

Original Article - Year 2015 - Volume 30 -
Diced cartilage graft to increase the nasal radix
Cartilagem fragmentada para aumento do radix nasal
ABSTRACT
INTRODUCTION: The main complaint of patients visiting plastic surgery clinics for rhinoplasty is the nasal dorsum. Cartilage grafts are routinely used in the nasal radix to reduce inappropriate nasofacial angles or redefine the transition point of the radix and then lengthen or shorten the nose. The aim of this study is to present cartilage nasal radix grafts prepared with diced cartilage and introduced to the radix with the aid of a syringe.
METHOD: We evaluated the surgical procedure and the results obtained by analyzing the medical records of 37 patients who underwent this surgery between May 1, 2011 and May 1, 2013.
RESULTS: In all cases, we achieved the expected result of successfully increasing the nasal radix. No graft absorption was clinically detected.
CONCLUSION: The use of a diced cartilage graft as described in this study effectively increased the nasal radix.
Keywords: Rhinoplasty; Cartilage; Graft; Nasal cartilage.
RESUMO
INTRODUÇÃO: A principal queixa dos pacientes que procuram as clínicas de cirurgia plástica para serem submetidos a rinoplastia é o dorso nasal. A utilização de enxerto cartilaginoso em radix nasal é rotineira e suas indicações habituais são para diminuir o ângulo nasofacial inadequado ou para redefinir o ponto de transição do radix, para alongamento ou encurtamento do nariz. Este trabalho tem o intuito de apresentar a enxertia de cartilagem do radix nasal, com cartilagem fragmentada e introduzida até o radix com seringa.
MÉTODO: Foi analisado o ato cirúrgico e seu resultado através da revisão de prontuários dos pacientes submetidos ao ato cirúrgico no período de 1/maio/2011 a 1/maio/2013, totalizando 37 casos.
RESULTADOS: Em todos os casos, conseguiu-se o resultado planejado de aumento do radix nasal com sucesso. Não foi observada absorção clinicamente detectável do enxerto.
CONCLUSÃO: A utilização do enxerto de cartilagem fragmentada realizada da forma descrita neste trabalho mostrou-se eficaz para a elevação do radix nasal.
Palavras-chave: Rinoplastia; Cartilagem; Enxerto; Cartilagens nasais.
The main complaint of patients visiting plastic surgery clinics for rhinoplasty is the nasal dorsum. The concept of an esthetically harmonious nasal dorsum can be subjective. In 2002, McKinney & Sweis1 reported a measurement system to determine the ideal proportion of the nose, thus providing the surgeon with parameters to define a balanced nose: the length, projection, rhinion, and radix height should in a ratio of 2:1:1:0.75. When altering the tip and the dorsum to provide a balanced nose, it may be necessary also to increase or reduce the nasal radix.
The use of cartilage grafts in the nasal radix is routine and indicated to reduce an inappropriate nasofacial angle2 or redefine the transition point of the radix to then lengthen or shorten the nose3. Historically, the most commonly used grafts were prepared from whole cartilage and are known as onlay grafts. However, the use of diced grafts regained importance after recent publications in rhinoplasty in particular4,5.
In this study, we proposed the use of a diced cartilage graft to increase the nasal radix and obtain a more ideal nasal tip-dorsum-radix ratio. The aim of this study was to present a cartilage nasal radix graft prepared with crushed and diced cartilage and introduced to the radix with the aid of a syringe to obtain a satisfactory result without rendering the graft visible.
This study was approved by the Research Ethics Committee - CEP (CAAE 17737913.8.0000.5430) on July 30, 2013 under protocol number 342.764.
METHODS
In this study, we analyzed the medical records of patients who underwent radix graft placement and evaluated their postoperative course longitudinally during the follow-up period. The patients were evaluated on days 7, 15, and 30; after 3 and 6 months; and after 1 and 2 years. Dorsal contour and patient satisfaction were assessed.
A total of 37 patients underwent this surgical procedure between May 1, 2011 and May 1, 2013. The access for all patients was through endonasal rhinoplasty, under local anesthesia and sedation.
The nasal dorsum was detached up to the nasal radix. This allowed preparation of the graft receiving area, which was detached in the demarcated region and the exact size of the graft. The volume to be grafted was determined by the injection of an anesthetic into the radix until the dorsal esthetic line was reached. The volume of the diced cartilage was the same as that of the local anesthetic applied.
The grafts were obtained from the nasal septum, nasal dorsum, and lateral portion of the alar cartilage. After isolation, the cartilage graft was crushed in the Cottle cartilage (Figure 1) and diced into 2-mm fragments on a Sheen plate using a No. 11 scalpel (Figure 2).
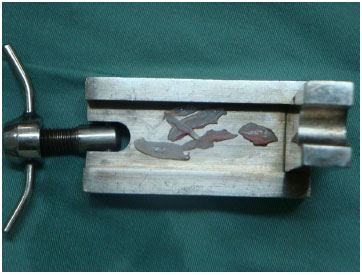
Figure 1. Cartilage grafts used.
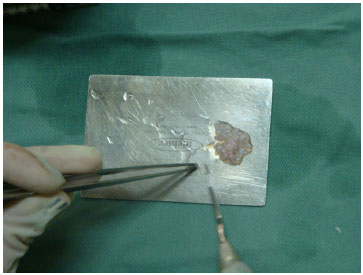
Figure 2. Diced cartilage pieces.
The crushed and diced cartilage was then introduced into an insulin syringe (1 mL) that was previously prepared6 (Figure 3) by cutting of the tip with Mayo scissors that are normally used for coarse tissue.

Figure 3. Prepared syringe.
The rhinoplasty continued as planned, and at the end of the surgery, when we proceeded to close the incision, we left part of the intercartilaginous incision above one of the nostrils open. We then inserted the syringe into this orifice until the tip reached the nasal radix (Figure 4) and slowly inserted the diced graft by pressing the plunger. This was shaped to the effect desired by the patient (Figure 5). This procedure can be repeated until the volume required is reached, which is usually predetermined by the injection of the local anesthetic.

Figure 4. Introduction of the syringe.

Figure 5. Introduction of the cartilage.
Once the graft was introduced and shaped (Figure 6), we started nasal microporation by placing the first strip above the grafted area to prevent graft displacement. The micropored region was that following the radix to the nasal tip (Figure 7).

Figure 6. Positioned and shaped cartilage.

Figure 7. Microporing.
RESULTS
The 37 patients were monitored postoperatively and underwent periodic evaluations on days 7, 15, and 30; after 3 and 6 months; and after 1 and 2 years. We operated on six men and 31 women who were 18-55 years old. In all cases, we obtained the expected results, i.e. successful increase of the nasal radix (Figures 8-13). A consolidated diced graft was observed during the late clinical follow-up period and the patient did not present any shape deformities. No graft absorption was clinically detected when the dorsal line was compared on postoperative images. Protrusions were observed in three cases (8%) due to excessive correction. Dislocation to the dorsum with elevation of the nasal bone was observed in two cases (5%). In late evaluations, i.e. after 2 years, 17 patients (46%) presented with a palpable graft detected during physical examination.

Figure 8. Preoperative view of patient 1.
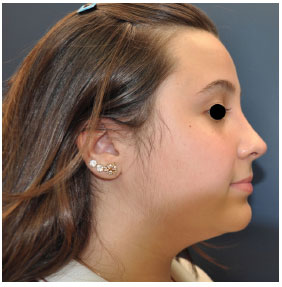
Figure 9. Three-month postoperative view of patient 1.
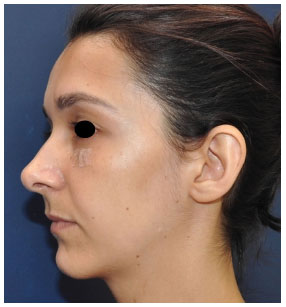
Figure 10. Preoperative view of patient 2.
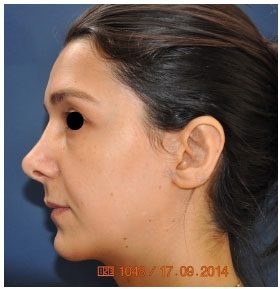
Figure 11. Two-year postoperative view of patient 2.

Figure 12. Preoperative view of patient 3.

Figure 13. Two-year postoperative view of patient 3.
All patients were satisfied with the outcome in the early and late postoperative periods.
DISCUSSION
Historically, the most commonly used grafts were prepared from whole cartilage and were known as onlay grafts. However, the use of diced cartilage has been extensively documented, including its broader application as published by Peer7,8. Its use in the rhinoplasty procedure increased after the publication by Erol of the Turkish Delight9, who proposed the use of Surgicel-wrapped diced cartilage to decrease cartilage perceptibility and concomitantly enable external shaping when used in the nasal dorsum.
Daniel and Calvert published their experience with Turkish Delight of unsatisfactory results and graft resorption4. They used a similar diced cartilage graft as used in our study, covered by the temporal fascia, and applied a graft without external wrapping to obtain satisfactory results and positive clinical outcomes5.
In a histological analysis performed by Brenner et al.10, Surgicel-wrapped diced cartilage resulted in an inflammatory response and subsequent absorption when implanted in rats10.
In a new study conducted by Erol, the use of compressed and diced cartilage (0.5-1.0 mm) without wrapped material to fill areas with syringes developed by the author resulted in complete filling of the prepared pouch. This suggests that the use of non-wrapped cartilage offers a more predictable result than those obtained on using grafts consisting of cartilage only11.
Compared to the studies by Erol and Daniel9, this study used larger diced cartilage pieces (approximately 2 mm instead of 0.5-1 mm), but this did not increase the graft's visibility. In addition, no wrapped grafts were employed, which has the advantages of not using exogenous material such as Surgicel and not causing additional trauma to obtain the temporal fascia.
The method we used to introduce the cartilage in the radix is similar to the technique employed by Gustavo Moreira Costa de Souza12. However, we believe that the free graft may move in other regions as a consequence of small detachments. Therefore, we did not use it in areas other than the radix. The tip of the syringe was cut as described by Daniel & Calvert4. The results observed in our study are in agreement with the findings published by Gustavo Moreira Costa de Souza12. The rate of absorption was not high and no irregularities were observed in the grafted area.
The technical difficulties encountered using a loose graft can be solved by using the following techniques: 1) the area detached should be restricted to the volume to be grafted; 2) the graft should be introduced with the aid of a 1 mL syringe in which the tip has been previously cut; and 3) micro-poring should be performed immediately after graft introduction to shape it and prevent its mobility.
CONCLUSION
The use of a diced cartilage graft as described in this study effectively increased the nasal radix. This graft does not cause deformities and, although onlay grafts are not visible, they can be palpable when consolidated. These grafts do not show clinical impact absorption and can be used safely.
REFERENCES
1. McKinney P, Sweis I. A clinical definition of an ideal nasal radix. Plast Reconstr Surg. 2002;109(4):1416-8, discussion 1419-20. http://dx.doi.org/10.1097/00006534-200204010-00033. PMid:11965001.
2. Sheen JH, Sheen AP. Aesthetic rhinoplasty. 2nd ed. St. Louis: Mosby; 1987.
3. Gunter JP, Landecker A, Cochran CS. Frequently used grafts in rhinoplasty: nomenclature and analysis. Plast Reconstr Surg. 2006;118(1):14e-29e. http://dx.doi.org/10.1097/01.prs.0000221222.15451.fc. PMid:16816668.
4. Daniel RK, Calvert JW. Diced cartilage grafts in rhinoplasty surgery. Plast Reconstr Surg. 2004;113(7):2156-71. http://dx.doi.org/10.1097/01.PRS.0000122544.87086.B9. PMid:15253210.
5. Daniel RK. Diced cartilage grafts in rhinoplasty surgery: current techniques and applications. Plast Reconstr Surg. 2008;122(6):1883-91. http://dx.doi.org/10.1097/PRS.0b013e31818d2104. PMid:19050542.
6. Chang CS, Bergeron L, Chen PK. Diced cartilage rhinoplasty technique for cleft lip patients. Cleft Palate Craniofac J. 2011;48(6):663-9. http://dx.doi.org/10.1597/09-169. PMid:21091138.
7. Peer AL. Diced cartilage grafts. Arch Otolaryngol. 1943;38(2):156-65. http://dx.doi.org/10.1001/archotol.1943.00670040167008.
8. Peer LA. Extended use of diced cartilage grafts. Plast Reconstr Surg. 1954;14(3):178-85. http://dx.doi.org/10.1097/00006534-195409000-00002. PMid:13204206.
9. Erol OO. The Turkish delight: a pliable graft for rhinoplasty. Plast Reconstr Surg. 2000;105(6):2229-41, discussion 2242-3. http://dx.doi.org/10.1097/00006534-200005000-00051. PMid:10839424.
10. Brenner KA, McConnell MP, Evans GR, Calvert JW. Survival of diced cartilage grafts: an experimental study. Plast Reconstr Surg. 2006;117(1):105-15. http://dx.doi.org/10.1097/01.prs.0000195082.38311.f4. PMid:16404256.
11. Erol OO. "Injection" of compressed diced cartilage in the correction of secondary and primary rhinoplasty: a new technique. Plast Reconstr Surg. 2012;130(5S1):44. http://dx.doi.org/10.1097/01.prs.0000421747.61781.dc.
12. Souza GMC, Costa SM, Penna WCNB. Enxerto de cartilagem picada injetável para rinoplastia: método e experiência do Hospital Felício Rocho. Rev Bras Cir Craniomaxilofac. 2012;15(1):17-20.
Departamento de Cirurgia Plástica, Faculdade de Medicina de Catanduva (FAMECA), São Paulo, SP, Brazil
Institution: Study carried out at Serviço de Cirurgia Plástica of the Faculdade de Medicina de Catanduva, São Paulo, SP, Brazil.
Corresponding author:
Manoel Alves Vidal
Faculdade de Medicina de Catanduva
Avenida Orlando Zancaner, 497 - Vila Amendola
Catanduva, SP, Brazil Zip Code 15801-120
E-mail: manoel.a.vidal@gmail.com
Article received: February 4, 2014.
Article accepted: December 13, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter