

Original Article - Year 2015 - Volume 30 -
Plication of the rectus abdominis muscles in one continuous and two planes
Plicatura dos retos do abdome em dois planos versus plano único contínuo
ABSTRACT
INTRODUCTION: The correction of diastasis of the rectus abdominis muscles is primarily performed using the plication technique, which involves a surgical procedure. To evaluate the efficacy and the surgical time necessary to correct diastasis of the rectus abdominis muscles using plication and sutures in one continuous or two planes.
METHOD: Twenty women with at least one pregnancy were included in the study. The study participants were randomized into two groups: the control group was subjected to plication in two planes, and the experimental group was subjected to plication using suture in one continuous plane with mono-nylon 2-0. The time required to perform each of these techniques was measured. For statistical analysis, the nonparametric Mann-Whitney test, Friedman test, and Wilcoxon test were used, and p-values of < 0.05 were considered statistically significant. All patients underwent ultrasonography before surgery, and at 3 weeks and 6 months postoperatively.
RESULTS: The plication technique was similarly effective in the two groups, achieving a long-term surgical outcome; however, the differences in the ultrasound measurements in the pre- and postoperative periods were statistically significant (p = 0.018). In addition, plication was performed in a significantly shorter time in the experimental group (p = 0.002).
CONCLUSION: Sutures in one continuous plane and in two planes were effective in correcting diastasis of the rectus abdominis muscles, with the maintenance of a long-term surgical outcome. In addition, the continuous suture technique can be performed in a shorter time.
Keywords: Abdominal wall; Abdominoplasty; Rectus abdominis muscles.
RESUMO
INTRODUÇÃO: A correção da diástase dos músculos retos do abdome é realizada principalmente pela sua plicatura, procedimento que consome muito tempo cirúrgico. O objetivo deste estudo é avaliar a eficácia e o tempo necessário para a correção da diástase dos retos do abdome comparando a plicatura com sutura contínua em plano único à plicatura em dois planos.
MÉTODO: Foram incluídas 20 mulheres com história de pelo menos uma gestação. Foram randomizadas em dois grupos, um submetido à plicatura dos retos do abdome em dois planos (controle) e outro à sutura em plano único contínuo (estudo) com mononylon 2-0. Mediu-se o tempo necessário para a realização de cada uma das técnicas. Para análise estatística, foram usados os testes não paramétricos de Mann-Whitney, Friedman e Wilcoxon, considerando estatisticamente significante p < 0,05. Todas as pacientes foram submetidas à ultrassonografia previamente à cirurgia, 3 semanas e 6 meses de pós-operatório.
RESULTADOS: A plicatura do grupo estudo mostrou-se tão eficaz quanto à do grupo controle, mantendo seu resultado em longo prazo, apresentando diferença estatisticamente significante (p = 0,018) na comparação das medidas pré e pós-operatórias. No grupo estudo, porém, a plicatura consumiu menor tempo cirúrgico para ser realizada, também com diferença estatisticamente significante (p = 0,002).
CONCLUSÃO: Com este estudo, pode ser concluído que tanto a sutura em dois planos como a em plano único contínuo são eficazes na correção da diástase dos retos do abdome e mantêm o resultado por longo tempo. Concluiu-se também que a técnica de sutura contínua demanda menor tempo para ser realizada.
Palavras-chave: Parede abdominal; Abdominoplastia; Reto do abdome.
The abdominal wall is the anatomical structure responsible for the protection of the abdominal viscera, and retains their position during changes in gravitational force and during increases in intraabdominal pressure. Diastasis of the rectus abdominis muscles is responsible for the protrusion of the abdominal wall, formation of hernias, and development of functional problems, including back pain. Many authors have proposed different strategies for the treatment of the deformities caused by muscle sagging in the abdominal wall. Plication of the anterior layer of the aponeurosis of the rectus abdominis muscles is the most common technique1-9.
Surgical outcomes should focus on the postoperative period, because the sutured region suffers opposing forces due to increased intraperitoneal pressure, tissue elasticity (the tendency of mobilized tissues to return to their original position), muscle contraction, and wound contraction1. Numerous studies have shown that the medial margins of the rectus abdominis muscles remain close to the midline six months after plication, using different types of suturing techniques1-11. In this context, abdominoplasty aims to ensure reliable suturing with lasting benefits.
In addition to the clinical outcomes to be achieved, the total time of surgery is important in the selection of the technique to be used. The selection of techniques that require shorter surgical time compared with those that are most frequently used will dictate favorable outcomes in the postoperative period. No prospective studies have compared the plication technique using two planes and one continuous plane with regard to the period and effectiveness of surgery.
Imaging examinations, including magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound (US), can be used to diagnose diastasis preoperatively, as well as to monitor the results postoperatively, assisting in the evaluation of recurrences5,12,13.
OBJECTIVE
The objective of this study was to evaluate the efficacy of plication and the total time of surgery necessary to correct diastasis of the rectus abdominis muscles using suture in a single continuous plane and in two planes.
METHODS
The patients enrolled underwent abdominoplasty without the performance of liposuction. The inclusion criteria were: female gender, history of at least one pregnancy, skin and subcutaneous tissue deformity of the abdominal region classified as Nahas type III7 (indication for the removal of all the skin and subcutaneous tissue between the umbilicus and the suprapubic region), musculoaponeurotic deformity classified as Nahas type A8 (classical diastasis of the rectus abdominis muscles secondary to pregnancy and with a good delineation of the waistline), and body mass index (BMI) of < 30 kg/m2. The exclusion criteria were: smoking, scars in the abdominal wall (except for Pfannenstiel incision for cesarean delivery), presence of abdominal hernias, history of deep vein thrombosis, chronic obstructive pulmonary disease, cancer, hypertension, diabetes or other chronic systemic diseases, and use of corticosteroids.
Twenty patients who met the inclusion and exclusion criteria were randomized into two groups. The control group underwent correction of diastasis of the rectus muscles by plication using sutures in two planes, and the experimental group underwent plication by using sutures in a single continuous plane. Of the 20 patients, 14 were selected because their postoperative period was > 6 months during the study period.
Before surgery, patients were subjected to US of the abdominal wall using a LOGIQ P6 system (GE Healthcare, USA) and an 11L probe (Jungwon-Gu Seongnam-Si, South Korea).
Two measurements were made for confirmation and recording of diastasis: the first at a height of 3 cm above the superior margin of the umbilicus, and the second at a height of 2 cm below the inferior margin of the umbilicus.
General anesthesia was administered with isoflurane and nitrous oxide, 0.5 to 1.0 mcg/kg of sufentanil, 200 mg of propofol, and 1 mg/kg of pancuronium (only during induction of anesthesia); 100 mg of tramadol was administered at the end of surgery.
Abdominoplasty was initiated with a suprapubic incision extended to the anterior superior iliac spine bilaterally. The aponeurotic flap was dissected using electrocautery (power of 35 W for dissection and coagulation), and diastasis was identified with methylene blue. The distances between the medial margins of the rectus abdominis muscles were measured with a ruler in the two levels predetermined for imaging examinations.
Diastasis of the rectus muscles in the control group was corrected with sutures in two planes, including reversed points every 0.4 cm in the first plane, and continuous sutures secured between every two stitches in the second plane. In the experimental group, plication was performed with continuous sutures secured between every two stitches in a single plane. The thread used in both groups was mono-nylon 2-0 (Ethicon, Somerville, NJ, USA).
The umbilical pedicle was fixed to the aponeurosis with simple mono-nylon 4-0. Subsequently, the flap was retracted for the resection of any excess and for umbilical transposition. Vacuum drainage was performed with a 4.8 mm-caliber drain (Portovac, Kalmédica, Campinas, Brazil), positioned under the flap and externalized in the suprapubic region, and maintained until an output of < 40 mL was achieved in 24 hours; suturing was performed in planes with 3-0, black and colorless 4-0, and 5-0 mono-nylon threads.
The time necessary for the performance of each technique and the total time of surgery were measured. The measurement of the total time of surgery was initiated from the moment of the suprapubic incision until the application of the last stitch to suture the flap. The plication period was measured from the moment that the needle pierced the aponeurosis for the first time until the last stitch was cut.
The patients were instructed to use an abdominal compressive garment for 30 days. The period of hospital stay was 24 hours, and early ambulation was encouraged on the first day after surgery.
The surgical outcome was monitored by clinical examination and the performance of US examinations 3 weeks and 6 months postoperatively. The differences in the values obtained in the preoperative and postoperative periods were used to determine the effectiveness of each technique. Clinical examinations were performed in all postoperative consultations, and were conducted on a weekly basis in the first month, and monthly up to six months postoperatively, followed by two additional consultations until the completion of a postoperative period of 12 months.
For statistical analysis, we used the nonparametric Mann-Whitney test, Friedman test, and Wilcoxon test, and p-values of < 0.05 were considered statistically significant. The Mann-Whitney test was used for independent samples and to make pairwise comparisons of individual variables. The Friedman test was used when paired data were available for the simultaneous comparison of three or more variables (qualitative and ordinal). The Wilcoxon test was used when both the magnitude and the direction of the changes could be determined to make pairwise comparisons of individual variables.
RESULTS
No serious complications were observed in the postoperative period, such as thromboembolic events or situations that required reoperation. Only two patients in the control group and one in the experimental group showed small-volume seroma, diagnosed clinically, or on US 3 weeks after surgery. These were treated by aspiration with a needle and syringe, and the largest seroma had a volume of 24 mL. Palpation on physical examination indicated the absence of recurrent diastasis in the patients evaluated (Figures 1 to 8). All patients in both groups reported being satisfied with the surgical outcome.

Figure 1. Outcomes in the preoperative and postoperative periods (3 months and 6 months).

Figure 2. Outcomes in the preoperative and postoperative periods (6 months and 12 months).

Figure 3. Outcomes in the preoperative and postoperative periods (1 month and 3 months).

Figure 4. Outcomes in the preoperative and postoperative periods (1 week and 2 months).

Figure 5. Outcomes in the preoperative and postoperative periods (1 month and 6 months).

Figure 6. Outcomes in the preoperative and postoperative periods (1 week and 3 months).

Figure 7. Outcomes in the preoperative and postoperative periods (1 week and 2 months).

Figure 8. Outcomes in the preoperative and postoperative periods (1 month and 6 months).
The follow-up and US examination 6 months postoperatively indicated that none of the patients had recurrent diastasis (Table 1 and Figure 9).
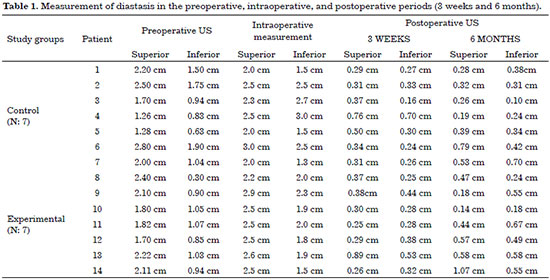
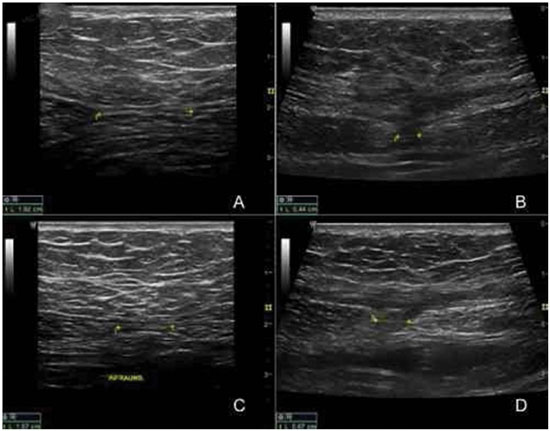
Figure 9. Ultrasound measurement of the rectus abdominis muscles of patient No. 11 in the experimental group. A) Preoperative measurement at a height of 3 cm above the umbilicus. B) Postoperative measurement after 6 months at a height of 3 cm above the umbilicus. C) Preoperative measurement at a height of 2 cm below the umbilicus. D) Postoperative measurement after 6 months at a height of 2 cm below the umbilicus.
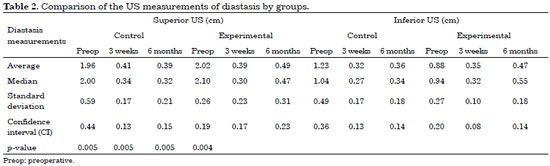
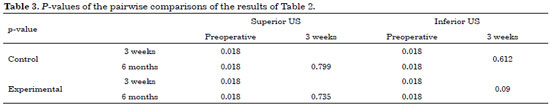
US measurements were compared in the two groups. The results of the Friedman test indicated statistically significant differences between the superior and inferior US measurements in both groups (Table 2). Therefore, to accurately determine the periods in which these differences occurred, the Wilcoxon test was used to make pairwise time comparisons (Table 3).
The analysis of the Wilcoxon test indicated the occurrence of significant differences in the preoperative period, but not in the postoperative period (three weeks and six months), demonstrating that both plication techniques corrected the diastasis (on US 3 weeks postoperatively), and achieved a long-term surgical outcome (on US 6 months postoperatively).
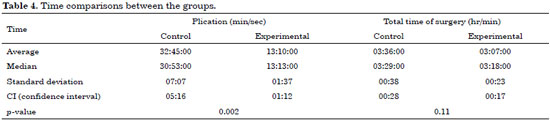
The period of plication and the total time of surgery were compared between the groups using the Mann-Whitney test. A statistically significant difference was observed between the groups only for the period of plication (Table 4); the average time in the control and experimental groups was 32 minutes and 45 seconds and 13 minutes and 10 seconds, respectively (p = 0.002).
DISCUSSION
An increase in intra-abdominal pressure, such as in pregnancy and obesity, can lead to diastasis of the rectus abdominis muscles. Therefore, tissue sagging increases progressively with subsequent pregnancies and aging; for this reason, the deformity of the abdominal wall tends to be more pronounced in multiparous women14. Plication of the rectus muscles aims to restore the integrity of the abdominal wall and provide reinforcement for the musculoaponeurotic layer of the abdomen2,15. Many strategies have been proposed for the execution of this procedure, and plication of the anterior layer of the rectus sheath with non-absorbable suture is most commonly used16.
The use of nylon threads proved to be an effective method to correct diastasis, and provided resistance against the increased level of intra-abdominal pressure, which is primarily responsible for the recurrent sagging of the abdominal wall10,11. Patients with morbid obesity or multiparous women present with recurrent diastasis of the rectus muscles more frequently14,17. The risk of recurrence has prompted the evaluation of the long-term outcome of plication of the anterior aponeurosis of the rectus abdominis muscles. Weight gain normally occurs by the accumulation of fat, both in the subcutaneous layer and in the abdominal cavity, increasing the tension in the plication area. However, this weight increase did not result in recurrence of diastasis in patients subjected to plication in two planes using absorbable or non-absorbable threads2,10.
The plication technique in two planes (the first plane with separate and inverted stitches and the second plane with continuous suture) was effective for the correction of diastasis, and did not lead to recurrence after long-term follow-up in the postoperative period2,4,10. The comparison of non-absorbable thread (nylon 2-0) with absorbable thread (polyglycolic acid 2-0) using this technique indicated that the surgical outcome lasted for at least 6 months, independently of the type of thread used3.
Nahas et al.11 reported a case of pregnancy after correction of diastasis with nylon 4-0 in two planes, and found no recurrence on clinical evaluation conducted 3 and 15 months after delivery. CT results indicated that the rectus abdominis muscles were juxtaposed in the midline in this same period. This result suggests that plication is resistant to the increase in intra-abdominal pressure, and can prevent the recurrence of diastasis.
The polyester thread used in plication in a single plane with separate stitches showed good results in the correction of diastasis6. Van Uchelen et al.5 used continuous suture with absorbable thread in a single plane for plication of the rectus abdominis muscles, but the outcome was less favorable after a 5-year follow-up period. A previous study used US for the late assessment of correction of diastasis, and observed recurrence in 40% of the cases5. Al-Qatan14 used midline plication in a single plane with non-absorbable thread (Prolene 1) and separate sutures in 20 multiparous women, and reported that the durability of the plication technique remained the biggest challenge in abdominoplasty, among patients with large musculoaponeurotic sagging, and that a modified plication technique or the use of mesh reinforcement could improve the outcomes.
In 2011, Elkhatib et al.13 concluded that plication of the rectus abdominis muscles is a long-term procedure that requires a 6- to 25-month follow-up postoperatively. The technique they used was continuous suture with nylon 0, and the long-term surgical outcome was confirmed by comparing MRI measurements in the preoperative and postoperative periods.
Both techniques - suture in one continuous plane and in two planes - can achieve favorable long-term surgical outcomes. However, according to Tadiparthi et al.15, suture in one continuous plane can be performed in a shorter time, and requires less suture material, thereby reducing complications and improving its cost-effectiveness. Similar results were obtained in this study. Diastasis of the rectus muscles is diagnosed by clinical evaluation, and can be confirmed by imaging studies. Several studies have used US, CT, and MRI, and all of these techniques have proved adequate1,2,4,10,12,18. Some minor limitations related to each of these techniques did not negatively impact their benefits. CT proved to be a reproducible technique; however, its use was limited due to the emission of radiation and its high cost. Elkhatib et al.13 used MRI and confirmed its advantage, because it is not operator-dependent, does not emit radiation, and is reproducible. Its limitation is related to the long procedure time and high cost. Although US is operator-dependent, it does not emit radiation, can be performed rapidly and repeated as often as necessary, and is low cost. Considering the absence of statistically significant differences between preoperative measurements (US) and intraoperative measurements (ruler), this technique proved to be a good choice for the evaluation of soft tissues of the abdominal wall.
Of all imaging techniques available, radiography is the least reliable method to evaluate diastasis, because it depends on the use of metal clips to identify the margins of the rectus abdominis muscles, which may be surrounded by fibrosis. Therefore, this technique may not accurately indicate the position of the muscles.
The choice of plication influences the total time of surgery. Complications due to prolonged surgical time have been reported, including deep vein thrombosis, pulmonary thromboembolism19, and anesthetic complications. Huang et al.20 confirmed that plication of the rectus abdominis muscles increases intraperitoneal pressure, culminating in a decrease in venous return, and increases the risk of thromboembolic events.
Little is known about the normal distance between the rectus abdominis muscles. Beer et al.18 reported that a width of the linea alba of 6-22 mm at a height of 3 cm above the umbilicus, and of 2-16 mm at a height of 2 cm below the umbilicus, were considered normal in nulliparous women with a BMI < 30 kg/m2.
In this study, the absence of recurrence of diastasis demonstrated that both suture techniques were effective in the correction of this deformity. Although there was no statistically significant difference in the total time of surgery, the decrease of 30 minutes in the average time using the continuous suture technique decreases the risk of complications in patients under surgery and anesthesia.
CONCLUSION
The results of the present study indicate that sutures in one continuous plane and in two planes are effective in correcting diastasis of the rectus abdominis muscles, and can achieve a long-term surgical outcome. However, the continuous suture technique can be completed in a shorter time.
REFERENCES
1. Nahas FX, Augusto SM, Ghelfond C. Should diastasis recti be corrected? Aesthetic Plast Surg. 1997;21(4):285-9. PMID: 9263554
2. Nahas FX, Ferreira LM, Ely PB, Ghelfond C. Rectus diastasis corrected with absorbable suture: a long-term evaluation. Aesthetic Plast Surg. 2011;35(1):43-8. DOI: http://dx.doi.org/10.1007/s00266-010-9554-2
3. Birdsell DC, Gavelin GE, Kemsley GM, Hein KS. "Staying power"--absorbable vs. nonabsorbable. Plast Reconstr Surg. 1981;68(5):742-5. PMID: 6270714 DOI: http://dx.doi.org/10.1097/00006534-198111000-00013
4. Nahas FX, Augusto SM, Ghelfond C. Nylon versus polydioxanone in the correction of rectus diastasis. Plast Reconstr Surg. 2001;107(3):700-6. DOI: http://dx.doi.org/10.1097/00006534-200103000-00008
5. van Uchelen JH, Kon M, Werker PM. The long-term durability of plication of the anterior rectus sheath assessed by ultrasonography. Plast Reconstr Surg. 2001;107(6):1578-84. DOI: http://dx.doi.org/10.1097/00006534-200105000-00046
6. Netscher DT, Wigoda P, Spira Melvin, Peltier M. Musculoaponeurotic plication in abdominoplasty: how durable are its effects? Aesthetic Plast Surg. 1995;19(6):531-4.
7. Nahas FX. A pragmatic way to treat abdominal deformities based on skin and subcutaneous excess. Aesthetic Plast Surg. 2001;25(5):365-71. DOI: http://dx.doi.org/10.1007/s00266-001-0025-7
8. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg. 2001;108(6):1787-95. DOI: http://dx.doi.org/10.1097/00006534-200111000-00057
9. Ferreira LM, Castilho HT, Hochberg J, Ardenghy M, Toledo SR, Cruz RG, et al. Triangular mattress suture in abdominal diastasis to prevent abdominal bulging. Ann Plast Surg. 2001;46(2):130-4. PMID: 11216606 DOI: http://dx.doi.org/10.1097/00000637-200102000-00007
10. Nahas FX, Ferreira LM, Augusto SM, Ghelfond C. Long-term follow-up of correction of rectus diastasis. Plast Reconstr Surg. 2005;115(6):1736-41. DOI: http://dx.doi.org/10.1097/01.PRS.0000161675.55337.F1
11. Nahas FX. Pregnancy after abdominoplasty. Aesthetic Plast Surg. 2002;26(4):284-6. PMID: 12397451 DOI: http://dx.doi.org/10.1007/s00266-002-1487-y
12. Mendes Dde A, Nahas FX, Veiga DF, Mendes FV, Figueiras RG, Gomes HC, et al. Ultrasonography for measuring rectus abdominis diastasis muscles. Acta Cir Bras. 2007;22(3):182-6. DOI: http://dx.doi.org/10.1590/S0102-86502007000300005
13. Elkhatib H, Buddhavarapu SR, Henna H, Kassem W. Abdominal musculoaponeuretic system: magnetic resonance imaging evaluation before and after vertical plication of rectus muscle diastasis in conjunction with lipoabdominoplasty. Plast Reconstr Surg. 2011;128(6):733e-40e. PMID: 22094774 DOI: http://dx.doi.org/10.1097/PRS.0b013e318230c8a1
14. al-Qattan MM. Abdominoplasty in multiparous women with severe musculoaponeurotic laxity. Br J Plast Surg. 1997;50(6):450-5. DOI: http://dx.doi.org/10.1016/S0007-1226(97)90333-7
15. Tadiparthi S, Shokrollahi K, Doyle GS, Fahmy FS. Rectus sheath plication in abdominoplasty: assessment of its longevity and a review of the literature. J Plast Reconstr Aesthet Surg. 2012;65(3):328-32. PMID: 22015165 DOI: http://dx.doi.org/10.1016/j.bjps.2011.09.024
16. Pitanguy I. Abdominal plastic surgery. Hospital (Rio J). 1967;71(6):1541-56.
17. Nahas FX, Ferreira LM, Mendes Jde A. An efficient way to correct recurrent rectus diastasis. Aesthetic Plast Surg. 2004;28(4):189-96. DOI: http://dx.doi.org/10.1007/s00266-003-0097-7
18. Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA. The normal width of the línea alba in nulliparous women. Clin Anat. 2009;22(6):706-11. DOI: http://dx.doi.org/10.1002/ca.20836
19. Rohrich RJ, Rios JL. Venous thromboembolism in cosmetic plastic surgery: maximizing patient safety. Plast Reconstr Surg. 2003;112(3):871-2. PMID: 12960870 DOI: http://dx.doi.org/10.1097/01.PRS.0000067916.54634.43
20. Huang GJ, Bajaj AK, Gupta S, Petersen F, Miles DA. Increased intraabdominal pressure in abdominoplasty: delineation of risk factors. Plast Reconstr Surg. 2007;119(4):1319-25. PMID: 17496607 DOI: http://dx.doi.org/10.1097/01.prs.0000254529.51696.43
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade Federal de São Paulo,São Paulo, SP, Brazil
Institution: Private Clinic.
Corresponding author:
Luiz José Muaccad Gama
Rua Alameda dos Nhambiquaras, 156, Indianópolis
São Paulo, SP, Brazil Zip code 04090-000
E-mail: luiz.gama@cmgama.com.br
Article received: July 30, 2013.
Article accepted: April 2, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter