

Original Article - Year 2015 - Volume 30 - Issue 2
Surgical lipodystrophy correction associated with the use of antiretroviral therapy: An analysis of procedures performed and impact on the patients
Correção cirúrgica da lipodistrofia relacionada ao uso da terapia antirretroviral: Uma análise sobre os procedimentos realizados e o impacto sobre os pacientes
ABSTRACT
INTRODUCTION: Treatment of patients with acquired immunodeficiency syndrome should be complete and based on controlling the disease and the complications related to the use of antiretroviral medications, such as lipodystrophy. This study aimed to evaluate the main complaints, epidemiological aspects, and surgical procedures performed for lipodystrophy correction among patients receiving long-term antiretroviral therapy.
METHOD: In this retrospective study, data were collected from the medical records of 27 patients who underwent 36 surgical procedures associated with lipodystrophy correction, from March 2010 to June 2014, at the Plastic Surgery Service of the Hospital das Clínicas, Faculty of Medicine of Ribeirão Preto.
RESULTS: The average age of the patients was 47.2 years; 22.2% were men and 77.8% were women. The average duration of antiretroviral therapy (HAAR) was 12.1 years. The most frequent complaints were dorsal hump (44.4%), abdominal lipodystrophy (44.4%), and gluteal lipoatrophy (37.04%). The majority of patients (70.4%) had undergone surgery. The most common type of surgery performed was hump liposuction (carried out in 48.1% of the patients), followed by abdominal, back, or flank liposuction (44.4%) and gluteoplasty (22.2%). Among all 36 procedures performed, only 2 resulted in complications. The average postoperative follow-up period was 11.2 months. In total, 70.4% of patients were satisfied with the results of their procedure.
CONCLUSIONS: The success of surgical treatment of HAAR-induced lipodystrophy is based on proper preoperative selection as well as constant and prolonged follow-up. Improved self-esteem facilitates the adherence to antiretroviral drug treatment.
Keywords: Lipodystrophy; Antiretroviral therapy; Acquired immunodeficiency syndrome; Liposuction; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O tratamento de pacientes portadores da síndrome da imunodeficiência adquirida deve ser integral e se basear no controle da doença e das complicações relacionadas ao uso de medicações antirretrovirais, como a lipodistrofia. Esse estudo tem como objetivo avaliar as principais queixas, os aspectos epidemiológicos e os procedimentos cirúrgicos realizados para corrigir a lipodistrofia em pacientes em uso crônico de antirretrovirais.
MÉTODO: Estudo retrospectivo, no qual foram coletados dados dos prontuários de 27 pacientes submetidos a 36 procedimentos cirúrgicos relacionados à correção de lipodistrofia no período de março de 2010 a junho de 2014 no serviço de Cirurgia Plástica do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto.
RESULTADOS: A idade média dos pacientes foi 47,2 anos, 22,2% homens e 77,8% mulheres. O tempo médio de uso da terapia antirretroviral (TARV) foi de 12,1 anos. As queixas mais encontradas foram: giba dorsal (44,4%), lipodistrofia abdominal (44,4%) e lipoatrofia glútea (37,04%). Na maioria dos pacientes (70,4%), foi realizada uma cirurgia. Quanto às cirurgias, a lipoaspiração de giba foi realizada em 48,1% dos pacientes, seguida da lipoaspiração de abdome, dorso ou flancos (44,4%) e gluteoplastia (22,2%). Entre todos os 36 procedimentos realizados, apenas dois apresentaram complicações. O tempo médio de seguimento pós-operatório foi de 11,2 meses. Do total, 70,4% dos pacientes mostraram-se satisfeitos após os procedimentos.
CONCLUSÕES: O sucesso do tratamento cirúrgico da lipodistrofia causada pelo uso da TARV baseia-se na seleção pré-operatória adequada e em seguimento constante e prolongado. A melhoria da autoestima facilita a adesão ao tratamento com antirretrovirais.
Palavras-chave: Lipodistrofia; Terapia antirretroviral; Síndrome da imunodeficiência adquirida; Lipoaspiração; Procedimentos cirúrgicos reconstrutivos.
Antiretroviral therapy-induced lipodystrophy is becoming increasingly common worldwide, as it is one of the most frequent disorders found in patients infected with human immunodeficiency virus (HIV)1-3. The development of antiretroviral drugs and the implementation of highly active antiretroviral therapy (HAART) has increased survival rates among these patients as well as the prevalence of lipodystrophy associated with the use of these medications4.
Lipodystrophy in HIV-infected patients is a syndrome causing both morphological alterations and metabolic disorders5-7. Morphologically, the patient can present with conditions ranging from a loss of fat in the subcutaneous tissue (lipoatrophy) to fat accumulation in unusual areas, such as the posterior cervical region5,8. These changes can be simultaneously manifested by the same patient. Regarding metabolic changes, the patient may present with dyslipidemia and increased insulin resistance. The mechanisms leading to lipodystrophy are quite complex, and symptoms can range from changes in lipid metabolism to changes in eating habits among patients treated with antiretroviral therapy5,6.
The consequences of body deformities induced by HAART include loss of social relationships, poor body image, and scarce adherence to the proposed treatment. Therefore, treating morphological changes caused by lipodystrophy is critical in HIV-infected patients, as it will significantly improve their quality of life and increase their adherence to the long-term use of antiretroviral drugs.
OBJECTIVES
Based on the experience of our service, this study aimed to assess the major complaints, epidemiological aspects, and surgical procedures performed for lipodystrophy correction among patients receiving long-term antiretroviral drug therapy.
METHODS
This study was conducted at the Plastic Surgery Service of the Hospital das Clínicas of the Faculty of Medicine of Ribeirão Preto, University of São Paulo, HC-FMRP-USP. This is a retrospective, observational, and descriptive study in which data were collected from the medical records of 27 patients who underwent 36 surgical procedures associated with lipodystrophy correction in body areas other than the face between March 2010 and June 2014. The medical records of these patients were analyzed by the researcher. All patients had an indication for a surgical procedure according to the evaluation carried out by the plastic surgery team in outpatient consultations.
The inclusion criterion was that the patient needed to undergo one or more surgical procedures to correct lipodystrophy while receiving long-term antiretroviral drug therapy. All patients were referred to our service by the public health network for an outpatient evaluation of the disturbance associated with a poor body fat distribution caused by HAART. We then analyzed the main complaints of the patients and the indications for surgical correction of lipodystrophy.
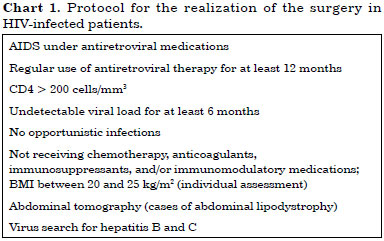
To undergo surgery, patients had to fulfill all the criteria of the protocol established by the Plastic Surgery Service and described in Chart 1. This protocol was established by the Infectious Diseases Service of HCFM-RP to ensure the safety of both the patient and the plastic surgery team.
Patients were excluded from the study due to incomplete or incorrect medical record data or if they underwent procedures related to face lipodystrophy correction, as these are performed by the dermatology team in our service.
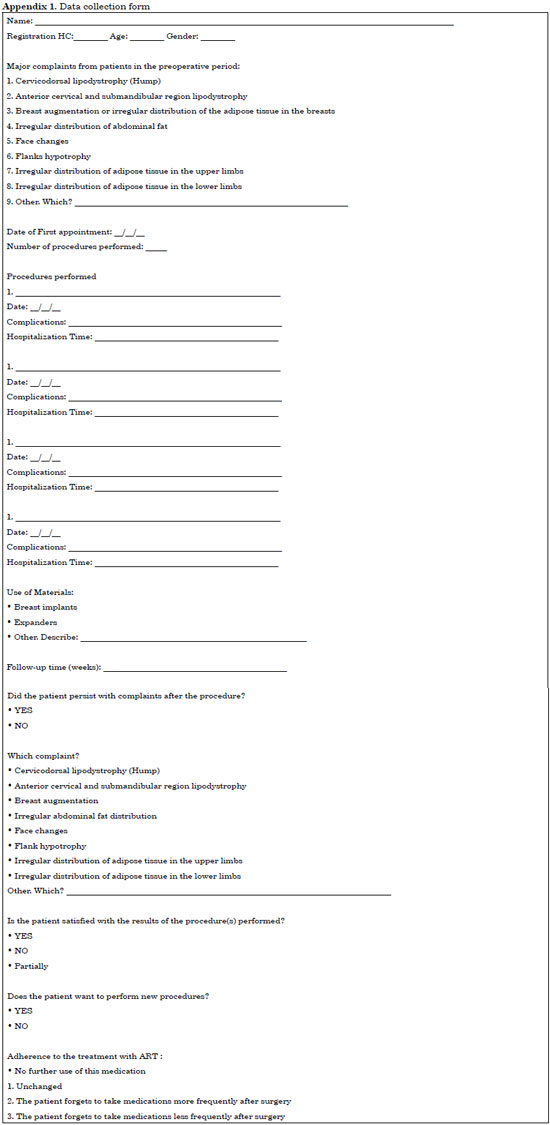
We used a form for the collection of the data (Appendix 1) from medical records stored at the Medical Archive and Statistics Service (MASS) and in the database of the Plastic Surgery Service of HC-FMRP.
After the collection and compilation of data, we verified the following variables: age, gender, history of patient complaints, duration between the date of the first consultation and the time of the first surgery, number of procedures performed, type of procedure(s) performed, complication rate, use of prostheses or expanders, follow-up, patient satisfaction in the postoperative period, requirement for new procedures, and patient adherence to HAART.
Study completion was based on the Brazilian Code of Medical Ethics in the Declaration of Helsinki and Resolution 196/96 of the National Health Council of 1996. The study was approved by the Research Ethics Committee of the Hospital das Clínicas of the Faculty of Medicine of Ribeirão Preto, under the protocol CAEE 33897514.9.0000.5440.
RESULTS
The age of the patients analyzed ranged from 36 to 68 years, with an average age of 47.18 years (median, 47 years) ± 8.85 years. Of the 27 patients analyzed, 18.72% were older than 40 years and 85.18% were 40 years or older. Of the group analyzed, 6 (22.2%) were men and 21 (77.8%) were women. The body mass index (BMI) of the patients ranged from 18.7 to 27.4 kg/m2, with an average of 23.58 kg/m2. Only 3 patients had a BMI above or below the values of the service's protocol (2 above 25 kg/m2 [25.3 kg/m2 and 27.4 kg/m2] and 1 below 20 kg/m2 [18.7 kg/m2]).
Most of the patients studied had been taking antiretroviral drugs for a long time, and the average duration of use was 12.1 years. Only 11.1% had used these medications for less than 8 years.
Taking into account the comorbidities reported by the patients, 59.2% did not present with any comorbidities, whereas 22.2% presented with dyslipidemia, 22.2% with hypertension, and 11.1% with type 2 diabetes mellitus under treatment for depression.
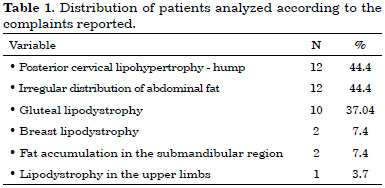
The complaints that were most commonly made by patients who submitted to surgical procedures included posterior cervical region lipohypertrophy as well as hump and irregular distribution of abdominal fat (44.4% each). Gluteal lipoatrophy was present in 37.04% of patients, whereas 7.4% complained of submandibular fat accumulation and breast lipodystrophy. Only 3.7% of patients complained of upper limb lipodystrophy (Table 1).
The average duration between the indication for surgery and time of the first procedure was 111 days, with a range of 8 to 386 days. Most patients (70.4%) underwent only 1 surgery, whereas 29.6% had 2 or more procedures in the period analyzed.
The most frequent surgery performed was hump liposuction (carried out in 48.1% of the patients), followed by abdominal, back, or flank liposuction (44.4%) and gluteoplasty (22.2%) with silicone prostheses (11.1%) or fat grafting (11.1%). The other surgeries performed included conventional abdominoplasty, fat grafting on the knees, submental liposuction, and reducing mastoplasty. Among all the 36 procedures performed, only 2 resulted in complications (i.e., wound dehiscence after gluteoplasty with silicone prosthesis and a pubic abscess that developed in a patient who underwent conventional abdominoplasty).
The average postoperative follow-up period was 11.2 months, with a range of 2 to 32 months. Among the patients studied, 40.8% stopped complaining about lipodystrophy after the first procedure, whereas 59.2% continued complaining about fat distribution in other body segments. The most frequent complaint was abdominal lipodystrophy (present in 33.3% of the patients), followed by submental lipohypertrophy and gluteal lipoatrophy (14.8%).
Despite the persistence of some complaints, most patients (70.4%) expressed satisfaction after the surgical procedures, whereas 25.9% were partially satisfied and only 3.7% were unsatisfied. Among the patients studied, 59.2% wanted to undergo new procedures, and 40.8% did not want to have any more surgeries.
DISCUSSION
The treatment of lipodystrophy associated with the use of antiretroviral drugs is quite complex and requires a multidisciplinary team trained and prepared to treat these patients. When they arrive for their consultation with the plastic surgeon, the patient should be examined as a whole, taking into account epidemiological factors as well as complaints and expectations regarding the treatment proposed. The current clinical conditions, complications inherent in each case, and the use of antiretroviral therapy should be evaluated, as well as which procedure should be performed for each individual.
Epidemiological factors such as age and gender are relevant when choosing the procedure to be performed. Several studies show that lipodystrophy in patients receiving antiretroviral therapy appears approximately 10 years after the use of these medication4,5. Therefore, it makes sense that the average age of the patients presenting to our Plastic Surgery Service for lipodystrophy correction in this study was 47.18 years, as according to the national and international literature, the average age at which patients with HIV start antiretroviral therapy is 37 years.1,2,9.
In several studies, male gender is considered to be a protective factor in the development of lipodystrophy in patients who are taking antiretroviral drugs1. It follows that, worldwide, there is a predominance of female patients seeking plastic surgery to correct the changes in body fat distribution induced by disorders associated with HAART.
The majority of patients with lipodystrophy induced by HAART seeking plastic surgery for the correction of this disorder had a BMI within the normal range (i.e., between 18 and 25 kg/m2)1,8. In this study, the average BMI was 23.58 kg/m2, which is within the range established by the service's protocol (25 > BMI > 20 kg/m2; Table 1). However, 3 patients did not have a BMI that fit within this range: one patient had a BMI of 18.7 kg/m2, and the others had BMIs of 25.3 kg/m2 and 27.4 kg/m2, respectively. These 3 individuals underwent dorsal hump liposuction. This situation does not fully meet the protocol regarding BMI values; therefore, it is important to consider an individual assessment to judge the safety of the procedures. In these cases, the surgeries were carried out only because they were shorter and there were no major nutritional restrictions or preconditions that could interfere with the safety and final outcome.
We should take into account that, in addition to aesthetic disorders, there are a number of metabolic disorders related to the use of HAART. Changes in glucose tolerance, insulin resistance, dyslipidemia, and hypertension are frequently observed in HAART patients, who present with the same disturbances as individuals with metabolic syndromes. Therefore, lipodystrophy can be associated with an increased cardiovascular risk, which motivates the candidates to receive a higher level of pre- and postoperative care for surgical procedures4.
Patients with lipodystrophy usually have low self-esteem and have already undergone different treatments due to their underlying disease. These are, in most cases, patients with multiple complaints regarding both their appearance and the psychosocial damage associated with acquired immunodeficiency syndrome (AIDS) and its treatment. As for aesthetic complaints, the loss of subcutaneous tissue on the face and extremities as well as excess fat in certain body segments is mostly found in this group of patients. Excluding facial deformities, dorsal hump and abdominal lipodystrophy are among the most frequent complaints reported by these patients in several studies conducted worldwide1,8,10,11.
After an initial consultation with and individual analysis of all patients, we took into consideration the adequacy of the same protocol service, seeking to ensure the safety of both the patient and the team performing the procedure. As patients are usually not followed up by infectiologists of the HCFMRP service, in some cases, the delay from the time of initial consultation to the time of surgery is due to a lack of data for patients referred and the accomplishment of criteria established in the protocol described.
According to the Brazilian Ministry of Health, since 2004, a number of corrective surgeries for patients with AIDS who are receiving antiretroviral drug therapy were included in the table of the Hospital Information System of the Unified Health System-SIH/SUS. This table includes hump and abdominal wall liposuction, breast reduction, gynecomasty, fat grafting and gluteal reconstruction, and facial filling with fatty tissue and polymethylmethacrylate (PMMA)12. Most of these procedures were performed in this study, except those related to face lipodystrophy and gynecomasty correction. In a national scenario, given the increasing demand to perform these surgeries, the number of centers carrying out these interventions has increased in recent years13.
Once we identified the main complaints of the patients, we proposed the most appropriate treatment for lipodystrophy correction. In the international literature, dorsal hump is the procedure that is most commonly performed in patients with lipohypertrophy induced by the use of antiretroviral drugs, as this is the most frequent complaint among these patients and the best technique that can be used to correct this disorder1,2,8,10.
Abdominal lipodystrophy may vary considerably among patients and take several forms. Accumulation of visceral fat, apron abdominal fat, and deposit of adipose tissue in the flank and back are some of the main complaints among these patients. Therefore, there are several ways to treat this disorder, among which we highlight abdominal liposuction. This is a relatively effective procedure to correct excess fat in specific segments of the abdomen, as in most cases, the patients are not obese (the average BMI in this study was 23.5 kg/m2). There are very few studies in the world literature describing the correction of abdominal lipodystrophy in patients receiving HAART. However, we noticed in this study that liposuction associated with abdominoplasty in selected cases ensures a good final result in terms of the patient's satisfaction.
Gluteal lipoatrophy is listed among the most frequent complaints of these patients, causing aesthetic and functional damage in some cases. Some patients complain of difficulty in walking or sitting, which is due to atrophy in the region. Therefore, the correction of this disorder significantly improves the self-esteem and quality of life of patients with gluteal lipodystrophy. The surgical treatment performed is known as gluteoplasty, which is carried out either with the use of autologous fat graft or with prostheses. In different studies carried out in Brazil, this surgery results in satisfactory outcomes and high patient satisfaction rates14.
The complication rate of all these procedures is relatively low if we take into account the complication rate of these procedures in patients without HIV. The establishment of a strict protocol for the realization of the surgery and good nutritional status of patients is essential to avoid such complications.
The postoperative follow-up is essential for the full treatment of lipodystrophy in patients receiving antiretroviral therapy. The underlying disease should remain under control, and the patient often requires new surgical interventions (i.e., to correct previous surgeries or to perform procedures to repair other body segments). Hence, complaints related to a poor distribution of body fat generally persist in patients who have a prolonged follow-up period. Therefore, the treatment of lipodystrophy should be continued for long periods and often requires multiple surgeries. In this study, the follow-up period of the patients analyzed was relatively short (11.2 months on average), mainly because a large percentage of the patients studied (46.2%) had surgery less than 12 months from the day on which they were first evaluated.
Regarding the adherence to HAART, during the study period, patients often reported that the antiretroviral medication was responsible for the body changes they experienced. Therefore, many of them considered discontinuing therapy to improve their body image. We believe that the surgical treatment of lipodystrophy increases the probability that patients will adhere to HAARR, because it offers them a chance to improve their self-esteem.
However, our evaluation of patient satisfaction was difficult, because even though the patients assessed how satisfactory was the result of the surgery performed, they continued to be dissatisfied with lipodystrophy in other body regions. In our study, the vast majority of patients were satisfied or partially satisfied, as in the investigations that were conducted in other regions of the world. This supports the idea that the surgical procedures used for lipodystrophy correction are effective and capable of improving a patient's quality of life1,2,8,13.
CONCLUSION
The correction of lipodystrophy in HIV-infected patients receiving HAART is essential for the treatment of these patients. Surgical procedures used to manage these disorders not only improve the quality of life of the patients but also provide an even better reintegration of these individuals into society and minimize the possibility of HAART discontinuation. The success of this treatment is based on the establishment of an appropriate preoperative period and constant and prolonged follow-up.
REFERENCES
1. Zinn RJ, Serrurier C, Takuva S, Sanne I, Menezes CN. HIV-associated lipodystrophy in South Africa: the impact on the patient and the impact on the plastic surgeon. J Plast Reconstr Aesthet Surg. 2013;66(6):839-44.
2. Berhane T, Yami A, Alemseged F, Yemane T, Hamza L, Kassim M, et al. Prevalence of lipodystrophy and metabolic syndrome among HIV positive individuals on Highly Active Anti-Retroviral treatment in Jimma, South West Ethiopia. Pan Afr Med J. 2012;13:43.
3. Murray CJ, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9947):1005-70.
4. Caron-Debarle M, Lagathu C, Boccara F, Vigouroux C, Capeau J. HIV-associated lipodystrophy: from fat injury to premature aging. Trends Mol Med. 2010;16(5):218-29.
5. Martínez E. Disorders of fat partitioning in treated HIV-infection. Best Pract Res Clin Endocrinol Metab. 2011;25(3):415-27.
6. Magkos F, Mantzoros CS. Body fat redistribution and metabolic abnormalities in HIV-infected patients on highly active antiretroviral therapy: novel insights into pathophysiology and emerging opportunities for treatment. Metabolism. 2011;60(6):749-53.
7. Gallego-Escuredo JM, Villarroya J, Domingo P, Targarona EM, Alegre M, Domingo JC, et al. Differentially altered molecular signature of visceral adipose tissue in HIV-1-associated lipodystrophy. J Acquir Immune Defic Syndr. 2013;64(2):142-8.
8. Nelson L, Stewart KJ. Experience in the treatment of HIV-associated lipodystrophy. J Plast Reconstr Aesthet Surg. 2008;61(4):366-71.
9. Grangeiro A, Escuder MM, Cassenote AJ, Souza RA, Kalichman AO, Veloso VG, et al. The HIV-Brazil cohort study: design, methods and participant characteristics. PLoS One. 2014;9(5):e95673.
10. Shridharani SM, Mohan R. A 51-year-old man with HIV and cervicodorsal lipodystrophy (buffalo hump). JAMA. 2013;309(12):1289-90.
11. Domingo P, Estrada V, López-Aldeguer J, Villaroya F, Martínez E. Fat redistribution syndromes associated with HIV-1 infection and combination antiretroviral therapy. AIDS Rev. 2012;14(2):112-23.
12. Brasil. Ministério da Saúde. Portaria GM/MS nº 2582, de 02 de Dezembro de 2004. Inclui cirurgias reparadoras para pacientes portadores de AIDS e usuários de anti-retrovirais.
13. Araújo FV, Faiwichow L, Andrade A, Gurgel LP, Fernandes FS, Warde M. Logística do tratamento cirúrgico da lipodistrofia em paciente soropositivos para HIV/AIDS no Hospital do Servidor Público Estadual de São Paulo. Rev Bras Cir. Plást. 2010;25(supl.1):1-102.
14. Sakabe D, Scozzafave A, Bianco RM, Pinho DBM, Ferreira DL, Miranda FBS. Tratamento da lipoatrofia glútea secundária à terapia antirretroviral com inclusão de implantes de silicone. Rev Bras Cir Plást. 2010;25(supl.1):1-102.
1. Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Divisão de Cirurgia Plástica do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, Ribeirão Preto, SP, Brazil.
Corresponding author:
Jayme Adriano Farina Junior
Av. Bandeirantes, 3900 - Monte Alegre
Ribeirão Preto, SP, Brazil Zip code 14048-900
E-mail: jafarinajr@gmail.com
Article received: August 18, 2014.
Article accepted: April 21, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter