

Original Article - Year 2015 - Volume 30 -
Morphometric study of the latissimus dorsi muscle in human fetuses
Estudo morfométrico do músculo latíssimo do dorso em fetos humanos
ABSTRACT
INTRODUCTION: The latissimus dorsi muscle (LDM) is broad and triangular and performs extension, adduction, and internal rotation motions of the arm. The LDM is vascularized by the thoracodorsal vessels and perforating branches of the posterior intercostal and lumbar arteries and is considered a type V Mathes and Nahai flap that is of great applicability in plastic surgery. The goal of the present study was to analyze the morphometry and vascularization of LDM in human fetuses.
METHOD: The axillary region and the LDM of eight human fetuses (three female, five male) were dissected at 20-32 weeks' gestation in the supine position with full arm abduction. We measured the subscapular and thoracodorsal vessel lengths and conducted a muscle morphometric analysis.
RESULTS: In all fetuses, the thoracodorsal vessels conferred primary vascularization of the LDM. In 25%, the subscapular vein was directly confluent with the axillary vein; 25% of the cases presented with a double scapular circumflex vein. The branch to the serratus anterior muscle was unique in all cases. In 50% of cases, the angular branch of the thoracodorsal artery was visualized, while 25% of them came from the branch to the serratus anterior muscle. The distances between muscle insertion and input of the neurovascular pedicle were 1.1 and 1.9 cm in fetuses 21 and 26 weeks, respectively. The anterior muscle margin was on the mid-axillary line in all fetuses.
CONCLUSION: The observed constant morphometry and reduced anatomical variation of the vascular pedicle enabled the possibility of research involving the use of LDM in intrauterine surgical reconstructions.
Keywords: Latissimus dorsi muscle; Human fetuses; Morphometry.
RESUMO
INTRODUÇÃO O músculo latíssimo do dorso (MLD) é largo, triangular e realiza extensão, adução e rotação medial do braço. É vascularizado pelos vasos toracodorsais e ramos perfurantes das artérias intercostais posteriores e lombares, configurando retalho tipo V de Mathes e Nahai, de grande aplicabilidade em cirurgia plástica. O objetivo é analisar a morfometria e a vascularização do MLD em fetos humanos.
MÉTODO: Dissecou-se a região axilar e o MLD de oito fetos humanos formolizados (três do sexo feminino e cinco do sexo masculino), entre 20 e 32 semanas gestacionais, em decúbito dorsal e abdução completa do braço. Mensuraram-se os comprimentos dos vasos subescapulares e toracodorsais, e foi realizada a morfometria do músculo.
RESULTADOS: Em todos os fetos, os vasos toracodorsais conferiram a vascularização primária do MLD. Em 25%, a veia subescapular era tributária direta da veia axilar; 25% dos casos apresentaram veia circunflexa da escápula dupla. O ramo para o músculo serrátil anterior foi único em todos os casos. Em 50% dos casos, o ramo angular da artéria toracodorsal foi visualizado e, em 25% deles, era proveniente do ramo para o músculo serrátil anterior. A distância entre a inserção do músculo e a entrada do pedículo neurovascular variou entre 1,1 e 1,9 cm em fetos de 21 e 26 semanas, respectivamente. Todos os fetos apresentaram a margem anterior do músculo na linha axilar média.
CONCLUSÃO: A morfometria constante e a reduzida variação anatômica do pedículo vascular encontradas possibilitam a realização de pesquisas envolvendo o uso do MLD em reconstruções cirúrgicas intraútero.
Palavras-chave: Músculo latíssimo do dorso; Fetos humanos; Morfometria.
The latissimus dorsi muscle (LDM) is a large triangular muscle with a proximal fixation in the spinous processes of the thoracolumbar fascia of the lower six thoracic vertebrae, the iliac crest, and the third or fourth lower ribs. In its upper portion, the muscle undergoes a 180º twist to form the tendon that inserts into the intertubercular groove of the humerus1,2. The LDM performs arm extension and adduction and medial arm medial rotation as well as moves the scapular medially and downward2. Its innervation is performed by the thoracodorsal nerve branch of the posterior division of the brachial plexus1.
The LDM is primarily vascularized by the thoracodorsal artery, a terminal branch of the subscapular artery along with the circumflex scapular artery3. The thoracodorsal artery can send branches to the serratus anterior and teres major muscles; when penetrating the LDM, it forks in the horizontal and vertical muscular branches to perforate the musculocutaneous flap1,4,5. The LDM is secondarily vascularized by the perforating branches of the posterior intercostal and lumbar arteries6,7.
Taylor and Watanabe observed two vascular areas in the skin overlying the LDM6,7. The first area consists of a vascular network of direct anastomosis between the cutaneous perforators of the thoracodorsal artery and the scapula circumflex artery and the perforating branches of the ninth, tenth, and eleventh posterior intercostal arteries. The second vascular area is formed by the anastomosis network between the perforating branches of the subcostal artery and the first and second lumbar arteries7.
The musculocutaneous and muscular flaps of the LDM are the most versatile in plastic surgery and have been used to correct birth defects in cases of aplasia cutis congenita8 as well as reconstructions of diaphragmatic hernia congenita9 and myelomeningocele10,11.
OBJECTIVE
The purpose of this study was to analyze LDM morphology and vascularization in eight fetuses fixed with formaldehyde for possible use in intrauterine reconstructive surgeries.
METHOD
This work meets the standards of the National Council for Research Ethics Resolution 96/166 and was conducted at the Anatomy Department of the Federal University of Alagoas (FUAL).
Eight human fetuses (three female, five male) with gestational ages of 20-32 weeks harvested from miscarriages were dissected and legally donated to the FUAL by the "Estácio de Lima" Legal Medical Institute (Alagoas) and previously numbered by the FUAL anatomy sector.
The corpses were positioned in the supine horizontal12 position with the left arm in abduction. Z-shaped skin incisions were made in the axillary region and extended along the mid-axillary line. Next, a drape-covered cushion measuring 5 cm long and 14 cm wide was positioned along the left paraspinal line to elevate each fetus and facilitate access to the muscle.
The LDM was separated from its integument and the musculocutaneous flap-perforating branches of the posterior lumbar and intercostal arteries were sectioned. The muscle anterior margin was separated from its insertion into the iliac crest and the lower four ribs to create dorsal traction.
Once the artery and thoracodorsal vein were visible, the vascular bundle was dissected superior to the origin of the subscapular vessels in the artery and axillary vein. The subscapular artery and vein, scapular and thoracodorsal circumflex, branches to the serratus anterior muscle, and angular branch of the thoracodorsal artery were studied.
The measurements were performed in the above described position using an analog Mitutoyo® caliper. The subscapular artery was measured from its origin in the axillary artery to its bifurcation into the scapular circumflex and thoracodorsal arteries; on the other hand, the thoracodorsal artery was measured from the scapula circumflex artery to the branch emergence of the serratus anterior and from that point to the LDM input artery since the branch to the serratus anterior muscle curves the thoracodorsal artery when the LDM is pulled posteriorly. We measured the vein lengths using the same protocol.
The LDM was measured in a triangular manner to measure the length of the anterior margin from the tendon to the humerus to the iliac crest; from the muscle upper margin, which goes from the tendon to the humerus to the spinous process of the six inferior thoracic vertebrae; and from the posterior muscle margin, in its attachment to the thoracolumbar fascia, which runs from the spinous process of the last six thoracic vertebrae to its attachment to the iliac crest. We also measured the muscle length from its tendon to the input of the neurovascular pedicle.
The lengths of the thoracodorsal artery and thoracodorsal vein to the junction with the thoracodorsal nerve in the same fascia were measured. We then took a picture and did a schematic drawing of the axillary region of all dissected fetuses and described the axillary artery and vein as well as the anatomical variations found in the subscapular vessels and the scapular and thoracodorsal circumflex.
RESULTS
The general data of the studied fetuses are listed in Table 1.
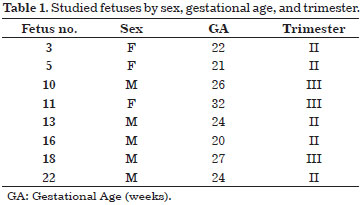
For each dissection, a representative drawing of the observed anatomical variations was made to illustrate the non-displayed branches in the axillary region photographs. In all cases, the veins were positioned anterior to the arteries. The drawings and images of the axillary region of each case are shown in Figures 1 a 8.
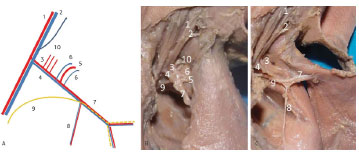
Figure 1. Left axillary region of Fetus 3. (A) Diagram of the neurovascular pedicle. (B) Photographs of the latissimus dorsi muscle in its anatomical position. (C) upon being dorsally pulled. 1. Axillary artery. 2 .Axillary vein. 3. Subscapular artery. 4. Subscapular vein. 5. Scapula circumflex artery. 6. Scapula circumflex vein. 7. Thoracodorsal artery and vein. 8. Branch of serratus anterior muscle. 9. Thoracodorsal nerve. 10. muscular branches of the subscapular artery.
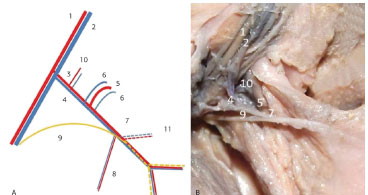
Figure 2. Left axillary region of Fetus 5. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Subscapular artery. 4. Subscapular vein. 5. Scapula circumflex artery. 6. Scapula circumflex vein. 7. thoracodorsal artery and vein. 8. Branch of the serratus anterior muscle. 9. Thoracodorsal nerve. 10. Muscle branches of subscapular artery. 11. Angular branch of the thoracodorsal artery.
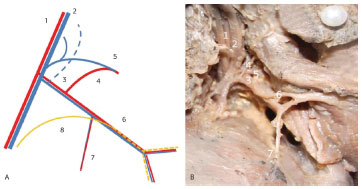
Figure 3. Left axillary region of Fetus 10. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Subscapular artery. 4. Scapula circumflex artery. 5. Scapula circumflex vein. 6. Thoracodorsal artery and vein. 7. Branch of the serratus anterior muscle. 8. Thoracodorsal nerve.
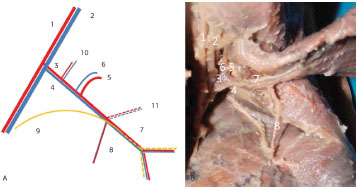
Figure 4. Left axillary region of Fetus 11. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Subscapular artery. 4. Subscapular vein. 5. Scapula circumflex artery. 6. Scapula circumflex vein. 7. Thoracodorsal artery and vein. 8. Branch of the serratus anterior muscle. 9. Thoracodorsal nerve. 10. Muscle branches of the subscapular artery. 11. Angular branch of the thoracodorsal artery.
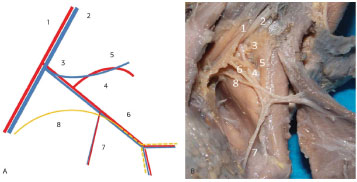
Figure 5. Left axillary region of Fetus 13. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Subscapular artery. 4. Scapula circumflex artery. 5. Scapula circumflex vein. 6. Thoracodorsal artery and vein. 7. Branch of the serratus anterior muscle. 8. Thoracodorsal nerve.
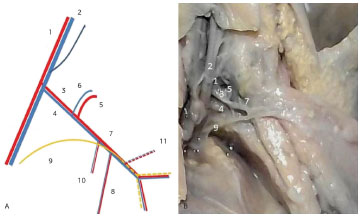
Figure 6. Left axillary region of Fetus 16. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Scapula circumflex artery. 4. Subscapular vein. 5. Scapula circumflex artery. 6. Scapula circumflex vein. 7. Thoracodorsal artery and vein. 8. Branch of the serratus anterior muscle. 9. Thoracodorsal nerve. 10. Branch of the subscapular muscle. 11. Angular branch of the thoracodorsal artery.
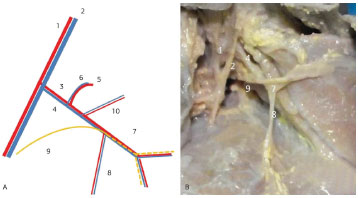
Figure 7. Left axillary region of Fetus 18. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Subscapular artery. 4. Subscapular vein. 5. Scapula circumflex artery. 6. Scapula circumflex vein. 7. Thoracodorsal artery and vein. 8. Branch of the serratus anterior muscle. 9. Thoracodorsal nerve. 10. Muscle branches of the subscapular artery.
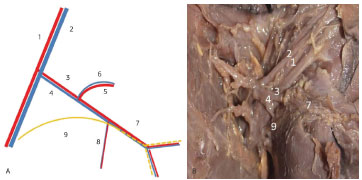
Figure 8. Left axillary region of Fetus 22. (A) Diagram of the neurovascular pedicle. (B) Photograph of the latissimus dorsi muscle dorsally pulled. 1. Axillary artery. 2. Axillary vein. 3. Subscapular artery. 4. Subscapular vein. 5. Scapula circumflex artery. 6. Scapula circumflex vein. 7. Thoracodorsal artery and vein. 8. Branch of the serratus anterior muscle. 9. Thoracodorsal nerve.
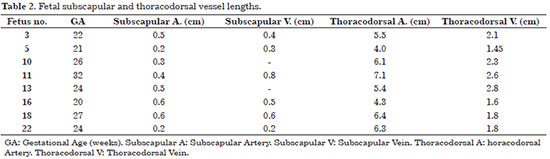
In all fetuses, the LDM was primarily vascularized by the thoracodorsal vessels, branches of the subscapular vessels. The subscapular vein bifurcates into the scapula circumflex and thoracodorsal veins in 75% of cases. In 25% of the studied fetuses, the subscapular vein was directly confluent with the axillary vein. The circumflex artery of the scapula was not a direct branch of the axillary artery in any of the fetuses. The length of the subscapular vein was 0.2-0.8 cm in fetuses at 24-32 weeks' gestation, respectively; on the other hand, the length of the subscapular artery was 0.2-0.6 cm in fetuses at 21-27 weeks' gestation, respectively. The length of the thoracodorsal vessels was 1.6-2.8 cm in fetuses at 20-24 weeks' gestation, respectively (Table 2).
The scapula circumflex vein was doubled in fetuses 3 and 5 (25%). None of the fetuses presented with a double scapula circumflex artery. Before entering the LDM, the thoracodorsal artery issued a branch to the serratus anterior muscle and the angular branch. In all fetuses, the branch to the serratus anterior muscle was unique. In fetuses 3, 5, 11, and 18, the angular branch was visualized (50%); in fetus 3 only (25%), it came from the branch to the serratus anterior muscle.
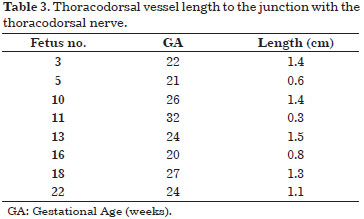
The thoracodorsal nerve joined the thoracodorsal vessels to form the neurovascular pedicle. The thoracodorsal artery length to the junction of the corresponding nerve in the pedicle ranged from 0.3 cm in the 32-week fetus and 1.5 cm in the 24-week fetus (Table 3).
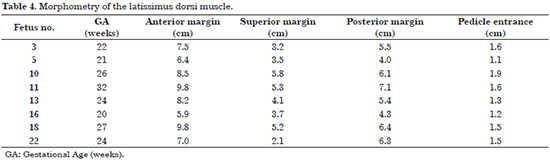
The LDM morphometry is described in Table 4. The distance between muscle insertion and the neurovascular pedicle input was 1.1 and 1.9 cm in the 21- and 26-week fetuses, respectively. In all fetuses, the anterior muscle margin was positioned in the mid-axillary line.
DISCUSSION
The comparisons were based on anatomical studies of adults due to the lack of published studies related to LDM anatomy in fetuses accessed in the PUBMED, BVS, and SCIELO databases.
In all studied cases, the thoracodorsal artery was a branch of the subscapular artery, a similar result obtained in studies of adults by Rowsell et al.4 and Bartlett et al.1. Regarding the venous anatomy, the subscapular vein was confluent with the axillary vein in 25% of cases. Bartlett found this anatomical variation in 12% of cases; a double scapula circumflex artery was found in 8% of dissections, while a double scapula circumflex vein was found in 14% of dissections. In this study, a double circumflex vein was found in 25% of cases, but this morphology was not observed in the arterial system.
All of the fetuses had only one branch of the thoracodorsal artery for the serratus anterior muscle. Bartlett1 e Rowsell4 found only one branch in 54% and 72% of cases, respectively. However, Safwat & Rahman13 obtained divergent results in which two branches to the serratus anterior muscle were seen in a higher percentage of cases (42.9%).
The angular branch of the thoracodorsal artery was found in 50% of cases; only 25% originated from the branch to the serratus anterior muscle or the thoracodorsal artery. Seneviratne14 found similar results in 51% of dissections in which the angular branch originated from the thoracodorsal artery; 20% originated in a trifurcation pattern in which the thoracodorsal artery gave off a branch to the serratus anterior muscle, continued toward the LDM, and issued an angular branch; and in 21% originated from the branch to the serratus anterior muscle. Smaniotto et al.15 found divergent results: In 92.8% of his dissections, the angular branch originated from the branch to the serratus anterior muscle, while in 7.2%, it originated from the thoracodorsal artery in a trifurcation pattern.
The angular branch has great importance because irrigating the inferior angle of the scapula allows vascularized bone grafting of the region in a combined flap of the LDM or serratus anterior muscle15,16, which can be used for the reconstruction of orofacial defects such after tumor resection since the muscular component allows the coverage of large body segments, which limits complications such as infection and fistula formation16.
The LDM is considered a type V Mathes and Nahai flap since it is primarily vascularized by the thoracodorsal vessels and secondarily vascularized by the musculocutaneous perforation of the posterior and lumbar intercostal7-9 arteries. The proximal LDM flap is based on the primary vascular pedicle, while a flap that is based on secondary vascularization is a reverse flap. Both flaps were studied by Meuli-Simmen et al.17 for myelomeningocele coverage (MMC) in fetuses and are already used fir MMC correction in neonates11.
The anatomical studies of Manchot and Salmon defined the existence of cutaneous vascular territories in which the scapular and thoracodorsal were adjacent18. Taylor and Watanabe consolidated the two vascular areas in the skin overlying the LDM6,7. The first territory consists of a vascular network of direct anastomosis between cutaneous perforation of the thoracodorsal artery and the scapula circumflex artery and the perforating branches of the ninth, tenth, and eleventh posterior intercostal arteries. The second vascular territory is formed by a network of anastomosis between perforating branches of the subcostal artery and the first and second lumbar7 arteries. It is possible to use these areas for the individualization and use of major flaps, such as the perforator flap of the thoracodorsal artery and the scapular fasciocutaneous flap, that are based on the scapula circumflex artery18.
In its insertion in the humerus, the LDM twists 180º1,2. This little-studied segment can be sectioned to increase the rotation arc of the LDM in reconstructions involving the breasts and neck, which enables positioning of the LDM flap to a region below the zygomatic arch19. Its section may be designed to create a reverse flap that is used for MMC11,17 correction. In adults, no study has taken measurements of the LDM insertion segment in the humerus. Because of its importance, this study measured the LDM length from its humeral insertion to the entrance of the vascular pedicle, which was 1.1-1.9 cm in fetuses 20-32 weeks' gestational age. However, the correlation between gestational age and tendon length was not studied.
Intrauterine surgery remains controversial, and its indications are restricted to conditions that undermine survival and cause high degrees of morbidity for the child. The preliminary results of the Myelomeningocele Management Study showed significantly improved symptoms of nerve damage caused by MMC at birth despite the risk of prematurity and spontaneous rupture of the membranes20. The MLD flap, which is widely used in reconstructive surgery in adults, will have great future importance as our knowledge of intrauterine surgery advances. The knowledge of LDM vascular anatomy in fetuses enables the surgeon to choose the technique that best applies to each defect11.
CONCLUSION
The morphometry and reduced anatomic variations of the LDM vascular pedicle in the fetuses studied here enables research on the use of LDM in intrauterine surgical reconstructions.
REFERENCES
1. Bartlett SP, May JW JR, Yaremchuk MJ. The latissimus dorsi muscle: a fresh cadaver study of the primary neurovascular pedicle. Plast Reconstr Surg. 1981;67(5):631-6. http://dx.doi.org/10.1097/00006534-198105000-00010. PMid:7232584.
2. Moore KL, Dalley AF, Agur AMR. Anatomia orientada para a clínica. 6th ed. Filadélfia: Guanabara Koogan; 2010.
3. Costa KCM, Kiyohara LY, Jorge HMH, Araújo MP, Torres LR, Barros TEP FO. Estudo do alcance do retalho do músculo grande dorsal para o revestimento cutâneo da coluna. Acta Ortop Bras. 2009;17(5):305-8. http://dx.doi.org/10.1590/S1413-78522009000500011.
4. Rowsell AR, Eisenberg N, Davies DM, Taylor GI. The anatomy of the thoracodorsal artery within the latissimus dorsi muscle. Br J Plast Surg. 1986;39(2):206-9. http://dx.doi.org/10.1016/0007-1226(86)90083-4. PMid:3697562.
5. Saijo M. The vascular territories of the dorsal trunk: a reappraisal for potential flap donor sites. Br J Plast Surg. 1978;31(3):200-4. http://dx.doi.org/10.1016/S0007-1226(78)90082-6. PMid:354722.
6. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41. http://dx.doi.org/10.1016/0007-1226(87)90185-8. PMid:3567445.
7. Watanabe K, Kiyokawa K, Rikimaru H, Koga N, Yamaki K, Saga T. Anatomical study of latissimus dorsi musculocutaneous flap vascular distribution. J Plast Reconstr Aesthet Surg. 2010;63(7):1091-8. http://dx.doi.org/10.1016/j.bjps.2009.05.042. PMid:19581133.
8. Yang JY, Yang WG. Large scalp and skull defect in aplasia cutis congenita. Br J Plast Surg. 2000;53(7):619-22. http://dx.doi.org/10.1054/bjps.2000.3413. PMid:11000081.
9. Barbosa RF, Rodrigues J, Correia-Pinto J, Costa-Ferreira A, Cardoso A, Reis JC, et al. Repair of a large congenital diaphragmatic defect with a reverse latissimus dorsi muscle flap. Microsurgery. 2008;28(2):85-8. http://dx.doi.org/10.1002/micr.20455. PMid:18220249.
10. El-khatib HA. Large thoracolumbar meningomyelocele defects: incidence and clinical experiences with different modalities of latissimus dorsi musculocutaneus flap. Br J Plast Surg. 2004;57(5):411-7. http://dx.doi.org/10.1016/j.bjps.2003.12.035. PMid:15191821.
11. Zakaria Y, Hasan EA. Reversed turnover latissimus dorsi muscle flap for closure of large myelomeningocele defects. J Plast Reconstr Aesthet Surg. 2010;63(9):1513-8. http://dx.doi.org/10.1016/j.bjps.2009.08.001. PMid:19726259.
12. Andrade FAG, Servant JM, Ferreira LM, Revol M, Traber H, Nascimento CP JR, et al. Decúbito dorsal no retalho microcirúrgico do músculo grande dorsal - técnica de J. M. Servant. Rev Soc Bras Cir Plást. 2000;15(2):35-46.
13. Safwat MD, Rahman WA. Anatomic study of the neurovascular pedicle of the serratus anterior muscle. Bull Alex Fac Med. 2007;43(4):845-52.
14. Seneviratne S, Duong C, Taylor GI. The angular branch of the thoracodorsal artery and its blood supply to the inferior angle of the scapula: an anatomical study. Plast Reconstr Surg. 1999;104(1):85-8. http://dx.doi.org/10.1097/00006534-199907000-00012. PMid:10597678.
15. Smaniotto PHS, Silva JCF, Doi A, Ferreira MC. Estudo anatômico do ramo angular da artéria tóracodorsal e suas implicações no transplante ósseo vascularizado do ângulo da escápula. Rev Bras Cir Plást. 2009;24(4):414-9.
16. L'Heureux-Lebeau B, Odobescu A, Harris PG, Guertin L, Danino AM. Chimaeric subscapular system free flap for complex oro-facial defects. J Plast Reconstr Aesthet Surg. 2013;66(7):900-5. http://dx.doi.org/10.1016/j.bjps.2013.02.031. PMid:23582503.
17. Meuli-Simmen C, Meuli M, Adzick NS, Harrison MR. Latissimus dorsi flap procedures to cover myelomeningocele in utero: a feasibility study in human fetuses. J Pediatr Surg. 1997;32(8):1154-6. http://dx.doi.org/10.1016/S0022-3468(97)90673-4. PMid:9269961.
18. Ishida LH. Estudo anatômico comparativo entre o retalho escapular e o retalho perfurante da artéria toracodorsal [Dissertação]. São Paulo: Departamento de Cirurgia, Faculdade de Medicina, Universidade de São Paulo; 2006.
19. Masson J, Couturaud B, Martinaud C, Ledanvic M, Revol M, Servant JM. Reconstrucción mamaria: técnicas e indicaciones. In: Enciclopedia Médico-Quirúrgica: Cirugía Plástica 2. Paris: Elsevier; 2000. p. 1-23.
20. Adzick NS. Fetal surgery for myelomeningocele: trials and tribulations. Isabella Forshall Lecture. J Pediatr Surg. 2012;47(2):273-81. http://dx.doi.org/10.1016/j.jpedsurg.2011.11.021. PMid:22325376.
Faculdade de Medicina, Universidade Federal de Alagoas (Ufal), Maceió, AL, Brazil
Institution: Study performed at the Faculdade de Medicina, Universidade Federal de Alagoas, Maceió, AL, Brazil.
Corresponding author:
Fernando Gomes de Andrade
Universidade Federal de Alagoas (Ufal)
Avenida Lourival Melo Mota, s/n - Campus A.C. Simões
Maceió, AL, Brazil Zip Code 57072-970
E-mail: fernandogomescirurgiaplastica@hotmail.com
Article received: June 23, 2014.
Article accepted: December 12, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter