

Original Article - Year 2015 - Volume 30 -
Auto skin expansion in delayed breast reconstruction using flaps without expander: a new concept
Auto-expansão da pele em reconstrução mamária tardia com retalhos sem expansor: um novo conceito
ABSTRACT
INTRODUCTION: The purpose of this study was to share the authors 10 year experience with a new concept in autologous delayed breast reconstruction using deepithelialized pedicled flaps in order to achieve tissue expansion without the use of allogenic expanders.
METHODS: A retrospective analysis of all the patients who underwent deepithelialized thoracodorsal flap (a combination of a musculocutaneous LD with a thoracic fasciocutaneous extension), deepithelialized latissimus dorsi flap or deepithelialized TRAM flap reconstruction between 1999 and 2009 was performed. All the flaps were buried under the mastectomy skin and no skin paddles were used in any of the cases.
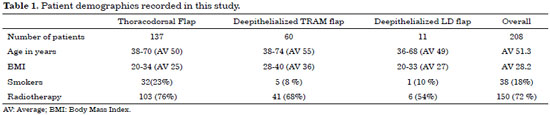
RESULTS: A total of 208 patients including 137 thoracodorsal, 60 TRAM and 11 deepithelialized Latissimus dorsi flaps were performed by the senior surgeon. The average operative time was 90 minutes, 120 minutes and 140 minutes for the deepithelialized Latissimus dorsi, thoracodorsal and TRAM flaps respectively. The mean follow-up period was 4 years, ranging from 1 to 10 years. Although no complete flap loss was reported, fat necrosis was found in 12 % of TRAM flaps. Tissue expansion without the need of allogenic expanders or implants was achieved in all the patients; expansion under the non irradiated breast occurred over the 3 months following reconstruction, where as that under irradiated breasts occurred gradually over the 5 months following reconstruction. The average breast size obtained was cup C. Secondary procedures included lipofilling (20%), contralateral breast remodeling was done in 93% of the cases.
CONCLUSION: In selected cases, tissue expansion of mastectomy skin can be solely achieved by autologous tissue without the need to skin expanders. This method provides a new concept in autologous breast reconstruction circumventing the use of prosthetic material.
Keywords: Latissimus dorsi flap; Breast reconstruction; Transplantation autologous; Tissue expansion.
RESUMO
INTRODUÇÃO: O objetivo deste estudo foi de compartilhar experiência de 10 anos com um novo conceito para reconstrução mamária autóloga utilizando retalhos desepitelizados pediculados para obter expansão de tecido sem o uso de expansores alogênicos.
METÓDOS: Estudo retrospectivo de pacientes submetidos a reconstrução com retalho toracodorsal desepitelizado (uma combinação de musculocutâneo de latíssimo do dorso com extensão facio cutânea torácica), retalho latíssimo do dorso desepitelizado ou retalho TRAM desepitelizado. Todos os retalhos foram acomodados sob a pele onde foi realizada a mastectomia, não foram utilizadas placas de pele em nenhum dos casos.
RESULTADOS: O total de 208 pacientes incluindo 137 retalhos toracodorsal, 60 retalhos TRAM e 11 retalhos latíssimo do dorso desepitelizado foram utilizados pelo cirurgião sênior. O tempo médio da cirurgia foi de 90 minutos, 120 minutos e 140 minutos para retalhos latíssimo do dorso desepitelizados, toracodorsal, e TRAM, respectivamente. A média de seguimento foi de 4 anos, variando de 1 a 10 anos. Apesar de perda completo de retalho não ter sido relatada, a necrose gordurosa foi encontrado em 12% dos retalhos de TRAM. A expansão de tecido sem a necessidade de expansor alôgenico ou implantes foi obtido em todos os pacientes; a expansão sob a mama não irradiada ocorreu em 3 meses seguido da reconstrução, enquanto a expansão sob a mama irradiada ocorreu gradualmente ao longo de 5 meses após a reconstrução. A média do tamanho da mama obtida foi o molde C. Secundário aos procedimentos incluindo a lipofilling (20%), a remodelagem da mama contralateral foi necessária em 93% dos casos.
CONCLUSÃO: Nos casos selecionados, a expansão do tecido da pele onde foi realizada mastectomia pode ser obtida somente com uso de tecido autólogo sem a necessidade de expansores de pele. O método disponibiliza um novo conceito em reconstrução de mama autóloga evitando assim o uso de material prostético.
Palavras-chave: Retalho latíssimo do dorso; Mamoplastia; Transplante autólogo; Expansão de tecido.
The myriad of reconstructive procedures available for breast reconstruction coupled with fast evolution in the field render breast reconstruction a true challenge for plastic surgeons. Patients presenting for delayed breast reconstruction lack the pliability of the native skin envelope over the breast as well as the delineation of the natural infra-mammary fold1. Following radiotherapy, skin expansion becomes even more restricted2-4.
Several treatment modalities have evolved over the past three decades to try to overcome these challenges. The use of allogenic expanders in the form of implants5-8 or other types in order to achieve desired breast volumes coupled with tissue expansion has solved many problems, yet created new challenges9-12. These challenges sparked interest in improving autologous flaps3,9,13-17 in an attempt to avoid using expanders, optimize surgical outcome, and reduce morbidities. The tradeoff was the patch effect over the reconstructed breast.
In this perspective we have described a new concept in delayed autologous breast reconstruction using pedicled deepithelialized thoracodorsal (TD), latissimus dorsi (LD) and TRAM flaps to achieve breast skin expansion without the need for allogenic expanders while avoiding the patch effect over the reconstructed breast.
OBJECTIVE
The purpose of this article is to share our 10 years of experience with a new concept using deepithelialized pedicled flaps in order to achieve gradual skin expansion in delayed breast reconstruction. The limitations and different complications are analyzed as well.
METHODS
We performed a retrospective review of the files on all the patients who underwent deepithelialized TD flap (a combination of a musculocutaneous LD with a thoracic fasciocutaneous extension)18, deepithelialized LD flap, or deepithelialized TRAM flap reconstruction between 1999 and 2009. Parameters of interest included age, BMI, and smoking, as well as radiation and chemotherapy history, breast size, flap dimensions, extent of tissue expansion over the reconstructed breast, operative time, hospital stay, and the different complications. The main indications for surgery included patient refusal of breast expanders and their preference for one of the three mentioned treatment modalities. The patient population comprised those who underwent unilateral or bilateral delayed reconstruction, with or without adjuvant radiotherapy. The deepithelialized LD flap was indicated for patients with originally small breasts, whereas TD flaps and deepithelialized TRAM flaps were indicated for patients with larger breasts. Comparable volumes were achieved following the use of the latter two flaps. Exclusion criteria included all patients with primary reconstruction or partial mastectomy, as well as those who had previously undergone expansion, namely with prosthetic implants or Becker expanders.
The adopted flap designs were as described in the literature for the TRAM and LD flaps; for the TD, it was designed as described by Abboud et al.18. All the surgeries were performed by the same senior surgeon (MA). Access to the breast tissues is permitted through donor incisions at the posterior and mid-axillary lines without invading the breast skin or the mastectomy scar, for the deepithelialized LD and TD flap cases. For the TRAM flap cases, the mastectomy scar is partially incised in order to perform the breast pocket dissection. Following the creation of a pocket under the breast skin, the deepithelialized flaps were transposed and buried under the recipient site. The pocket where the flap will be inset is made tight enough to accommodate the flap, enabling the latter to push on the breast skin and promote tissue expansion. No skin paddles were used in any of the cases. The donor and recipient sites are closed primarily by approximation of deep tissues and skin using absorbable sutures; drains are placed at the recipient and donor sites. The patients were followed closely for the first 6 months following the surgery, then at 6 month intervals. Data were integrated and analyzed in a computerized database (Figure 1A, B, C); (Figure 2A, B, C, D); (Figure 3A, B, C, D); (Figure 4A, B, C, D).
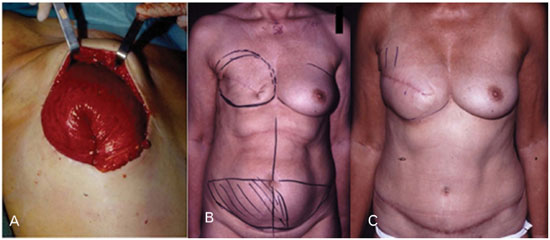
Figure 1. (A) Intraoperative picture showing how the flap is deepithelialized, lumped together, and buried under the recipient skin. Lumping of the flap gives a shape and volume similar to a breast implant and causes tissue expansion by progressively pushing the overlying skin. (B) Preoperative picture before breast reconstruction showing the flat right breast and the preoperative markings. (C) Tissue expansion of the right breast in the same patient at three months post-op.
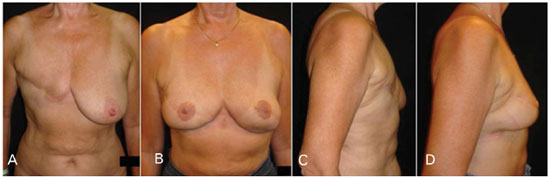
Figure 2. Case of bilateral TD flap reconstruction, right delayed following radiotherapy, and left immediate. (A) and (C) Preoperative pictures. (B) and (D) Postoperative pictures at 4 year follow-up. The auto skin expansion that occurs achieves a projected natural breast, coupled with an improvement in the skin quality. Similar breast shapes were achieved using the same flap for immediate and delayed reconstruction on the same patient.

Figure 3. Case of delayed right deepithelialized TRAM flap reconstruction in an irradiated breast, coupled with contralateral mastopexy. (A), (C) Preoperative pictures. (B), (D) Postoperative pictures at 5 year follow-up showing the extent of breast skin expansion without the need for expanders, coupled with improved skin quality.
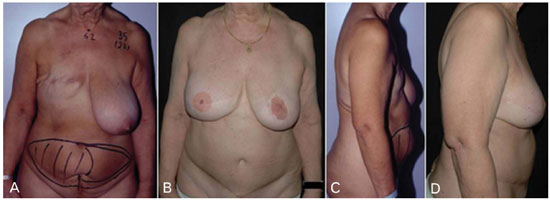
Figure 4. Case of delayed right deepithelialized TRAM flap reconstruction in an irradiated breast, coupled with contralateral mastopexy. (A), (C) Preoperative pictures. (B), (D) Postoperative pictures at 6 year follow-up showing the extent of breast skin expansion and the natural look of the breast.
RESULTS
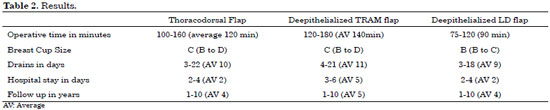
A total of 208 patients who underwent 137 TD, 60 TRAM and 11 LD flap procedures were included in the study. The age groups ranged from 36 to 74 years, and the BMI varied from 20 to 40. Thirty-eight patients were smokers (Table 1). The average operative time was 90 minutes, 120 minutes, and 140 minutes for the deepithelialized latissimus dorsi, thoracodorsal, and TRAM flaps, respectively. The mean follow-up period was 4 years for the LD and TD flap groups compared to 5 years for the TRAM group, ranging from 1 to 10 years. The average hospital stay was 5 days for the TRAM patients and 2 days for both the TD flap and LD flap groups (Table 2). Expansion of mastectomy skin was achieved in all the patients; expansion under the non-irradiated breast skin occurred on average over the 3 months following reconstruction, while under the irradiated breast this process gradually occurred on average over the 5 months following reconstruction. Improvement in the quality of the skin, mainly following radiotherapy, was observed.
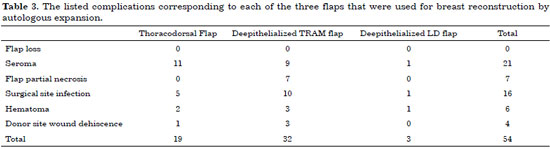
The final breast cup was estimated by the patient's bra cup size. An average C cup was obtained for the TD and TRAM flaps, and B for the LD flap. Secondary procedures included lipofilling (20%) and remodeling of the contralateral breast (93%), 43% of which was comprised of mastopexy. The total complication rate was 25% in this series. No complete flap losses were reported; on the other hand, 12% fat necrosis was recorded for the TRAM flap group. The seroma rate was 10% after all the drains had been removed. Drains were kept in place for an average of 7 days, ranging from 4 to 16 days. The rest of the complications included 16 surgical site infections, 6 hematomas, and 4 cases of dehiscence at the donor site (Table 3).
DISCUSSION
Despite the different established techniques and surgical modalities described in delayed breast reconstruction, major limitations persist, and include the patchy look as well as the need for expanders in order to obtain the required skin expansion over the reconstructed breast2,5,6,7,19. The technique we describe unravels these challenges in delayed breast reconstruction.
It has been shown that reconstruction using autologous tissue improves tissue quality20. We believe that the rich blood supply provided by autologous flaps improves tissue quality, enabling gradual skin expansion over the reconstructed breast. In addition, the bulk of the tissue granted by the TD and TRAM flaps replicates the volume brought by allogenic implants, circumventing the use of the latter to achieve the necessary breast tissue expansion.
In this series, tissue expansion occurred gradually following the surgery, comparable to expansion using allogenic expanders7,8,21-23. Tissue expansion without the need for allogenic expanders or implants was achieved in all the patients; expansion under the non-irradiated breast occurred over the 3 months following reconstruction, while under the irradiated breast this process took place gradually over the 5 months following reconstruction. Expansion occurring spontaneously, as described in this article, presents an advantage over established techniques in the literature, in which serial visits for expander injections as well as high patient compliance are expected8,21,23. This tenuous task is avoided for both patient and physician.
In this series, it was observed that the extent of breast tissue expansion correlated with the volume of the flap, and was coupled with improvement in skin quality which manifested by softening of the breast skin flap, mainly that of irradiated breast.
Sparing the patch effect over the reconstructed breast by adopting the principle of deepithelialized buried flaps was based on the premise that in mastectomy, the best skin for reconstruction is that of the breast itself24. Moreover, burial of the deepithelialized autologous flaps under the recipient skin insures a harmony of the breast in terms of shape and color25,26. Delay described the thoracoabdominal advancement flap coupled to the LD in order to avoid the patch effect over the reconstructed breast. This was followed by another publication in which additional fat surrounding the LD muscle was harvested to obtain larger breast volume.
Quantification of the expanded skin was estimated to be equivalent to the ellipse formed by the incision over the recipient site before in-sitting the flap in the TRAM group. Closure of the recipient wound under moderate tension was well tolerated, owing to the robust blood supply provided by the pedicled flaps25,26.
The reconstructed breast takes its final shape after augmentation with implants; this dictated remodeling of the contralateral breast, when necessary, in order to obtain bilateral breast symmetry, reflected in the 93 % remodeling rate for the contralateral breast in this series. Lipofilling of the reconstructed breast, in addition to the contralateral breast in selected cases, was performed at the time of the reconstruction of the nipple areola complex for 21 patients. Variable volumes ranging from 50 to 300 ml, with an average of 220 ml, were added depending on the volume of the contralateral breast in order to achieve breast symmetry. Overfilling of the reconstructed breast compared to the normal breast was performed, knowing that part of the injected fat volume would be absorbed. Lipofilling served as a complementary modality to achieve further tissue expansion and larger breast volumes, as well as improvement of the skin quality over the reconstructed breast.
Besides an 11.5% rate of partial flap fat necrosis in the TRAM flap group, there were no reported total flap losses in this series. In addition, the lower recorded operative time for the three groups (2 hours, 2 hours 20 minutes, and 1 hour 30 minutes for the TRAM, TD and LD flaps respectively) diminishes pre-operative as well as postoperative complications27. This offers a breadth of surgical options for the plastic surgeon confronting the different challenges of breast reconstruction.
The low seroma rate in this series could be explained by the fact that seroma was recorded after removal of the drains, when the drainage amount was less than 20 CC per day. Therefore, the seroma rate in this report cannot be compared to the numbers in the literature.
Contraindications to the presented technique in our experience involve patients with considerable breast skin damage from radiotherapy. In such cases, it would be preferable for the damaged skin to be excised and replaced with an autologous paddled flap. Other contraindications include previous surgeries, such as thoracotomy at the side of the reconstruction, or major prior abdominal surgery which would hamper use of either the latissimus dorsi muscle or the TRAM flaps.
Besides being a retrospective study, limitations of this article include crude estimation of the achieved breast volumes by looking at cup sizes. Moreover, very large breast volumes cannot be achieved with this surgical technique, so implants or fat grafting are required in a subsequent, complementary procedure for patients who desire larger breast volumes. Another challenge is found in patients with contralateral ptotic breasts, who refuse remodeling of the latter in order to achieve symmetry of both breasts.
CONCLUSION
In selected cases, tissue expansion of mastectomy skin can be solely achieved with autologous tissue without the need for skin expanders. This method provides a new concept in autologous breast reconstruction circumventing the use of prosthetic material. The main advantages of this technique include avoiding the patchy look of skin paddles, improved skin quality (mainly following radiotherapy), and achieving considerable tissue expansion that gradually occurs following the surgery. However, this new concept merits further investigations to unravel the physiology behind tissue expansion using autologous flaps without the need for allogenic expanders, proper quantification of the extent of tissue expansion, as well as the changes brought by the pedicled deepithelialized flaps to the skin and soft tissues of the reconstructed breast, namely following radiation therapy.
REFERENCES
1. Disa JJ, McCarthy CM, Mehrara BJ, Pusic AL, Hu QY, Cordeiro PG. Postmastectomy reconstruction: an approach to patient selection. Plast Reconstr Surg. 2009;124(1):43-52.
2. Tran NV, Evans GR, Kroll SS, Baldwin BJ, Miller MJ, Reece GP, et al. Postoperative adjuvant irradiation: effects on tranverse rectus abdominis muscle flap breast reconstruction. Plast Reconstr Surg. 2000;106(2):313-7.
3. Sigurdson L, Lalonde DH. MOC-PSSM CME article: Breast reconstruction. Plast Reconstr Surg. 2008;121(1 Suppl):1-12.
4. Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg. 2004;114(4):950-60.
5. Becker H. The expander mammary implant for breast reconstruction. In: Nordström REA, ed. Tissue Expansion. Boston: Butterworth-Heinemann; 1996.
6. Cohen BE, Casso D, Whetstone M. Analysis of risks and aesthetics in a consecutive series of tissue expansion breast reconstructions. Plast Reconstr Surg. 1992;89(5):840-3.
7. Wickman M. Rapid versus slow tissue expansion for breast reconstruction: a three-year follow-up. Plast Reconstr Surg. 1995;95(4):712-8.
8. Becker H. Expansion augmentation. Clin Plast Surg. 1988;15(4):587-93.
9. Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg. 2003;112(2):467-76.
10. Forman DL, Chiu J, Restifo RJ, Ward BA, Haffty B, Ariyan S. Breast reconstruction in previously irradiated patients using tissue expanders and implants: a potentially unfavorable result. Ann Plast Surg. 1998;40(4):360-3.
11. Lipa JE, Qiu W, Huang N, Alman BA, Pang CY. Pathogenesis of radiation-induced capsular contracture in tissue expander and implant breast reconstruction. Plast Reconstr Surg. 2010;125(2):437-45.
12. Dickson MG, Sharpe DT. The complications of tissue expansion in breast reconstruction: a review of 75 cases. Br J Plast Surg. 1987;40(6):629-35.
13. Kraemer O, Andersen M, Siim E. Breast reconstruction and tissue expansion in irradiated versus not irradiated women after mastectomy. Scand J Plast Reconstr Surg Hand Surg. 1996;30(3):201-6.
14. Bostwick J 3rd, Jones G. Why I choose autogenous tissue in breast reconstruction. Clin Plast Surg. 1994;21(2):165-75.
15. Delay E. Reconstruction mammaires autologues. In: Dauplat J, Dauce JP, eds. Cancer du sein. Paris: Monographie de l'Association Francaise de Chirurgie; 1995. p.63-94.
16. Elliott LF. Options for donor sites for autogenous tissue breast reconstruction. Clin Plast Surg. 1994;21(2):177-89.
17. Kroll SS. An overview of postmastectomy breast reconstruction. In: Kroll SS, ed. Reconstructive plastic surgery for cancer. St. Louis: CV Mosby; 1996. p.273.
18. Abboud MA, Dibo SA. The deepithelialized Thoracodorsal Flap, a New Concept For Autologous Breast Reconstruction. Abstract at 22nd Annual EURAPS Meeting in 2011, and poster at the16th Congress of the IPRAS in 2011.
19. Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg. 2006;118(4):825-31.
20. Mimoun M, Chaouat M, Lalanne B, Smarrito S. Latissimus dorsi muscle flap and tissue expansion for breast reconstruction. Ann Plast Surg. 2006;57(6):597-601.
21. Pusic AL, Cordeiro PG. An accelerated approach to tissue expansion for breast reconstruction: experience with intraoperative and rapid postoperative expansion in 370 reconstructions. Plast Reconstr Surg. 2003;111(6):1871-5.
22. Collis N, Sharpe DT. Breast reconstruction by tissue expansion. A retrospective technical review of 197 two-stage delayed reconstructions following mastectomy for malignant breast disease in 189 patients. Br J Plast Surg. 2000;53(1):37-41.
23. Khouri RK, Schlenz I, Murphy BJ, Baker TJ. Nonsurgical breast enlargement using an external soft-tissue expansion system. Plast Reconstr Surg. 2000;105(7):2500-12.
24. Delay E, Bremond A. Mastectomie avec conservation de l'étui cutané: concept, problèmes, indications. In: Namer M, Teissier E, Ferrero JM, eds. Les traitements médicaux des cancers du sein. Paris: Arnette Blackwell; 1996. p.309.
25. Delay E, Gounot N, Bouillot A, Zlatoff P, Rivoire M. Autologous latissimus breast reconstruction: a 3-year clinical experience with 100 patients. Plast Reconstr Surg. 1998;102(5):1461-78.
26. Delay E, Jorquera F, Pasi P, Gratadour AC. Autologous latissimus breast reconstruction in association with the abdominal advancement flap: a new refinement in breast reconstruction. Ann Plast Surg. 1999;42(1):67-75.
27. Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9-16.
1. Hospital Center University De Tivoli, La Louviere, Belgium
2. American University of Beirut Medical Center, Beirut, Lebanon
Institution: Hospital CHU Tivoli, La Louviere, Belgium.
Corresponding author:
Dibo Saad
23 avenue penelope
Bruxelas, Bélgica Zip code 04551-060
E-mail: saaddibo@gmail.com
Article received: May 13, 2015.
Article accepted: May 26, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter