

Case Report - Year 2015 - Volume 30 - Issue 1
Aplasia cutis congenita on the lower limbs: a case report
Aplasia congênita da cútis em membros inferiores: relato de caso
ABSTRACT
INTRODUCTION Aplasia cutis congenita (ACC) is a rare disease characterized by the absence of a part of the skin at birth that may be either localized or widespread. The incidence of this disease is 0.1 per 100,000 births. It mainly involves the scalp alone in 60% of the cases. The causes are unclear; however, genetic factors, teratogens (alcohol, cocaine, marijuana, heroin, misoprostol, methimazole, carbimazole, congenital herpes simplex, congenital varicella, and others), impaired blood supply to the skin, trauma, and amniotic band and chromosomal disorders (trisomy 13) are associated with the wounds.
CASE REPORT: A female patient was delivered vaginally at 36 weeks 3 days of gestation, with appropriate weight for the gestational age. She was referred to our service after 7 days of birth, presenting total absence of skin integument on both legs, with impairment of approximately 17% of the body surface according to the Lund and Browder chart. The malformation consisted of the total absence of skin and subcutaneous tissue. Given the extent and localization of the wound, treatment with a partial skin graft was elected, thereby filling the totality of the defect.
CONCLUSION: Owing to the rarity of ACC and the small number of patients in the series published in the literature, standardization of treatment is still incipient. Currently, only recommendations are available. Further studies are needed in order to investigate the etiology of the disease and to evaluate treatment methods.
Keywords: Aplasia cutis congenital; Lower limbs; Malformation; Treatment.
RESUMO
INTRODUÇÃO A Aplasia Congênita da Cútis (ACC) é uma doença rara caracterizada pela ausência de uma parte da pele ao nascimento, seja em área localizada ou generalizada. A incidência é de 0,1 a cada 100.000 nascimentos, tendo como acometimento principal o couro cabeludo, ocorrendo de forma isolada nesta localização em 60% dos casos. As causas não são claras, mas fatores genéticos, teratógenos (álcool, cocaína, maconha, heroína, misoprostol, metimazol, carbimazol, herpes simples congênito, varicela congênita, etc.), comprometimento da irrigação sanguínea para a pele, trauma, bandas amnióticas e desordens cromossômicas (trissomia do 13) estão associados com as lesões.
RELATO DO CASO: Paciente do sexo feminino, nascida de parto vaginal com 36 semanas e três dias, e peso adequado para a idade gestacional. Referenciada ao nosso serviço após sete dias de nascimento, constando ausência total do tegumento cutâneo em ambas as pernas, com acometimento de aproximadamente 17% da superfície corpórea, segundo a tabela de queimados de Lund e Browder. A má formação consistia na ausência total de pele e tecido celular subcutâneo. Face a extensão e localização da lesão, optou-se pelo tratamento por enxerto de pele parcial, permitindo, dessa forma, preencher a totalidade do defeito.
CONCLUSÃO: Devido à raridade da ACC e ao pequeno número de pacientes nas séries publicadas na literatura, a padronização do tratamento ainda é incipiente e o que existe são recomendações. Ainda são necessários estudos que abordem desde a etiologia da doença até a avaliação dos métodos de tratamento.
Palavras-chave: Aplasia congênita da cútis; Membros inferiores; Má formação; Tratamento.
Aplasia Cutis Congenita (ACC) is a rare disease characterized by the absence of a part of the skin at birth, either localized or widespread. It usually occurs on the midline of the scalp and is presented at birth as an ulcerated wound reaching different depths1,2.
In 75% of patients, ACC occurs as a single wound1. The wounds are not inflammatory, are well defined, and extend from 0.5 to 10 cm or more. The skin defects that are formed early in pregnancy may heal before delivery, and appear as an atrophic, membranous, or parchment-like scar, with associated alopecia. Meanwhile, less mature defects are presented as ulcerations.
The reported incidence is 0.1 per 100,000 births3. The causes are unclear; however, genetic factors, teratogens (alcohol, cocaine, marijuana, heroin, misoprostol, methimazole, carbimazole, congenital herpes simplex, congenital varicella, and others), impaired blood supply to the skin, trauma, amniotic bands, and chromosomal disorders (trisomy 13) are associated with the wounds4.
The aim of this study is to report the rare case of a patient with ACC strictly localized on the lower limbs, treated with a partial skin graft.
CASE REPORT
A female patient was delivered vaginally at 36 weeks 3 days, with an Apgar score of 9/10 and appropriate weight for gestational age. In the anamnesis, family antecedents of congenital skin diseases were not found, and the parents were not consanguineous. The mother was 18 years old. This was her second pregnancy, and her eldest daughter was healthy. The mother discovered the pregnancy at approximately 20 weeks of gestational age, when she was still irregularly taking oral contraceptives (Levonorgestrel + Ethinyl estradiol). She initiated prenatal and ultrasonographic examinations at 27 weeks of gestational age. No changes were evident during the examinations.
The patient was referred to our service after 7 days of birth, presenting total absence of skin integument on the anteromedial face of both legs, preserving an island of skin on the posterior and plantar regions, with impairment of approximately 17% of the body surface according to the Lund and Browder chart. The malformation consisted of total absence of skin and subcutaneous tissue. The patient presented eumorphic facies, flat hemangioma in the bilateral eyelid, and incomplete cleft palate. The wound was present on the lower limbs, appearing like ulcerations with irregular delimited borders, involving part of the legs and feet bilaterally (Figure 1).

Figure 1. Patient with 11 days of life. Aplasia cutis congenita with extensive involvement of legs (anterior and medial walls), with full impairment of the skin and the subcutaneous tissue.
During hospitalization, serological tests for infectious diseases such as herpes and varicella were requested, as well as skin biopsy and karyotyping for exclusion of chromosomal disorders. Transfontanellar and abdominal ultrasonography, as well as echocardiography, were also performed. In the examinations, only patent ductus arteriosus 2.5-mm long with discrete hemodynamic repercussion was identified. The radiograph of the long bones did not show any malformation. Evaluation by a geneticist did not detect any other malformations. Thus, a syndromic picture could not be defined; only a picture of isolated ACC was observed.
Given the extent and localization of the wound, we opted for treatment with a skin graft on the 11th day of the patient's life. A partial skin graft was applied, removed from both thighs and used to fill the totality of the defect. The dressing performed on the fifth postoperative day showed good integration of the skin graft on nearly all the grafted areas. The patient was discharged to outpatient follow-up on the 16th postoperative day, presenting a good evolution of the wound (Figure 2).

Figure 2. Patient on the 16th postoperative day.
DISCUSSION
ACC is a rare disease that is clinically diagnosed according to the physical finding of absence of skin at birth. It is most commonly manifested as focal wounds affecting the scalp. The histological aspect of the wound varies from partial absence of skin, transitioning to its total absence; impairment of subcutaneous tissue, fascia, and muscles; and finally, impairment of bone and dura mater5. More rarely, it affects other areas of the body, including the trunk and limbs, as it widely spreads to large areas.
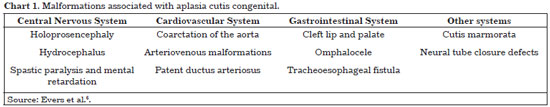
ACC is usually manifested as an isolated malformation, such as the case in our patient. However, several associated single or multiple malformations that affect the most diverse organ systems have been described (Chart 1)6.
According to statistical data7, of the overall ACC cases, 25% involve impairment of the lower limbs, 12% involve the trunk and flanks, and 60% involve impairment of the scalp.
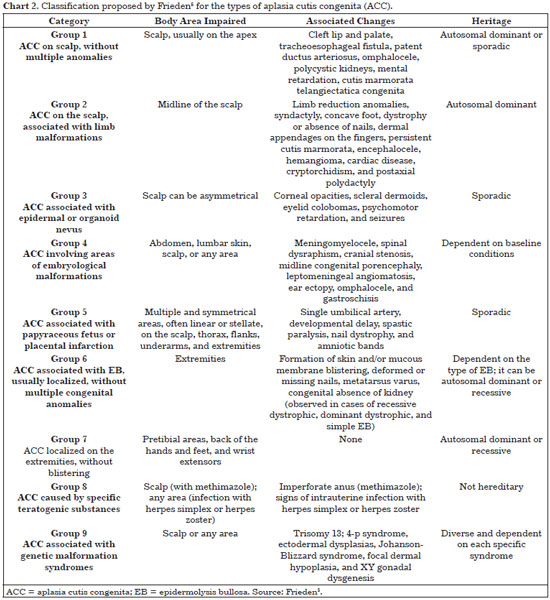
In 1986, Frieden5 performed an extensive survey of subjects and proposed a classification based on the patterns of presentation of the skin wound, the presence and type of associated malformations, and transmission mode (Chart 2). The researcher subdivided the patients into nine groups. The patient under analysis in this study seems to fit in group 7 of Frieden's classification, that is, "ACC localized on the extremities, without blistering," based on clinical findings that coincide with the occurrence pattern of the patient's skin wound (ACC involving pretibial areas, the back of the hands and feet, and wrist extensors; Table 2). Involvement of the upper limbs, however, was not observed.
Owing to the large extent of the wound, it resembled third-degree burns. The first concern of the medical team was safeguarding the patient from water, electrolyte and caloric losses, and the risk of infection while waiting for the best clinical conditions before administering the definitive surgical treatment. Therefore, the patient was under the care of the pediatrics and plastic surgery team for hydration maintenance and infection control, through local care and antibiotic therapy.
Several treatment options presented by different authors5,7,8 are available, depending on the type and extent of the wound. Small wounds affecting only the skin and subcutaneous tissue are left to healing by secondary intention, which occurs fast. In many reports, patients present at birth with small scars on the scalp, featuring an aplasia appearance, with intrauterine healing. For larger wounds, especially those affecting deeper tissues and when vital organs are exposed, treatment with local flaps would be indicated. In cases with extensive wounds, as in the present case, the use of a skin graft seems the only solution. Most of the similar cases described in the literature were treated by using the same method, with complete wound closure.
The importance of this report relies in describing another case for publication in the literature as a relevant rare condition, which is even rarer when its extension, pattern of involvement, and secondary changes are considered.
CONCLUSION
Owing to the rarity of the ACC and the small number of patients in the series published in the literature, standardization of the treatment is still incipient. Currently, only recommendations are available. Further studies are needed in order to investigate the etiology of the disease and to evaluate the treatment methods, as well as the clinical evolution in larger groups of patients.
REFERENCES
1. Moscona R, Berger J, Govrin J. Large skull defect in aplasia cutis congenita treated by pericranial flap: long-term follow-up. Ann Plast Surg. 1991;26(2):178-82. http://dx.doi.org/10.1097/00000637-199102000-00012. PMid:2006845.
2. Yang JY, Yang WG. Large scalp and skull defect in aplasia cutis congenita. Br J Plast Surg. 2000;53(7):619-22. http://dx.doi.org/10.1054/bjps.2000.3413. PMid:11000081.
3. Bajpai M, Pal K. Aplasia cutis cerebri with partial acrania--total reconstruction in a severe case and review of the literature. J Pediatr Surg. 2003;38(2):e4. http://dx.doi.org/10.1053/jpsu.2003.50064. PMid:12596124.
4. Suárez O, López-Gutiérrez JC, Andrés A, Barrena S, Encinas JL, Luis A, et al. [Aplasia cutis congenita: surgical treatment and results in 36 cases]. Cir Pediatr. 2007;20(3):151-5. PMid:18018742.
5. Frieden IJ. Aplasia cutis congenita: a clinical review and proposal for classification. J Am Acad Dermatol. 1986;14(4):646-60. http://dx.doi.org/10.1016/S0190-9622(86)70082-0. PMid:3514708.
6. Evers MEJW, Steijlen PM, Hamel BC. Aplasia cutis congenita and associated disorders: an update. Clin Genet. 1995;47(6):295-301. http://dx.doi.org/10.1111/j.1399-0004.1995.tb03968.x. PMid:7554362.
7. Stringa S, Pellerano G, Bustin Z. Aplasia cutis congênita comentário sobre cinco casos. Med Cut ILA. 1985;13:321-6.
8. Irons GB, Olson RM. Aplasia cutis congenita. Plast Reconstr Surg. 1980;66(2):199-203. http://dx.doi.org/10.1097/00006534-198008000-00003. PMid:6996008.
1. Hospital Santa Casa de Campo Grande, Campo Grande, MS, Brazil
2. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil
3. Hospital Regional de Mato Grosso do Sul, Campo Grande, MS, Brazil
4. Hospital Universitário de Mato Grosso do Sul, Campo Grande, MS, Brazil
Institution: Study performed at the Hospital Santa Casa de Campo Grande, MS, Brazil.
Corresponding author:
Gustavo de Sousa Marques Oliveira
Av. Primeiro de Maio, 335 - São Bento
Campo Grande, MS, Brazil Zip Code 79004-620
E-mail: gustavomo49@hotmail.com
Article received: September 19, 2011.
Article accepted: October 16, 2011.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter