

Original Article - Year 2015 - Volume 30 -
Reconstruction of a burned nipple-areola complex using an autonomized star flap
Reconstrução do complexo areolomamilar da mama queimada com retalho trilobado autonomizado
ABSTRACT
INTRODUCTION Reconstruction of the nipple-areola complex is the final stage of breast reconstruction. The most common nipple reconstruction techniques use local flaps or grafts. However, these techniques in cases of burns produce undesirable outcomes due to the decreased vascularization of damaged skin. The objective of this work was to evaluate the use of the autonomized star flap in the nipple reconstruction of burned breasts.
METHODS: Nipples were reconstructed in eight female patients in two surgeries each.
RESULTS: There were no complications such as necrosis, dehiscence, complete loss of projection of the new nipple, or infection. The mean projection at the end of surgery was 15.25 mm; 6 months after reconstruction, it was 3 mm, showing stability. All patients were satisfied with their results.
CONCLUSION: We conclude that autonomization leads to safe reconstruction of the nipple on burned breasts and maintains a satisfactory minimal projection of the reconstructed nipple.
Keywords: Burned breast; Nipple reconstruction; Breast sequelae.
RESUMO
INTRODUÇÃO A reconstrução do complexo areolomamilar é a fase final da reconstrução mamária. As técnicas de reconstrução do mamilo mais utilizadas são com retalhos locais ou enxertos. A utilização destas técnicas em mamas que sofreram queimaduras apresenta resultados indesejados, em decorrência da menor vascularização da pele lesada. O objetivo deste trabalho foi avaliar a utilização do retalho trilobado autonomizado na reconstrução do mamilo em mamas queimadas.
MÉTODOS: Oito pacientes do sexo feminino tiveram seus mamilos reconstruídas em dois tempos cirúrgicos.
RESULTADOS: Não ocorreram complicações, como necrose, deiscência, perda completa da projeção do novo mamilo ou infecção. A projeção média ao término da cirurgia foi de 15,25 mm e, após seis meses de reconstrução, foi de 3 mm, permanecendo estável. Todas as pacientes ficaram satisfeitas com os resultados.
CONCLUSÃO: Concluímos que a autonomização deu segurança à reconstrução do mamilo em mamas queimadas e manteve projeção mínima satisfatória do mamilo reconstruído.
Palavras-chave: Mama queimada; Reconstrução de mamilo; Sequela de mama.
Rebuilding the nipple-areola complex (NAC) represents the final stage of breast reconstruction. Many techniques have been described for NAC reconstruction; however, few have been described in burned breasts.
Some of the techniques used to reconstruct the nipple include a contralateral nipple graft (part of the contralateral nipple), composite grafts of auricular cartilage and skin, vaginal mucosa graft, and various local flaps1,2. The grafting of the contralateral nipple is more favorable in terms of color and texture3-5. However, there is not always a sufficient amount of nipple tissue for sharing with the other breast, the graft is not always integrated, projection loss is considerable, and morbidity of the donor area is increased. Grafting can also be combined with the use of prostheses and cartilage grafts6 to maintain the projection, but, as with any foreign body, are at a greater risk of infection and extrusion or reabsorption. For these reasons, many surgeons and patients may refuse this technique and prefer to use local tissue for reconstruction.
The main techniques used are based on designs that can elevate the local tissues, which may or may not be associated with the placement of a cartilage graft that is generally removed from the pinna4,7.
Many grafting techniques with different designs exist, such as the triangular skin flap, opposite triangle, purse-string suture, skate flap, "S" flap, and arrow flap5,6,8,9-11, each of which has its special features, advantages, and disadvantages. In all cases, the aims are to reach similarity with the contralateral NAC and maintain the projection of the reconstructed nipple.
One of the most common reconstruction techniques is the star or trilobed flap. Various published studies have shown a low rate of complications and low loss of projection of 41-60% over 1 year after the surgery, primarily within the first 6 months post-surgery12,13.
For areolar reconstruction, techniques include a split- or total-thickness skin graft (the vaginal mucosa, inner face of the thigh, or contralateral areola) and intradermal tattoo7,14.
Based on the literature, the authors began to perform nipple reconstructions on burned breasts using the star flap. The first cases, however, presented partial or full flap necrosis (Figure 1), although this has not been reported in the literature14,15.
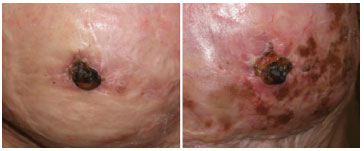
Figure 1. Two examples of complete flap necrosis in a reconstructed nipple.
Thus, due to flap necrosis, the authors proposed autonomizing16 them in an attempt to reduce these complications.
OBJECTIVE
The objective of this study was to evaluate the evolution of nipples of burned breasts reconstructed using autonomized star flaps.
METHODS
Eight women aged 18-34 years with second- or third-degree burns on the breasts and absence of the NAC who were treated with the autonomized star flap technique were studied between May and November 2011 (Figure 2).
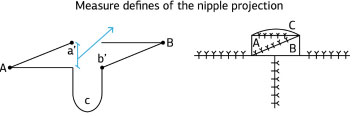
Figure 2. Left, schematic of the flap to be prepared. The lines represent demarcations of the incisions (A and B - side flaps; C - flap covering the new nipple). The tip of flap A is sutured to point b', while the tip of flap B is sutured to point a'. Right, the nipple profile result at the end of the second surgery.
The positioning of the new nipple was made symmetrically to the contralateral one; in its absence, it was placed at the apex of the breast cone. The desired projection at the end of surgery was 12-14 mm from the base measured by a caliper placed at the base of the lower portion of the reconstructed nipple. The procedures were performed under local anesthesia with 1% lidocaine.
1st Surgical procedure
Demarcation of flaps in accordance with Drawing 1 and an incision in the skin to the subcutaneous tissue without any type of detachment, achievement of hemostasis, and closure of the incisions with monofilament 5-0 nylon sutures (Figure 2).
2nd Surgical procedure - 15 days after the first surgery
Achievement of the incisions in the same locations of the first operation, followed by the removal of flaps with subcutaneous detachment, maintaining the pedicle at its base. This is followed by thinning of the flap (partial removal of subcutaneous tissue) as needed for the assembly of the nipple. Closure was performed with simple monofilament nylon 5-0 without tension, and the donor area in two planes, with subdermal monofilament nylon 4-0 and nylon monofilament 5-0 in skin (Figure 2).
After the second surgery, the wound is dressed with several layers of cotton gauze with a hole in the middle through which the new nipple is projected to prevent its compression by clothing. After the sutures are withdrawn on day 7, a silicone nipple shield, conventionally purchased in pharmacies and used by breastfeeding women, is used.
Evaluation of the results
Monthly follow-up was performed in the postoperative period. The reconstructed nipples were evaluated for both projection and complications such as dehiscence, necrosis, pain, and infection. The projection was initially evaluated with a pachymeter at the end of the second surgery and 15 days and 1, 3, 6, and 18 months postoperatively.
At 6 months post-reconstruction, the patients were queried whether they were satisfied with the results, would again undergo the procedure, or would recommend the surgery to other patients.
RESULTS
In the eight operated patients, no complications regarding anesthesia, dehiscence, infection, pain, or necrosis were observed.
The initial mean nipple projection was 15.25 ± 1.47 mm. At the end of the first month, an average 45% of the initial projection was lost, while 66% was lost at the third month. At 18 months post-reconstruction, 15-40% of the initial nipple projection remained (Figures 3-13).
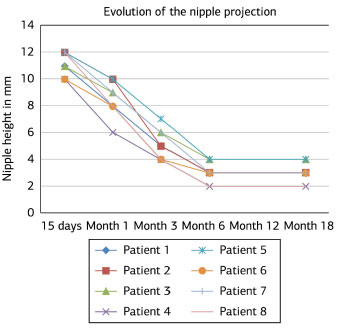
Figure 3. Evolution of the reconstructed nipple projection at 15 days and 1, 3, 6, and 18 months postoperatively.
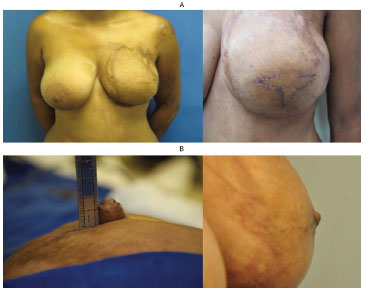
Figure 4. (A) Left: left breast without nipple reconstruction. Right: autonomized flaps with sutures after the first surgery. (B) Left: appearance of the nipple at the end of the second surgery. Right: appearance of the nipple after 12 months of follow-up.

Figure 5. (A) Left: breasts without reconstruction; both breasts had their nipple reconstructed. Right: appearance of the right nipple after 12 months of follow-up. (B) The left nipple after 12 months of follow-up.

Figure 6. Left: left breast without nipple reconstruction. Right: appearance of the left nipple after 12 months of follow-up.

Figure 7. Left: right breast without nipple reconstruction. Right: appearance of the right nipple with 12 months of follow-up.
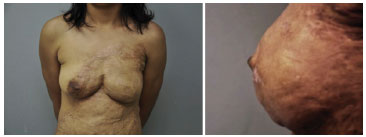
Figure 8. Left: left breast without nipple reconstruction. Right: appearance of the left nipple after 12 months of follow-up.
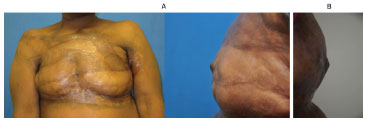
Figure 9. (A) Left: breasts without reconstruction; both breasts had their nipple reconstructed. Right: appearance of the left nipple after 12 months of follow-up. (B) Appearance of the left nipple after 12 months of follow-up.

Figure 10. (A) Left breast without reconstruction. (B) Appearance of the left nipple at the end of the second surgery.

Figure 11. (A). Left: breast without reconstruction. Middle and right: appearance of the left nipple after 12 months of follow-up. (B) Reconstruction sequence (left to right): surgical demarcation during the first surgery; autonomized flaps; reconstructed nipple at the end of the second surgery; reconstructed nipple 3 months after surgery.

Figure 12. End result of the nipple-areola complex reconstruction (tattooed areolas).

Figure 13. Left: end result of nipple and right areolar reconstruction using a skin graft. Right: graft on postoperative day 7.
All patients were satisfied with the results, saying that they would undergo surgery again and would recommend the procedure to another patient.
DISCUSSION
The most common changes found in sequelae of breast burns are related to the shape and poor quality of skin coverage - composed of scars - with skin elasticity loss and/or surface irregularities. Thus, cicatricial retractions cause major breast shape distortions.
NAC destruction may also occur. Several surgical techniques have been used to mitigate these effects, normally by the broad release of cicatricial retractions and the skin coverage of the open areas, using split-thickness skin flaps, local or remote flaps, or even skin expanders17.
NAC restoration represents the final stage of breast reconstruction and is a challenge to the plastic surgeon18,19. Retrospective analyses show that patient satisfaction in relation to breast reconstruction is directly related to the presence of the NAC20-22. Moreover, patients with sequelae of breast burns yearn for full breasts despite their marks and scars.
The main goals of NAC reconstruction are maintenance of nipple projection, coloring of the areola, and positional symmetry13. For this reason, several techniques have emerged over the last 30 years, but there is no universal preference of surgeons who perform breast reconstructions23.
The difficulties typically encountered with the use of local flaps are skin necrosis of the reconstructed nipple, infection, dehiscence, and especially long-term loss of projection8,15. This loss is thought to be due to the deficiency of normal structures that comprise the nipple, such as smooth muscle and lactiferous ducts, and are responsible for its characteristic firmness. These tissues suffer from the retraction of the flap itself as well as with the peripheral retraction that occurs during the healing process24.
Burn victims usually have an additional aggravating factor in nipple reconstructions: poor-quality neighboring tissues used in the construction of local flaps, with their low elasticity, varied thickness, thinner dermis, and poor vascularization15. These characteristics lead to a higher incidence of surgical complications, especially those related to poor vascularization, specifically pain or tissue necrosis of the reconstructed nipple.
Few studies have focused on this topic14,15,17,25. Due to the lack of information in this area, articles on nipple reconstruction in post-mastectomy breasts were also consulted. The trilobe or star flap most effectively protected against projection loss3-6,8-13,20,21,23,24,26,27.
Despite care taken during reconstruction, particularly in relation to the vascularization of small flaps, complete or near-complete flap necrosis occurred in the first two cases (Figure 1), impeding the goals and indicating inadequate vascularization of the adjacent skin used to implement this type of procedure, which has not been reported in the literature.
The attempt to solve the problem was sought in the basic principles of plastic surgery using autonomized flaps16,28. Using this simple feature, the occurrence of tissue necrosis was eliminated. Subsequently, the greatest challenge in nipple reconstruction was long-term attainment of the final outcome on the basis of the complete loss of projection of reconstructed nipples, possibly as a result of tension within neighboring tissues. This problem was overcome with a 20% increase in reconstructed nipple size. Nipples with 15-mm projection were obtained at the end of the surgery. Nevertheless, after 6 months, the reconstructed nipples (Figure 4) had decreased to approximately 20-30% of the initial projection.
Despite the low tissue elasticity, we encountered no difficulty raising the flaps. In all cases, however, there was a need to significantly thin the flap to retain almost the dermis only to transpose the flaps and sutures without tension.
These initial results are promising, with a mean follow-up time of 1.5 years, and the nipple projection achieved at 6 months postoperatively was retained.
An assessment of the psychological aspects indicated that, regardless of the technique used for the nipple reconstruction and the results obtained, the vast majority of patients were satisfied with the results and recommended the technique to other patients, suggesting that what really matters is the presence of a nipple, even if the results are not ideal18,19,22. Although no specific test was used in this study, patient satisfaction is demonstrated by the fact that other patients requested nipple reconstruction after having talked to and seen the results of other patients who underwent the surgery.
CONCLUSION
The use of autonomized flaps for the nipple reconstruction of burned breasts displayed no complications, maintained acceptable nipple projection at 18 months, and was deemed satisfactory by postoperative patients.
REFERENCES
1. Mendelson BC. Results of nipple areola reconstruction. Aust N Z J Surg. 1983;53(1):63-6. http://dx.doi.org/10.1111/j.1445-2197.1983.tb02398.x. PMid:6338874.
2. Wiemer DR, Freeman BS. Bilateral reconstruction of the nipple-areola complex. Plast Reconstr Surg. 1976;58(3):310-3. http://dx.doi.org/10.1097/00006534-197609000-00009. PMid:785499.
3. Asplund O. Nipple and areola reconstruction. A study in 79 mastectomized women. Scand J Plast Reconstr Surg. 1983;17(3):233-40. http://dx.doi.org/10.3109/02844318309013123. PMid:6673090.
4. Kargül G, Deutinger M. [Reconstruction of the breast areola complex. Comparison of different techniques]. Handchir Mikrochir Plast Chir. 2001;33(2):133-7. PMid:11329892.
5. Richter DF, Reichenberger MA, Faymonville C. [Comparison of the nipple projection after reconstruction with three different methods]. Handchir Mikrochir Plast Chir. 2004;36(6):374-8. http://dx.doi.org/10.1055/s-2004-821031. PMid:15633081.
6. Guerra AB, Khoobehi K, Metzinger SE, Allen RJ. New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg. 2003;50(1):31-7. http://dx.doi.org/10.1097/00000637-200301000-00006. PMid:12545106.
7. Muruci A, Dantas JJ, Noguerira LR. Reconstruction of the nipple-areola complex. Plast Reconstr Surg. 1978;61(4):558-60. http://dx.doi.org/10.1097/00006534-197804000-00010. PMid:345308.
8. Banducci DR, Le TK, Hughes KC. Long-term follow-up of a modified Anton-Hartrampf nipple reconstruction. Ann Plast Surg. 1999;43(5):467-9, discussion 469-70. http://dx.doi.org/10.1097/00000637-199911000-00001. PMid:10560860.
9. Gamboa-Bobadilla GM. Nipple reconstruction: the top hat technique. Ann Plast Surg. 2005;54(3):243-6. PMid:15725823.
10. Hugo NE, Sultan MR, Hardy SP. Nipple-areola reconstruction with intradermal tattoo and double-opposing pennant flaps. Ann Plast Surg. 1993;30(6):510-3. http://dx.doi.org/10.1097/00000637-199306000-00006. PMid:8368776.
11. Shestak KC, Gabriel A, Landecker A, Peters S, Shestak A, Kim J. Assessment of long-term nipple projection: a comparison of three techniques. Plast Reconstr Surg. 2002;110(3):780-6. http://dx.doi.org/10.1097/00006534-200209010-00010. PMid:12172139.
12. Eskenazi L. A one-stage nipple reconstruction with the "modified star" flap and immediate tattoo: a review of 100 cases. Plast Reconstr Surg. 1993;92(4):671-80. http://dx.doi.org/10.1097/00006534-199309001-00017. PMid:8356129.
13. Few JW, Marcus JR, Casas LA, Aitken ME, Redding J. Long-term predictable nipple projection following reconstruction. Plast Reconstr Surg. 1999;104(5):1321-4. http://dx.doi.org/10.1097/00006534-199910000-00012. PMid:10513912.
14. Pensler JM, Haab RL, Parry SW. Reconstruction of the burned nipple-areola complex. Plast Reconstr Surg. 1986;78(4):480-5. http://dx.doi.org/10.1097/00006534-198610000-00007. PMid:3532150.
15. Motamed S, Davami B. Postburn reconstruction of nipple-areola complex. Burns. 2005;31(8):1020-4. http://dx.doi.org/10.1016/j.burns.2005.06.014. PMid:16288961.
16. Dhar SC, Taylor GI. The delay phenomenon: the story unfolds. Plast Reconstr Surg. 1999;104(7):2079-91. http://dx.doi.org/10.1097/00006534-199912000-00021. PMid:11149772.
17. Ozgur F, Gokalan I, Mavili E, Erk Y, Kecik A. Reconstruction of postburn breast deformities. Burns. 1992;18(6):504-9. http://dx.doi.org/10.1016/0305-4179(92)90186-X. PMid:1489503.
18. Wilkins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106(5):1014-25, discussion 1026-7. http://dx.doi.org/10.1097/00006534-200010000-00010. PMid:11039373.
19. Yurck D, Farrar W, Andersen BL. Breast cancer surgery: comparing surgical groups and determining individual differences in post-operative sexuality and body change stress. J Consult Clin Psychol. 2000;68:679-709.
20. Little JW. Nipple areolar reconstruction. In: Cohen M, editor. Mastery of plastic and reconstructive surgery. Boston: Little, Brown; 1994.
21. Kroll SS. Integrated breast mound reduction and nipple reconstruction with the wraparound flap. Plast Reconstr Surg. 1999;104(3):687-93. http://dx.doi.org/10.1097/00006534-199909010-00011. PMid:10456519.
22. Wellisch DK, Schain WS, Noone RB, Little JW 3RD. The psychological contribution of nipple addition in breast reconstruction. Plast Reconstr Surg. 1987;80(5):699-704. http://dx.doi.org/10.1097/00006534-198711000-00007. PMid:3671562.
23. Kroll SS. Nipple reconstruction with the double-opposing tab flap. Plast Reconstr Surg. 1999;104(2):511-4, discussion 515-7. http://dx.doi.org/10.1097/00006534-199908000-00030. PMid:10654699.
24. Farhadi J, Maksvytyte GK, Schaefer DJ, Pierer G, Scheufler O. Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg. 2006;59(1):40-53. http://dx.doi.org/10.1016/j.bjps.2005.08.006. PMid:16482789.
25. Thai KN, Mertens D, Warden GD, Neale HW. Reduction mammaplasty in postburn breasts. Plast Reconstr Surg. 1999;103(7):1882-6. http://dx.doi.org/10.1097/00006534-199906000-00012. PMid:10359249.
26. Weiss J, Herman O, Rosenberg L, Shafir R. The S nipple-areola reconstruction. Plast Reconstr Surg. 1989;83(5):904-6. http://dx.doi.org/10.1097/00006534-198905000-00026. PMid:2710842.
27. Cheng MS, Ho CM, Cheung WY, Or A, Wong WM. Nipple-areoa reconstruction in autologous breast reconstruction: Chinese patients' perspective. Ann Plast Surg. 2004;53(4):328-33. http://dx.doi.org/10.1097/01.sap.0000137247.53249.a1. PMid:15385765.
28. Morris SF, Taylor GI. Predicting the survival of experimental skin flaps with a knowledge of the vascular architecture. Plast Reconstr Surg. 1993;92(7):1352-61. PMid:8248411.
1. Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo (USP), São Paulo, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Study performed at the Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brazil.
Corresponding author:
Luiz Philipe Molina Vana
Rua Batataes, 460 - Jardim Paulista
São Paulo, SP, Brazil Zip Code 01423-010
E-mail: philipe@uol.com.br
Article received: May 23, 2014.
Article accepted: August 31, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter