

Original Article - Year 2015 - Volume 30 -
Burn Care Unit of São Paulo Federal University: an epidemiological profile
Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo: estudo epidemiológico
ABSTRACT
INTRODUCTION: Burns constitute severe trauma and account for 100,000 hospital visits per year in Brazil. Burns units are essential for the treatment of these patients and the generation of knowledge on this subject.
METHOD: This study established the annual profile of burn unit attendance between 2009 and 2012. During these years of activity, we compared the number of hospitalized patients, patient origin, burn degree, age, burn body surface area, days of hospitalization, types of surgical procedures, agents, and mortality. Possible combinations were evaluated with the chi-square test.
RESULTS: A total of 321 patients were hospitalized. In 2009, 70% of the patients presented secon-degree burns; in 2012, 66% of the patients presented third-degree burns. In 2009, 37% of the patients were referred to other services; in 2012, 72% were referred. The average patient age was 29 years old in 2009 and 44 years old in 2012. Burn body surface was 13% in 2009 and 8% in 2012. Hospitalization time increased from 11 to 21 days. A total of 50 surgical procedures were performed in 2009, while 103 were performed in 2012. Flammable liquids were the most commonly observed causal agents. The overall mortality rate decreased from 7% to 4% over the study period.
CONCLUSION: There was an increase in the number of referred and complex patients with higher degree burns who required longer hospital stays and a greater number of procedures over the years. The decreased mortality rate reflected the technical improvement of the unit that was established as a regional reference for the treatment of burn victims.
Keywords: Burns; Burn unit; Measures in epidemiology.
RESUMO
INTRODUÇÃO: As queimaduras são traumas graves, que geram 100 mil atendimentos hospitalares por ano, no Brasil. As Unidades de Queimados são fundamentais para o tratamento desses pacientes e a produção de conhecimento sobre o tema.
MÉTODO: O estudo estabeleceu o perfil de atendimento em cada ano de funcionamento da unidade no período de 2009 a 2012, e comparou, entre esses anos, a quantidade de pacientes internados, a procedência, os graus de queimadura, a idade, a superfície corporal queimada, os dias de internação, os tipos de procedimentos cirúrgicos, os agentes e a mortalidade. Para avaliação das possíveis associações, foi utilizado o teste do Qui-quadrado.
RESULTADOS: Foram internados 321 pacientes. Em 2009, 70% dos pacientes apresentavam queimadura de II grau e, em 2012, 66% dos pacientes tinham queimadura de III grau. Em 2009, 37% vieram referenciados de outros serviços, e em 2012, 72%. A idade média dos pacientes foi de 29 anos em 2009 e 44 anos, em 2012. A superfície corporal queimada no início era de 13%, e em 2012, foi 8%. O tempo de internação subiu de 11 para 21 dias. Em 2009, realizaram-se 50 procedimentos cirúrgicos. Em 2012, foram 103. O agente causal mais encontrado foram os líquidos inflamáveis e a mortalidade global caiu de 7% para 4%, ao longo dos anos.
CONCLUSÃO: Houve um aumento na quantidade de pacientes referenciados e complexos, com queimaduras de maior grau, exigindo mais procedimentos e maior hospitalização, ao longo dos anos. A taxa de mortalidade diminuiu, refletindo melhora técnica da Unidade, que se estabeleceu como referência regional no tratamento de queimados.
Palavras-chave: Queimaduras; Unidade de queimados; Medidas em epidemiologia.
Burns are severe traumatic wounds whose etiology involves contact of a patient with thermoelectric sources and corrosive substances1. An estimated 6 million victims presenting with some degree of burn seek medical care worldwide each year2. The lack of epidemiological data and national reporting systems makes it almost impossible to classify the specific distribution of cases by country. In some countries, for example, the available data enable the estimation of the annual incidence of burns, which approximately accounts for 500,000 cases in the United States (US)3, 10-15,000 hospitalizations per year in Germany4, and 700-800,000 new cases in India5. In Brazil, it is estimated that the total number of burns per year is approximately 1 million. Of these, only 100,000 victims seek medical care, while approximately 2,500 die of direct or indirect consequences of these burns.6 Still, according to the data of the Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde), this type of disease is responsible for nearly 30,000 hospitalizations per year6, which demonstrates the importance of this issue in public health planning.
Burn Care Units (BCUs) were first established in the US and England in the 1950s with the aims of improving and intensifying the specific treatment of burn victims and improving the epidemiological indices of attendance7. There are currently 137 BTUs throughout the US8. According to the Brazilian Society of Burns (BSB), there are 57 registered BCUs throughout Brazil1. In the municipality of São Paulo, with a population of almost 20 million inhabitants, there are six BCUs in public hospitals accredited by the BSB for an annual local incidence of an estimated 10,000 new cases per year6.
These units are reference centers for the hospitalization and treatment of critical patients presenting with complex second and third degrees burns as well as important comorbidities. These units operate as multidisciplinary treatment centers with dozens of professionals providing care to these patients7,9. In addition to providing clinical care, these units should function as promoter centers of knowledge as well as professionals trainers and disseminators of burn data.
OBJECTIVE
The aim of this study was to use epidemiological information collected from the BCU to establish and compare the profile of attendance by year or activity.
METHODS
The study compared the data of each patient admitted to the BCU of the Hospital São Paulo, Plastic Surgery Service of Paulista Medical School, Federal University of São Paulo, between July 20, 2009 and December 26, 2012. The variables were separately categorized by year and classified as follows: number of patients hospitalized, patient origin, burn degree, age, burn body surface, days of hospitalization, surgical procedures, burn agents, and mortality rate.
Burns were divided into second and third degrees according to a clinical evaluation analyzing the presence of a burn and the superficial areas affected. The presence of a 1% full-thickness burn was enough to include a patient in the third-degree burns group due to the high correlation between this variable and mortality10,11. Patient origin was divided into Spontaneous Arrival (patients who arrived to the unit by themselves without any kind of prior specialized care) and Referred (patients who were initially treated in another service and then transferred to the unit or brought by rescue service after a specialized central office adjusted the available vacancies).
For the variables Age, Burn Body Surface, and Days of Hospitalization, we calculated the simple arithmetic mean of the values obtained by each patient by year of service. The techniques used for the surgical procedures were classified as Debridement, Grafting, Amputations, and Flaps, and the number of times each procedure was performed was recorded for each year evaluated. The Burn Agents considered were Flammable Liquids (liquid alcohol and gel, solvents, and fuels), Special Agents (electrical and chemical burns), Solids (materials with heated surfaces such as stoves, ovens, and industrial sheet metal), Heat/Fire (fires and explosions), and Hot Liquids (oil and water). The mortality rate that was calculated was based on the number of deaths per year. The Burn Degree variable was elected as an independent variable, whereas the others were dependent variables.
All data were obtained from specific tables containing the individual details of each patient that were updated daily between 2009 and 2012 and information was obtained directly from the patients' medical records.
We used the chi-square test to evaluate possible associations. The use of the statistical data was approved by the Research Ethics Committee of the Federal University of São Paulo.
RESULTS
In the evaluated period, 321 patients were admitted to the BCU. Of them, 166 patients presented with partial-thickness burns (second-degree) and 155 patients presented with total thickness burns (third-degree). There were 101 hospitalized patients in 2011; of them, 48 had partial-thickness burns and 53 had total-thickness burns. In 2012, 25 (33%) hospitalized patients had second-degree burns and 50 (67%) had third-degree burns. Over the 4 years, a significant increase in patients with third-degree burns was observed compared to second-degree burns (χ2 test = 21.45/p=0.0001) (Figure 1).
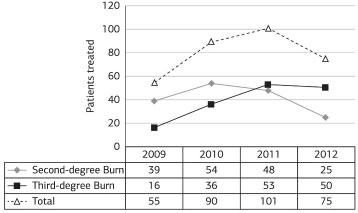
Figure 1. Patients treated per year by burn degree (Q2 = 21.45; p=0.0001).
Regarding patient origin, in 2009, 35 (63%) spontaneously sought medical care and 20 (37%) patients were referred; in 2012, 21 (28%) patients spontaneously sought care and 54 (72%) were referred. Over the 4-year study period, 138 patients were admitted to the service by spontaneous arrival and 183 patients were referred to the BCU, a significant increase (χ2 test = 18.21/p=0.0001) in referred patients (Figure 2).
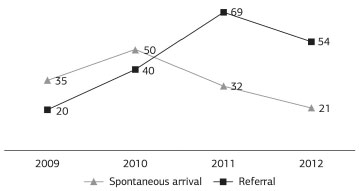
Figure 2. Patient origin (spontaneous arrival versus referral) by year of service (Q2 = 18.21; p=0.0001).
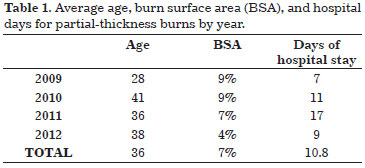
The average age of patients with partial-thickness burns was 36 years in the entire evaluation period. Regarding burn body surface area, the total average was 7% for second-degree burns and only 4% in 2012. Over the 4 evaluated years, the average number of days of hospitalization of patients with partial-thickness burns was 11 (range, 7 in 2009 to 17 in 2011) (Table 1).
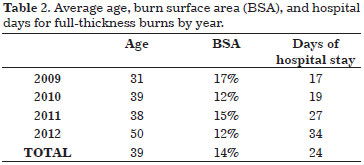
For full-thickness burns, the average patient age was 39 years. In 2009, the average patient age (31 years) was lower, while the highest average age (50 years) was observed in 2012, when the greatest number of patients with third-degree burns was hospitalized. Regarding the number of days that patients with third-degree burns remained in the BCU, the average was 24 (range, 17 in 2009 to 34 in 2012) (Table 2). The average burn body surface that these patients presented during these 4 years was 14% and peaked at 17% in 2009.
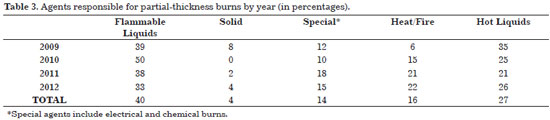
Flammable liquids were most commonly responsible for the partial-thickness burns (mean, 40%), and hot liquids accounted for an average of 27% of these burns. No significant variation in these agents was observed over the study period. Special agents (electrical burns and chemicals) alternated between the third and fourth place in the incidence of accidents caused by heat and fire. A slight predominance of heat/fire (16%) was observed over special agents (14%). For this type of burn, solid agents were the least responsible (4%) (Table 3).
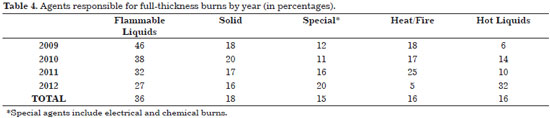
Similarly, flammable liquids were more commonly the causative agents of full-thickness burns (mean, 36% during the study period). Only in 2013 did hot liquids (32%) exceeded flammable agents (27%) in prevalence of causing burns. Unlike partial burns, solid agents achieved the second highest overall average over the years, accounting for 18% of third-degree burns. Hot liquids, heat/fire, and special agents were responsible for 16%, 16%, and 15%, respectively (Table 4).
Regarding the surgical procedures performed on patients suffering from second-degree burns, a total of 114 procedures were performed in the evaluation period, including 59 debridements and 54 grafts. For these patients, the highest number of procedures was performed in 2011, with 21 debridements and 17 grafts (Figure 3).
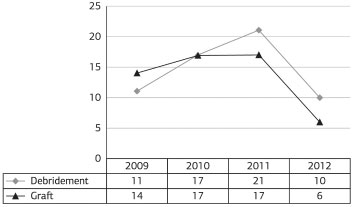
Figure 3. Number of procedures performed per year for seconddegree burns.
Regarding the surgical procedures performed in the full-thickness burn victims, 273 were performed between 2009 and 2012, including 130 debridements, 127 grafts, eight amputations, and eight flaps (Figure 4).
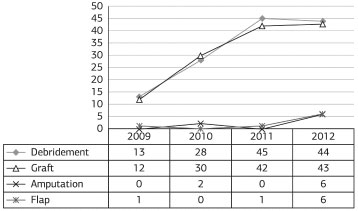
Figure 4. Number of procedures performed per year for thirddegree burns.
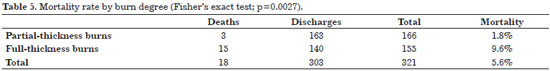
Of the total 321 patients admitted to the unit, 18 died, which corresponds to an overall mortality rate of 5.6% throughout the study period (6% in 2009 and 3% in 2012) for both burn degrees (Figure 5).
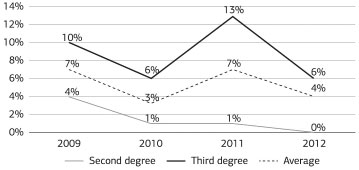
Figure 5. Mortality rate per burn degree by year (in percentage).
Considering burn degree only, a mortality rate of 1.8% was observed for partial-thickness burns, and of 9.6%, for full-thickness burns (Table 5).
DISCUSSION
Most studies on epidemiological data obtained from BCUs in Brazil describe these findings in cross-sectional studies6,12-14. Variables such as gender, age, burn body surface area, flammable agents, and mortality rate, among others, are very common in different services, with publications consistently reporting on the care service profile without investigating the evolution of each unit2,15,16. On the other hand, publications from more developed countries revealed greater heterogeneity; in addition to epidemiological variables, their evolution17, burn-related costs9, and specific treatment strategies7 are considered in addition to transfer criteria and the rational arrangement of BCUs in those countries3,18. This study analyzed the data obtained in an attempt to establish both the profiles of the hospitalized patients and the evolution of the BCU over the years evaluated in a regional and national scenario of burn care.
The unit became active in the second half of 2009, when the number of patients attended and the procedures performed remained low. A total of 321 patients attended in the 4 years evaluated, a number compatible with the data obtained from other BCUs6,16. However, units with higher numbers of beds reported larger samples6,14.
The relative risk for patient referral to reference BCUs is 2.4 for head and neck burns, 1.8 for hand burns, and 1.09 for burns affecting a body surface > 40%18. Patients with these types of injuries represent more complex cases, i.e. with associated lesions and requiring a greater number of surgical procedures and a longer hospital stay. Over the evaluation period, an increased number of patients were referred to our BCU. These patients were more severe and these complex cases contributed to increase the length of hospital stay in the BCU.
The number of surgical procedures that are performed in patients with full-thickness burns demonstrates the complexity of these cases16,18,19. Throughout the 4-year evaluation period, the absolute number of surgical procedures increased by >200%. There was a decrease in the absolute number of surgical procedures in patients presenting with partial-thickness burns, probably due to the ability to make a differential diagnosis between deep and superficial injuries.
The average age of the patients treated at the BCU throughout the study period was 37.5 years, which differs from the national and international literature. A review6 collecting data from >10 Brazilian BCUs published in 2012 reported an age range of 25-30 years. Older patients have more comorbidities that require greater multidisciplinary care18. Compared to 2009, an increase of 44% was observed in the average age of patients admitted in 2012. This may have contributed to the increased length of hospital stay observed in the last year.
Regarding etiologic agents, flammable liquids, mainly represented by alcohol for domestic use, were the main causes of superficial and deep burns. The national literature cites similar data in a comprehensive manner6, while liquid alcohol has been the focus of specific studies14. However, the world literature places heat/fire as a first agent, followed by scalding and injury due to the contact with hot solids2,15,16. Several sociocultural differences explain the variation observed between causative agents in countries with different socioeconomic levels, for example, the high rates of electrical burn in Turkey is due to a poor public lighting system20. In Brazil, liquid alcohol is sold in large plastic containers (500-1,000 mL), which is sufficient to cause large burns.
Regarding the burn surface area (BSA), the averages observed were 7% for partial-thickness burns and 14% for full-thickness burns, which is in agreement with the data reported in the literature6,17. Despite the small average, patients with second-degree burns admitted in a reference unit call attention to the occurrence of lesions in critical areas such as the face, hand, and genitals, as these injuries are the criteria used for the transfer and admission of patients to BCUs who require treatment to minimize possible sequelae.
BSA is the main determinant for the duration of hospital stay: patients with a BSA of 20-35% remained hospitalized for 12-28 days, while those with a BSA >50% may require unit care for >40 days20. On the other hand, patient ages, comorbidities, inhalation injuries, associated traumas, and electrical and chemical burns are important risk factors that not only prolong hospital stays but also determine the transfer to BCUs2,18. The highest incidence of patients transferred and the increased average age, i.e. from 31 to 50 years old, of patients with full-thickness burns in the BCU can be elucidatory factors in the apparent paradox between reduced BSA and increased time of admission observed in the evaluation period. This increased the number of patients with severe burns who sought treatment or were referred to the BCU of the Hospital São Paulo as a regional reference in burn treatment.
Regarding the observed mortality rate, the value of 5.6% for the entire analyzed period is within the standards established in Brazil and worldwide. Compared to countries with the highest Human Development Index (HDI), the mortality rate in this study was slightly higher than the values found in these centers2,18. However, our mortality rate was lower than those of low HDI countries in Europe, Africa, and Southeast Asia15,17. There was also a decrease from 7% to 4% in the overall mortality rate over the 4-year study period, even with the attendance of more severely affected patients with more complex burns, suggesting technical improvements of the staff of our BCU in the treatment of these patients.
The mortality rates of BCUs have been largely related to the social and economic conditions of different countries because the severity of these accidents reflects the educational level of the population, promotion of prevention campaigns, networks of quality electrical distribution, available resources for burns treatment, and many other factors.
CONCLUSION
There was an increase in the number of patients with deep burns who were referred from other services and required longer hospital stays, a higher number of procedures performed over the study period, and a reduced mortality rate.
REFERENCES
1. Sociedade Brasileira de Queimaduras - SBQ. Queimaduras [Internet]. Goiânia [cited 2013 June 16]. Available from: http://sbqueimaduras.org.br/queimaduras-conceito-e-causas.
2. Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14(5):R188. http://dx.doi.org/10.1186/cc9300. PMid:20958968.
3. Klein MB, Kramer CB, Nelson J, Rivara FP, Gibran NS, Concannon T. Geographic access to burn center hospitals. JAMA. 2009;302(16):1774-81. http://dx.doi.org/10.1001/jama.2009.1548. PMid:19861669.
4. Spanholtz TA, Theodorou P, Amini P, Spilker G. Severe burn injuries: acute and long-term treatment. Dtsch Arztebl Int. 2009;106(38):607-13. http://dx.doi.org/10.3238/arztebl.2009.0607. PMid:19890417.
5. Atiyeh B, Masellis A, Conte C. Optimizing burn treatment in developing low- and middle-income countries with limited health care resources (part 1). Ann Burns Fire Disasters. 2009;22(3):121-5. PMid:21991167.
6. Cruz BF, Cordovil PBL, Batista KNM. Perfil epidemiológico de pacientes que sofreram queimaduras no Brasil: revisão de literatura. RevBras Queimaduras. 2012;11(4):246-50.
7. Al-Mousawi AM, Mecott-Rivera GA, Jeschke MG, Herndon DN. Burn teams and burn centers: the importance of a comprehensive team approach to burn care. Clin Plast Surg. 2009;36(4):547-54. http://dx.doi.org/10.1016/j.cps.2009.05.015. PMid:19793550.
8. American Burn Association - ABA. [Internet]. Chicago, EUA [cited 2014 Apr 21]. Available from: http://www.ameriburn.org/BCRDPublic.pdf.
9. Klein MB, Hollingworth W, Rivara FP, Kramer CB, Askay SW, Heimbach DM, et al. Hospital costs associated with pediatric burn injury. J Burn Care Res. 2008;29(4):632-7. http://dx.doi.org/10.1097/BCR.0b013e31817db951. PMid:18535469.
10. Tobiasen J, Hiebert JM, Edlich RF. The abbreviated burn severity index. Ann Emerg Med. 1982;11(5):260-2. http://dx.doi.org/10.1016/S0196-0644(82)80096-6. PMid:7073049.
11. Lionelli GT, Pickus EJ, Beckum OK, Decoursey RL, Korentager RA. A three decade analysis of factors affecting burn mortality in the elderly. Burns. 2005;31(8):958-63. http://dx.doi.org/10.1016/j.burns.2005.06.006. [Review] PMid:16269217.
12. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Estudo epidemiológico da Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo. RevBras Queimaduras. 2010;9(3):82-8.
13. Leão CEG, Andrade ES, Fabrini DS, Oliveira RA, Machado GLB, Gontijo LC. Epidemiologia das queimaduras no estado de Minas Gerais. RevBrasCirPlást. 2011;26(4):573-7.
14. Aldunate JLCB, Ferrari Neto O, Tartare A, Araujo CAL, Silva CC, Menezes MAJ, et al. Análise de 10 anos de casos de queimaduras por álcool com necessidade de internação em hospital quaternário. RevBras Queimaduras. 2012;11(4):220-5.
15. Oladele AO, Olabanji JK. Burns in Nigeria: a review. Ann Burns Fire Disasters. 2010;23(3):120-7. PMid:21991210.
16. Garg R, Gupta A, Pal R, Gupta AK, Uppal S. A clinico-epidemiologic study of 892 patients with burn injuries at a tertiary care hospital in Punjab, India. J Emerg Trauma Shock. 2011;4(1):7-11. http://dx.doi.org/10.4103/0974-2700.76820. PMid:21633560.
17. Engrav LH, Heimbach DM, Rivara FP, Kerr KF, Osler T, Pham TN, et al. Harborview burns--1974 to 2009. PLoS One. 2012;7(7):e40086. http://dx.doi.org/10.1371/journal.pone.0040086. PMid:22792216.
18. Zonies D, Mack C, Kramer B, Rivara F, Klein M. Verified centers, nonverified centers, or other facilities: a national analysis of burn patient treatment location. J Am Coll Surg. 2010;210(3):299-305. http://dx.doi.org/10.1016/j.jamcollsurg.2009.11.008. PMid:20193892.
19. Saaiq M, Zaib S, Ahmad S. Early excision and grafting versus delayed excision and grafting of deep thermal burns up to 40% total body surface area: a comparison of outcome. Ann Burns Fire Disasters. 2012;25(3):143-7. PMid:23467391.
20. Coban YK, Erkiliç A, Analay H. Our 18-month experience at a new burn center in Gaziantep, Turkey. Ulus Travma Acil Cerrahi Derg. 2010;16(4):353-6. PMid:20849054.
1. Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil
2. Unidade de Tratamento de Queimaduras, Departamento de Cirurgia, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil
3. Universidade Santo Amaro (UNISA), São Paulo, SP, Brazil
Institution: Study carried out at Escola Paulista de Medicina da Universidade Federal de São Paulo, SP, Brazil.
Corresponding author:
Lydia Masako Ferreira
Universidade Federal de São Paulo
Rua Napoleão de Barros, 737 - 4th floor - Vila Clementino
São Paulo, SP, Brazil Zip Code 04024-002
E-mail: marta.dcir@gmail.com; ldariofaustino@yahoo.com.br; dra.afo@gmail.com
Article received: July 1, 2014
Article accepted: January 25, 2015


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter