

Original Article - Year 2014 - Volume 29 -
Depression and wellness in elderly patients with venous ulcers
Depressão e bem-estar em individuo idoso com úlcera venosa
ABSTRACT
INTRODUCTION: Venous ulcers play an important role in patients' lives, as the deformities caused by this type of wound can lead to various adverse effects, including psychosocial disorders.
OBJECTIVE: To evaluate subjective wellness and depression in elderly patients with venous ulcers.
METHODS: This is a primary, descriptive, analytical, and multicenter clinical study involving 55 elderly patients with venous ulcers, undergoing treatment at the Nursing Assistance and Training Center of Clínicas Samuel Libânio Hospital, at the São João Outpatient Clinic of the University of Vale do Sapucaí and at the Primary Healthcare Units of Pouso Alegre city. The study included male and female patients, aged 360 years, and with an ankle-brachial index between 0.8 and 1.0. Data were collected between December 2012 and May 2013, after approval by the research ethics committee of the Faculty of Health Sciences Dr. José Antônio Garcia Coutinho, under recommendation 3.090.46. Sociodemographic data, Yesevage's reduced version of the Geriatric Depression Scale, and the Subjective Wellness Scale were used. Statistical analyses were carried out with the chi-square and Student's t tests.
RESULTS: Most of the study participants were female; 22 (40%) of the patients were aged 60-65 years and 27 (49.10%) were aged 66-70 years. Their income ranged between 1 and 2 minimum wages, and most of them are widowers. Twenty-three (41.82%) elderly patients with venous ulcers had mild to moderate depression levels, and 26 (47.28%) showed severe depression. In the Subjective Wellness Scale, most study participants revealed changes in items 43 (satisfaction with life; 78.20%) and 40 (72.70%).
CONCLUSION: This study revealed that study participants had mild to severe depression and decreased quality of life.
Keywords: Venous ulcer; Leg ulcer; Depression; Quality of life; Elderly.
RESUMO
INTRODUÇÃO: A úlcera venosa assume grande importância na vida dos pacientes, pois a ocorrência de deformidade causada por este tipo de ferida pode gerar consequência advensas as causais inclui distúrbios psicossocial. Avaliar bem-estar subjetivo e depressão em pessoas idosas com úlcera venosa.
MÉTODOS: Estudo clínico, primário, descritivo, analítico e multicêntrico. Participaram 55 indivíduos idosos com úlcera venosa, atendidos no Núcleo de Assistência e Ensino em Enfermagem do Hospital das Clínicas Samuel Libânio, no Ambulatório São João da Universidade do Vale do Sapucaí e nas Unidades Básicas de Saúde da cidade de Pouso Alegre. Foram incluídos pacientes com idade acima de 60 anos, ambos os sexos, índice tornozelo/braço entre 0,8 e 1,0. Os dados foram coletados no período compreendido entre dezembro de 2012 a maio de 2013, após aprovação Comitê de Ética em Pesquisa da Faculdade de Ciências da Saúde Dr. José Antônio Garcia Coutinho sob parecer 3.090.46. Os instrumentos utilizados foram: dado sócio demográfico, Escala de Depressão Geriátrica em versão reduzida de Yesavage e Escala de Bem-estar Subjetivo. Para análise estatística foi realizado os testes: Qui-Quadrado, t de Student.
RESULTADOS: A Maioria, dos indivíduos, era do sexo feminino, 22(40%) tinham entre 60 e 65 anos, 27(49,10%) entre 66 e 70 anos, tinham de 1 a 2 salários mínimos e viúvo. Foram identificados 23 (41,82%) idosos com úlcera venosa nível da depressão leve ou moderada, e 26(47,28%) depressão severa. Relacionado à Escala Bem-estar Subjetivo a maioria dos participantes do estudo apresentaram alteração nos domínios: 43(78,20%), satisfação com a vida, e 40 (72,70%).
CONCLUSÃO: Através deste estudo concluímos que os indivíduos que participaram da pesquisa apresentam depressão entre leve a severa e queda na qualidade de vida. Sentem-se infelizes, e insatisfeitos com a vida.
Palavras-chave: Úlcera venosa; Úlcera de perna; Depressão; Qualidade de vida; Idoso.
Owing to their high incidence among the elderly, venous ulcers are considered a public health problem in Brazil. It is estimated that approximately 1% of the population in developed countries will develop lower-limb ulcers at some stage of life, most of which resulting from problems in the deep venous system, leading to blood accumulation in the lower limbs. Such lesions are also known as stasis or varicose ulcers1,2. Different studies have reported a 0.06-3.6% prevalence of venous ulcers in the worldwide population, involving adults with a history of active or healed ulcers3,4.
Changes in lifestyle in this population directly affects the individuals' well-being, a subjective notion that involves all the essential components of human life that enable performing daily activities: physical, psychological, social, cultural, spiritual, and religious5-7. Such changes may lead to anxiety and depression.
Depression is considered one of the 10 main causes of impairment worldwide, leading to decreased performance at the physical, personal, and social levels. Nevertheless, only a small fraction of persons with depression receive adequate treatment. How individuals identify depression symptoms and their beliefs about its etiology may influence the help-seeking process, treatment compliance, as well as the attitude and behavior of the community toward those having this disease8.
However, depression has often been underdiagnosed and undertreated. Around 50-60% of clinical depression cases go undetected by the clinician. Depressed patients also often receive inadequate and unspecific treatments. Depression-associated morbidity and mortality can, to a large extent (about 70%), be prevented by adequate treatment9.
The presence of a streaming, odorous, painful wound that is difficult to heal limits the possibilities for changes in human life. Family, social, and leisure relations play an important role in recovery, and the absence of these factors may cause the patient to feel desperate and lose faith in the efficacy of treatment, i.e., that the wound will heal10,11.
Thus, venous ulcers play a large role in patients' lives, as the deformities caused by this type of wound can lead to various adverse effects, including psychosocial disorders, compromised quality of life and wellness, and lack of satisfaction toward life and the treatment, which may lead to negative affect.
Several studies have shown that the level of physical and mental health, as well the capacity to function, are reflected on a person's ability to perform the basic tasks of daily life and are critical factors to subjective wellness11. Persons with wounds who experience problems with these factors may tend to isolate themselves from their families and social environment, or deprive themselves of leisure activities12-14.
The study of subjective wellness seeks to understand how people evaluate their own lives, in terms of happiness, satisfaction, state of mind, affects, and quality of life. Therefore, subjective wellness is closely linked to persons with wounds; it is a measure of mental health, as well as a synonym for happiness, adjustment, and social integration; it can also be negatively associated with symptoms of depression and physical disease15-19. Thus, subjective wellness is an important indicator of a person's level of adaptation to society, family, and leisure. Given the scarcity of studies addressing subjective wellness in persons with wounds, the present study was aimed at evaluating subjective wellness and depression in patients with venous ulcers.
METHODS
This is a primary, descriptive, analytical, prospective, and nonrandomized clinical study involving 55 elderly persons with venous ulcer, who were undergoing treatment at the Nursing Assistance and Training Center (NAENF) of Clínicas Samuel Libânio Hospital, at the São João Outpatient Clinic of the University of Vale do Sapucaí and at the Primary Healthcare Units of Pouso Alegre city. For convenience, the sample was selected nonprobabilistically, and patients were included in the order of their arrival to the outpatient clinic. Male and female patients, aged 60 years or above, and with an ankle-brachial index of between 0.8 and 1.0 were recruited. The exclusion criteria were as follows: patients with dementia and/or other disorders preventing them from understanding and answering the questionnaires; patients with arterial/mixed ulcers; and diabetic patients with foot ulcers.
Data were collected between December 2012 and May 2013, after the approval by the research ethics committee of the Faculty of Health Sciences Dr. José Antônio Garcia Coutinho, under recommendation 309046. Data collection was performed by the researchers after the informed consent form was signed by the patients. Two tools were employed in the collection of research data: a questionnaire about demographic data, followed by Yesevage's reduced version of the Geriatric Depression Scale (GDS-15) and the Subjective Wellness Scale.
Yesevage's reduced version of the GDS-15 is a widely used and validated instrument for the diagnosis of depression in elderly patients. It is a test aimed at detecting depression symptoms in elderly persons, and includes 15 negative/affirmative questions, where a score of 5 or higher corresponds to depression and a score of 11 or higher corresponds to severe depression20,21.
The Subjective Wellness Scale is divided in two subscales. Subscale 1 includes components that relate to affection and non-affection emotions. It is made up of items 1 to 47, 21 of which refer to positive affects, and 26 to negative affects. The answer to each item can be 1 (not at all), 2 (a little), 3 (moderately), 4 (a lot), or 5 (extremely). Subscale 2 includes items 48 to 62, which describe the patients' evaluation of their own degree of satisfaction with life. Answers range from 1 to 5, where 1 means "totally disagree," 2 means "disagree," 3 means "don't know," 4 means "agree," and 5 means "totally agree." The final score of each subscale is obtained by adding the scores of the answers to each item, and dividing the result by the total number of items in that subscale. Number 3 corresponds to the median. The Subjective Wellness Scale generates three results that are analyzed independently: positive affects, negative affects, and satisfaction with life. Thus, high scores in subscale 1 (>3) correspond to positive affects; scores <3 correspond to negative affects. Scores >2 in subscale 2 represent satisfaction with life. All subscales display a good level of internal consistency (positive affects: 0.95; negative affects: 0.95; satisfaction with life: 0.9)18,19.
For statistical analyses, we employed the SPSS 11.5 software. The x2 test was used for the sociodemographic variables, and Student's t test was used for the quantitative variables. A 5% significance level was considered. Correlations between two quantitative variables were evaluated by using Pearson's correlation coefficient.
RESULTS
Chi-square test x2
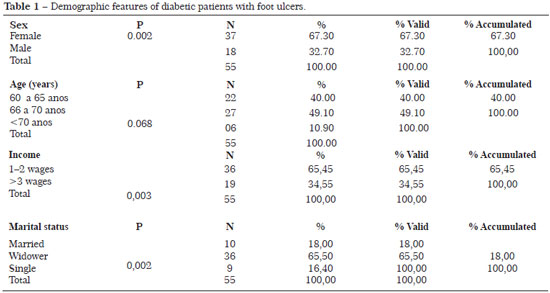
Of the 55 elderly patients with venous ulcers enrolled in the study, most were female; 22 (40%) of the patients were aged 60-65 years and 27 (49.10%) were aged 66-70 years. As shown in Table 1, most of the study participants had an income ranging between 1 and 2 minimum wages, and were widowers.
Student's t test
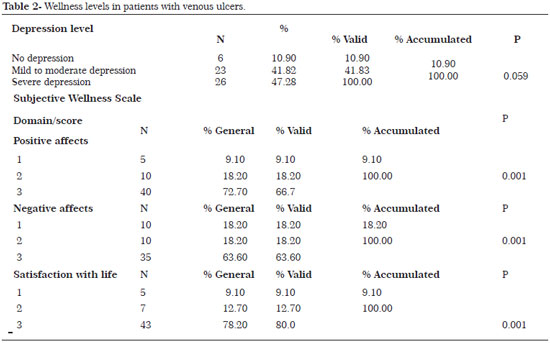
Twenty-three (41.82%) elderly patients with venous ulcers presented mild to moderate depression and 26 (47.28%) presented severe depression. Concerning the Subjective Wellness Scale, most study participants presented altered levels in the following domains: items 43 (satisfaction with life; 78.20%), 40 (positive affects; 72.70%) and 35 (negative affects; 63.60%). These findings indicate that the participants feel unhappy and unsatisfied, with altered positive affects and quality of life, as shown in Table 2.
DISCUSSION
The life expectancy of the Brazilian population has been increasing as a result of the scientific and technological advances in the medical field, as well as of the process of demographic-epidemiologic transition. In the 21st century, the worldwide health standards, including Brazil, are still affected by a wide range of relevant issues. The impacts of scientific and technological developments on the quality of life of the individuals is a matter of concern for the scientific community, concerning not only the effectiveness of therapeutic approaches but also the quality of life and wellness of elderly persons with chronic, degenerative, and nondegenerative conditions22-24.
The present study included 55 elderly patients with venous ulcers. Most of the participants were female; 22 (40%) of the patients were aged 60-65 years and 27 (49.10%) were aged 66-70 years. Most study participants had an income ranging between 1 and 2 minimum wages, and most of them were widowers. These characteristics are in agreement with several previous studies2,5,6,10-15.
Persons with skin lesions, particularly the elderly, must learn to live with their wounds. Depending on the type of lesion, treatment can last up to several months, which may result in impaired mobility and pain. The loss of autonomy and ability to perform various daily activities, such as walking and getting dressed, experienced by most of these individuals, also increase their suffering25. Odorous wounds requiring several changes of dressing per day lead to high costs in treatments and medication, with negative psychological, social, and economic impacts. Often, these factors cause the patients to withdraw from social, leisure, and even family-related activities, which may lead to a decrease in their quality of life, subjective wellness, self-esteem, and self-image26-29.
In the present study, we employed the Subjective Wellness Scale, and the results revealed alterations in various domains (negative affects, positive affects, and satisfaction with life). This indicates that the elderly patients with venous ulcers who participated in the study feel unhappy and unsatisfied, which may lead to their withdrawal from social, leisure, and family activities.
A previous study involving 4253 elderly patients with chronic conditions reported a lack of satisfaction with life among the participants. The existence of a chronic condition led to a significant increase in the feeling of isolation among the elderly interviewed in this study (8.8% vs. 3.5%)30.
Subjective wellness involves individual experiences and concerns the subjective evaluation of the positivity in life. It includes variables such as satisfaction with life and experience of positive affects. Various studies describe personality traits, social support, economic and cultural factors, and life events as the main determinants of subjective wellness31. As such, subjective wellness, also known as happiness32, can also be called stable extroversion, and relates to easy social interactions that enable natural and pleasant relations with other people. Thus, it makes sense to compare happiness and extroversion33.
All physical alterations that can occur may also cause patients to feel unhappy with their lives and to render interactions with other people more difficult, leading to changes in relationships with family and friends34.
Of the three dimensions of subjective wellness, satisfaction with life has the highest predictive value of social support and problem-confronting strategies. Studies from various authors have shown that satisfaction with life is higher in women, in persons with retirement funds, in people who are happy with the support they receive, in those who provide support to others, and in those who face problems directly and are able to reevaluate these problems from a positive perspective. Positive affects also correlate with increasing levels of satisfaction concerning the support received and with direct and relative confrontation, as well as with decreasing levels of avoidance of confrontations17.
Negative affects decrease in the presence of social support; in contrast, they increase with avoidance of confrontations. This constitutes an additional reason why persons with acute or chronic wounds should not be considered simply as passive recipients of help and understanding. The reach of their actions also contributes to their own wellness and satisfaction. Finally, the lower predictive value of social support and confrontation styles on an individual's positive and negative affects suggests that additional variables also play a role in the various dimensions of wellness in patients with lesions, particularly concerning their functional autonomy17,35,36.
Changes in the lifestyle of persons with ulcers directly influence their subjective wellness, which includes all the essential components of human nature: physical, psychological, social, cultural, and spiritual37,11.
A previous study evaluated the feelings of powerlessness and healing expectations in patients with leg ulcers. The study included 40 patients with venous ulcers and 40 diabetic patients with foot ulcers. The study assessed feelings of powerlessness and used Herth's Expectations Scale. The results obtained suggested that diabetic patients with foot ulcers felt powerless, unhappy, unsatisfied, and without hope of wound healing. However, patients with venous ulcers felt powerless, unhappy, and unsatisfied, but remain hopeful that their lesions would heal11.
Finally, any evaluation of subjective wellness must consider the fact that each person applies subjective concepts to the evaluation of their own life and of how events are experienced. These concepts include traits, expectations, beliefs, values, emotions, and previous experiences. Such self-evaluation encompasses thoughts and feelings about individual existence, which, in turn, are the result of a combination of the previously mentioned factors38, and may lead to anxiety and depression.
Twenty-six (47.28%) of the participants in the present study showed severe depression levels, whereas 23 (41.82%) presented mild to moderate depression.
Depression is the most common mental health problem among the elderly. It has a negative impact on all aspects of life and is therefore extremely relevant in terms of public health. Nevertheless, it is still common that elderly persons, their relatives, and even some health-care professionals wrongly attribute symptoms of depression to the normal aging process. Depression among the elderly has significant costs, besides leading to functional decline, familial stress, increased disease risk, slower health recovery rates, and premature death due to suicide or other causes21,39,40.
Worldwide, the prevalence of symptoms of depression among >65 year olds ranges between 10.3% and 13.5%. In Brazil, the prevalence of depression among the elderly ranges from 4.7% to 36.8%41,42.
Symptoms of depression in the elderly are also associated with cognitive and functional deficits, loss or absence of social contacts, widowhood, stressful events, low income, social isolation, lack of social activity, low education levels, and use of medication43; these symptoms may be aggravated by the presence of wounds in elderly persons. Depression is twice as prevalent in women as in men. Additional risk factors, which increase the prevalence of depression up to 5-fold, include the existence of morbidities, a history of depression, recent loss of a partner, and the absence of a partner (single/divorced)44,45.
A study addressing the factorial structure of the 15-item Geriatric Depression Scale among elderly persons enrolled in the Family Health Strategy described the social profile of the participants and analyzed their responses to the various items of the scale. Of the 503 elderly persons who participated in the study, 69.0% were women, 53.1% were illiterate, 53.7% were aged 70 years or older, and 34.4% had depression. The factorial analysis identified four factors (apathy, hopelessness, lack of motivation, and isolation). The structure of the GDS-15 did not allow the generalization of the results obtained. The authors concluded that apathy and isolation are most prevalent among the depressed elderly. It is up to the health-care teams to promote the physical, recreational, and cultural activities required to change this picture. Further research is necessary, particularly for the analysis of the factorial structure46.
A different study investigated the bio-psychosocial factors associated with symptoms of depression among elderly individuals attending a geriatric outpatient clinic in Rio de Janeiro, Brazil. This study showed that approximately 53% of the population showed symptoms of depression. The multivariate analysis revealed a significant association between depression symptoms and the following variables: age, sleep disturbances, mobility and balance, and number of chronic conditions. The authors concluded that age, number of comorbidities, mobility impairment, and balance, are strongly associated with depression in this group of individuals47.
Another study aimed at evaluating the frequency of depressive symptoms in patients with venous ulcers employed the Beck Depression Inventory. The study included 60 individuals, most of whom (91.66%) presented some level of depression. Most participants showed mild to moderate level of symptoms (n = 39; 65%). All levels revealed statistically significant differences. The five most common symptoms were sadness, distorted image of own body, self-deprecation, reduced libido, and social withdrawal. The least represented symptoms were suicidal thoughts and loss of appetite, found in one patient each. Concerning age, 43 patients were 61 years old or older, of whom 38 (88.4%) presented mild to severe depression symptoms5.
Depression is frequently underdiagnosed or even ignored among the elderly, particularly those with chronic conditions, as health-care professionals often see signs of depression as normal manifestations of the aging process48. Nevertheless, the presence of these symptoms may lead to loss of autonomy and worsening of preexisting pathologies. Depression is often associated with enhanced morbidity and mortality risks, leading to an increase in the use of health-care services, neglected self-care, and reduced treatment compliance. Moreover, the existence of comorbidities and the use of high amounts of drugs, as are common among the elderly, increase the complexity of the diagnosis and treatment of depression49.
In view of the necessities that arose in the last few decades due to the observed increase in chronic conditions and the number of patients with wounds, it becomes equally necessary to redirect the academic training and qualification of health-care professionals, valuing not only the content of that training but also the practical aspects of provision of care50,51.
Following this initial contribution to this subject, we suggest that further studies are needed, with larger sample sizes and comparisons between a study group that includes elderly individuals with wounds and a control group of elderly individuals without wounds.
CONCLUSION
The present study showed that the participants of this research had mild to severe depression and a decreased quality of life. They feel unhappy and unsatisfied with life.
REFERENCES
1. Araújo T, Valencia I, Federman DG, Kirsner RS. Managing the patient with venous ulcers. Ann Intern Med. 2003;138(4):326-34.
2. O'Meara S, Cullum NA, Nelson EA. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2009;21(1):CD000265.
3. Reichenberg J, Davis M. Venous ulcers. Semin Cutan Med Surg. 2005;24(4):216-26.
4. Maffei FH, Magaldi C, Pinho SZ, Lastoria S, Pinho W, Yoshida WB, et al. Varicose veins and chronic venous insufficiency in Brazil: prevalence among 1755 inhabitants of a country town. Int J Epidemiol. 1986;15(2):210-7.
5. Salome GM, Blanes L, Ferreira LM. Evaluation of depressive symptoms in patients with venous ulcers. Rev Bras Cir Plást. 2012;27(1):124-29.
6. Salome GM, Ferreira LM. Quality of life in patients with venous ulcers treated with Unna's boot compressive therapy. Rev Bras Cir Plást. 2012;27(3):466-471.
7. Peluso ET, Blay SL. Percepção da depressão pela população da cidade de São Paulo. Rev Saúde Púb. 2008;42(1):41-8.
8. McQuaid JR, Stein MB, Laffaye C, McCahill ME. Depression in a primary care clinic: the prevalence and impact of an unrecognized disorder. J Affect Disord. 1999;55(1):1-10.
9. Finlayson K, Edwards H, Courtney M. The impact of psychosocial factors on adherence to compression therapy to prevent recurrence of venous ulcers. J Clin Nurs. 2010;19(10):1289-97.
10. Salome GM, Pereira VR, Ferreira LM. Spirituality and subjective wellbeing of patients with lower-limb ulceration. J Wound Care. 2013;22(5):230-6.
11. Salomé GM, Alves SG, Costa VF, Pereira VR. Feelings of powerlessness and hope for cure in patients with chronic lower-limb ulcers. J Wound Care. 2013;22(6):300-4.
12. Rabelo DF, Neri AL. Bem-estar subjetivo e senso de ajustamento psicológico em idosos que sofreram acidente vascular cerebral: uma revisão. Estud Psicol (Natal). 2006;11(2):169-77.
13. Salomé GM, Blanes L, Ferreira LM. Assessment of depressive symptoms in people with diabetes mellitus and foot ulcers. Rev Col Bras Cir. 2011;38(5):327-33.
14. Salomé GM, Pellegrino DM, Blanes L, Ferreira LM. Self-esteem in patients with diabetes mellitus and foot ulcers. J Tissue Viab. 2011;20(3):100-6.
15. Salome GM, Espósito, VH. Nursing students experiences while caring people with wounds. Rev Bras Enfermagem. 2008;61(6):822-27.
16. Ferraz RB et al. Happiness: a review. Rev Psiq Clín. 2007;34(5):234-42.
17. Guedea MT, Albuquerque FJ, Tróccoli BT, Noriega JA, Seabra MA, Guedea RL. Relação do bem-estar subjetivo, estratégias de enfrentamento e apoio social em idosos. Psicol Reflex Crit. 2006;19(2):301-8.
18. Albuquerque AS, Tróccoli BT. Desenvolvimento de uma escala de bem-estar subjetivo. Psic Teor Pesq. 2004;20(2):153-64.
19. Panzini RG, Bandeira DR. Escala de Coping Religioso-Espiritual (Escala CRE): elaboração e validação de construto. Rev. Psicol Est. 2005;10(3):507-16.
20. Almeida OP, Almeida SA. Confiabilidade da versão brasileira da Escala de Depressão em Geriatria (GDS) versão reduzida. Arq Neuro-Psiquiatr. 1999;57:421-6.
21. Frank MH, Rodrigues NL. Depressão, ansiedade, outros distúrbios afetivos e suicídio. In: Freitas EV, Py L,Neri AL, et al. Tratado de geriatria e gerontologia. 2ª ed. Rio de Janeiro: Guanabara; 2006. p. 376-87.
22. Salomé GM, Pellegrino DM, Vieira TF, Blanes. Ferreira LL. Sleep quality among patients with venous ulcers: a cross-sectional study in a health care setting in São Paulo, Brazil. Wounds. 2012;24(5):124-31.
23. Salome GM, Donata MS, Blanes L, Ferreira LM. Sleep quality in patients with diabetic foot ulcers. Wounds 2013;25(1):20-7.
24. Nunes JP, Vieira D, Nóbrega WG, Farias TYA, Torres GV. Venous ulcers in patients treated at family health units in Natal, Brazil: prevalence and sociodemographic and health characterization. FIEP Bull. 2008;78(1):338-41.
25. Angélico RC, Oliveira AK, Silva DD, Vasconcelos QL, Costa IK, Torres GV. Perfil sociodemográfico, saúde e clínico de pessoas com úlceras venosas atendidos em um hospital universitário. Rev Wnferm UFPE Online. 2012;6(1):62-8.
26. Saliba OA, Giannini M, Rollo HA. Métodos de diagnóstico não-invasivos para avaliação da insuficiência venosa dos membros inferiores. J Vasc Bras. 2007;6(3):266-75.
27. González-Consuegra RV, Verdú J. Quality of life in people with venous leg ulcers: an integrative review. J Adv Nurs. 2011;67(5):926-44.
28. Silva FA, Freitas CH, Jorge MS, Moreira TM, Alcântara MC. Enfermagem em estomaterapia: cuidados clínicos ao portador de úlcera venosa. Rev Bras Enferm. 2009;62(6):889-93.
29. Bergonse FN, Rivitti EA. Avaliação da circulação arterial pela medida do índice tornozelo/braço em doentes de úlcera venosa crônica. An Bras Dermatol. 2006;81(2):131-5.
30. Broekman BF, Nyunt SZ, Niti M, Jin AZ, Ko SM, Kumar R, et al. Differential item functioning of the Geriatric Depression Scale in an Asian population. J Affect Disord. 2008;108(3):285-90.
31. Woyciekoski C, Stenert F, Hutz CS. Determinantes do Bem-Estar Subjetivo. Psico. 2012;43(3):280-8.
32. Diener E, Seligman, ME. Beyond money: toward an economy of well-being. Psychol Sci Public Interest. 2004;5(1):1-31.
33. Francis, LJ. Happiness is a thing called stable extraversion: a further examination of the relationship between the Oxford Happiness Inventory and Eysenck's dimensional model of personality and gender. Person Individ Diff. 1999;26(1):5-11.
34. Salomé GM, Ferreira LM. Impact of skin grafting of venous leg ulcers on functional status and pain. World J Surg. 2013;37(6):1438-45.
35. Guedea MT, Albuquerque FJ, Tróccol BT, Noriega JA, Seabra MA, Guedea RL. Relação do bem-estar subjetivo, estratégias de enfrentamento e apoio social em idosos. Psicol Reflex Crit. 2006;19(2):301-8.
36. Balsanelli AC, Grossi SA, Herth K. Assessment of hope in patients with chronic illness and their family or caregivers. Acta Paul Enferm. 2011;24(3):354-58.
37. Lopes CR, Figueiredo M, Ávila AM, Soares LM, Dionisio VC. Evaluation of limitations of venous ulcers in legs. J Vasc Bras. 2013;12(1):5-9.
38. Diener E, Lucas RF. Subjective emotional well-being. In M. Lewis, J.M. Haviland. New York: Guilford. 2000. Handbook of Emotions. p. 325-337.
39. Tourigny-Rivard MF, Buchanan D, Cappeliez P, et al. The assessment and treatment of depression. Toronto: Canadian Coalition for Seniors Mental Health; 2006.
40. Gonzalez JS, Safren SA, Delahanty LM, Cagliero E, Wexler DJ, Meigs JB, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med 2008;25(9):1102-7.
41. Blay SL, Bickel H, Cooper, B. Mental illness in cross-national perspective. Results from a Brazilian and German community survey among the elderly. Soc Psychiatr Epidemiol. 1999 [acesso em 2013 Ago 15];26:245-51.
42. Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. 2006;113(5):372-87.
43. Hegadoren K, Norris C, Lasiuk G, da Silva DG, Chivers-Wilson K. The many faces of depression in primary care. Texto Contexto Enferm. 2009;18(1):155-64.
44. Alvarenga MR, Oliveira MA, Faccenda O. Depressive symptoms in the elderly: analysis of the items of the Geriatric Depression Scale. Acta Paul Enferm. 2012;25(4):497-503.
45. Suassuna PD, Veras RP, Lourenço RA, Caldas CP. Factors associated with depressive symptoms in elderly assisted in a Geriatric outpatient clinic. Rev Bras Geriatr Gerontol. 2012;15(4):643-50.
46. Tourigny-Rivard MF, Buchanan D, Cappeliez P, et al. The assessment and treatment of depression. Toronto: Canadian Coalition for Seniors Mental Health; 2006.
47. Conn DK. An approach to detecting and screening depression. Geriatr Ageing. 2005;8(Suppl 8):3-7.
48. Snowdon J. How high in the prevalence of depression in old age? Rev Bras Psiquiatr. 2002;24(Suppl 1):42-7.
49. Rodrigues RA, Scudeller PG, Pedrazzi EC, Schiavetto FV, Lange C. Morbidity and interference in seniors' functional ability. Acta Paul Enferm. 2008;21(4):643-8.
50. Almeida SA et al. Assessment of the quality of life of patients with diabetes mellitus and foot ulcers .Rev. Bras. Cir. Plást. 2013;28(1):142-46.
51. Almeida AS, et al. Depression in patients wit traumatic spinal cord injuries and pressure ulcers. Rev. Bras. Cir. Plást.2013;28(2):282-88.
1. MSc in Nursing - MSc in Bioethics from the University of Vale do Sapucaí, Pouso Alegre/MG, Brazil
2. Nursing Student of the University of Vale do Sapucaí, Pouso Alegre/MG, Brazil
3. Master's Student in Health Applied Sciences of the University of Vale do Sapucaí, Pouso Alegre/MG, Brazil
4. PhD in Health Sciences from the Nursing Post-graduation Program of the Federal University of São Paulo; Lecturer of the Master's Course in Health Applied Sciences of the University of Vale do Sapucaí, Pouso Alegre/MG, Brazil
Institution: University of Vale do Sapucaí.
Corresponding author:
Geraldo Magela Salomé
Avenida Francisco de Paula Quintaninha Ribeiro, 280 - Apto. 134 - Bloco 01 - Jabaquara
São Paulo,SP, Brazil Zip code: 04330-020
E-mail: estomaterapeuta@outlook.com
Article submitted: September 25, 2013.
Article accepted: August 31, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter