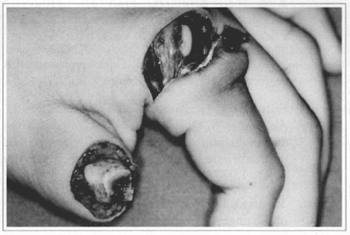
Fig. 7 - Thumb amputation, at the proximal phalanx level.
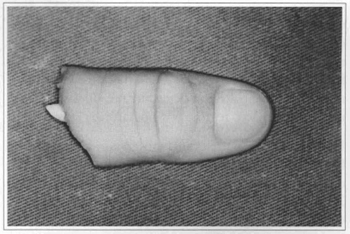
Fig. 8 - Amputated segmento.
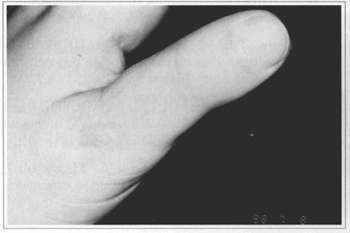
Fig. 9 - Final result.
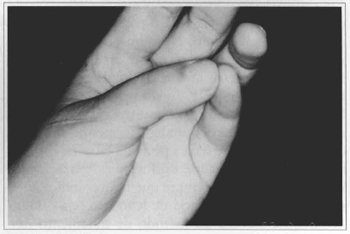
Fig. 10 - Functional result.
Another relevant aspect observed in the study was the ability of patients to assess the presence of postoperative thrombosis. Re-intervention was necessary in 15 of the 20 patients that reported circulatory abnormality in the reimplanted segment.
In selected cases, single digit replantation has a series of advantages in comparison to other treatment methods. No secondary reconstruction procedure attains the functional and aesthetic result of a successfully reimplanted and rehabilitated finger(3,13,14). Unfortunately, the shortage in SUS beds prevems many services from performing sing1e digit amputation reimp1antations, even in cases where replantation would be the first choice. We hope that the presem study will encourage single digit replantation whenever indicated and we suggest that the lack of hospital beds is not a decisive factor in choosing the method of treatment of finger amputations and devascularizations.
REFERENCES
1. Komatsu S, Tamai S. Successfull replantation of a completely cut off thumb. Plast Reconstr Surg 1968; 42:374-7.
2. Foucher G, Merle M, Braun JB. Distai digital replantations: one of the best indications for microsurgery lnt J Microsurg 1981; 3(4):263-70.
3. Chen CT, Wei FC, Chen HC, Chuang CC, Chen HT, Hsu WM. Distal phalanx replantation.Microsurg 1994; 15:77-82.
4. Soucacos PN, Beris AE, Touliatos AS, Vekris M, Pakos S, Varitimidis S. Acta Orthop Scand 1995; 66(264): 12-5.
5. Cheng GL, Pan DD, Zhang Nr, Fang GR. Digital replantation in children: A long-term followup study J Hand Surg 1998; 23A(4):635-46.
6. Boeckx W, Jacobs W, Guelinckx, Van de Kerchoven E. Late results in replanted digits. Is replamation of a single digit worthwhile? Actha Chir Belg 1992; 92:204-8.
7. Kim WK, Lirn JH, Han SK. Fingertip replamations: Clinical evaluation of 135 digits. Plast Reconstr Surg 1996; 98:470-5.
8. Manktelow RT, Mckee NH. Digital replantation: A functional assessment. Can J Surg 1979; 22(1):47-53.
9. Daoutis N, Gerostathopoulos N, Misitzis D, Ananostou S, Gianakopoulos P. Clinical analysis and evaluation of the function of replanted and revascularizated parts ofthe upper limbo Microsurg 1992; 13:178-81.
10. Yamano Y Replantation of the amputated distal part of the fingers. J Hand Surg 1985; 10A:211- 8.
11. Morrison WA, O'Brien B, McCLeod AM. Evaluation of digital replantation. A review of 100 cases. Orthop Clin North Am 1977; 8:295-308.
12. Furnas HI, Lineaweaver W, Buncke HJ. Blood loss associated with amicoagulation in patients with replanted digits. J Hand Surg 1992; 17A:226-9.
13. Kour AK, Phone MH, Chia J, Pho RWH. Digital replantations under local anaesthesia, Ann Acad Med Singapore 1995; 24S:68-72.
14. Eger M, Schmidt B, Torok G, Khodadadi J., Goldmann L. Replantation of upper extremities. Am J Surg 1974; 128:447-50.
I - Faculty of the PUCRS Medical School. Hand Surgery Specialist by AMB and the Brazilian Society of Hand Surgery.
II - Candidate Member to SBCP.
III - Faculty of PUCRS Medical School. Head ofthe Plastic Surgery Service of Hospital São Lucas - PUCRS.
Study performed at the Plastic surgery service of Hospital São Lucas of Pontifícia Universidade Católica (PUCRS) and at Clínica SOS Mão - Porto Alegre, RS.
Address for correspondence:
Jefferson Braga Silva, MD
Av.Ipiranga, 6690 Centro Clínico PUCRS, Cj. 216
90610-000 - Porto Alegre - RS Brazil
Phone / Fax: (55 51) 3315-6277 /3320-5040
e-mail: jeffmao@terra.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter