

Original Article - Year 2014 - Volume 29 -
Plastic surgery after gastroplasty: nutritional deficiency profile with wound-healing implications
Cirurgia plástica pós-gastroplastia: perfil das deficiências nutricionais com implicações na cicatrização
ABSTRACT
INTRODUCTION: Plastic surgeons have received in their outpatient clinics an increasing number of patients complaining of body contour defects due to the massive weight loss after a bariatric surgery. However, owing to dietary restrictions and surgical desorption, metabolic complications and nutritional disorders are commonly observed in the late postoperative period after gastroplasty. The aim of this study was to determine the prevalence of major nutritional disorders related to healing in patients at a specialized outpatient plastic surgery clinic who underwent gastroplasty.
METHOD: This is an observational, transversal, and descriptive study, in which a laboratory protocol was used to clinically evaluate and assess the patients.
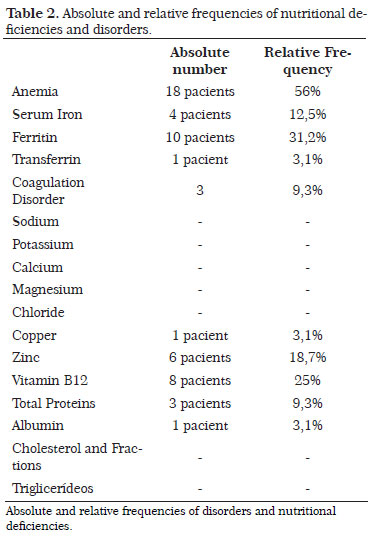
RESULTS: Thirty-two patients who underwent gastroplasty at least 2 years previously with weight stability for at least 6 months were evaluated. The major disorders identified included anemia (56% of patients) and deficiency in iron (31.2%), vitamin B12 (25%), zinc ions (18.7%), and copper (3.1%). Mild deficiencies in the protein profile were also observed; however, no deficiencies in basic and lipid biochemistry were noted.
CONCLUSION: The plastic surgeon should have an in-depth knowledge about the prevalence of the major nutritional disorders related to healing in postbariatric patients, to allow correction of possible deficiencies and prevention of complications. However, more studies would be required to correlate any dietary deficiency to the complications observed in the postoperative period in this group of patients.
Keywords: Gastroplasty; Ex-obese; Bariatric surgery; Plastic surgery.
RESUMO
INTRODUÇÃO: Os cirurgiões plásticos têm recebido em seus consultórios e ambulatórios um número cada vez maior de pacientes com queixa de deformidade do contorno corporal após maciças perdas ponderais secundárias a cirurgias bariátricas. Todavia, em função das restrições alimentares e disabsorções cirúrgicas, são frequentes complicações metabólicas e distúrbios nutricionais no pós-operatório tardio das gastroplastias. O objetivo deste estudo é detectar a prevalência dos principais distúrbios nutricionais relacionados à cicatrização em pacientes de ambulatório especializado em cirurgia plástica do paciente pós-gastroplastia.
MÉTODO: é um estudo observacional, transversal e descritivo, em que os pacientes foram avaliados clinicamente e através de protocolo laboratorial.
RESULTADOS: foram avaliados 32 pacientes com gastroplastia há pelo menos dois anos e estabilidade ponderal há no mínimo seis meses. Os principais distúrbios detectados foram: anemia (56% dos pacientes), com carências na bioquímica do ferro (31,2%) e da vitamina B12 (25%), bem como deficiências dos íons zinco (18,7%) e cobre (3,1%). Houve carências discretas no perfil proteico e ausência de déficits na bioquímica básica e lipidograma.
CONCLUSÃO: é dever do cirurgião plástico conhecer a fundo a prevalência dos principais distúrbios nutricionais relacionados à cicatrização na população de pacientes pós-gastroplastia no sentido de corrigir eventuais carências e prevenir complicações. Sabe-se, contudo, que ainda são necessários mais estudos para correlacionar qualquer deficiência alimentar às intercorrências observadas no pós-operatório deste grupo de pacientes.
Palavras-chave: Gastroplastia; Ex-obeso; Cirurgia bariátrica; Cirurgia plástica.
Plastic surgeons have received in their outpatient clinics an increasing number of patients complaining of body contour defects due to the massive weight loss after a bariatric surgery. This increase is due to the current statistical numbers related to the "obesity" problem. According to the Centers for Disease Control and Prevention (CDC), more than one-third of American adults (35.7%) and approximately 12.5 million children and adolescents (17%) in the United States are obese1. The United States occupies only the 5th position in the obesity ranking according to the World Health Organization, whereas Brazil is already in the 77th position2. Bariatric surgery, which emerged in the 1950s, has significantly improved; it is now considered a fundamental tool for weight loss and improvement of several metabolic disorders such as diabetes mellitus and dyslipidemia. In Brazil, an increase of approximately 200% in the number of bariatric surgeries performed was observed between 2003 and 20113. After a considerable weight loss, the most frequent complaints were tissue sagging and skin changes, affecting mainly the breasts, abdomen, back, arms, thighs, and face4. At this time, the plastic surgeon as part of a multidisciplinary team provides the surgical repair necessary to the affected segments. However, owing to dietary restrictions and surgical desorption, metabolic complications and nutritional disorders are commonly observed in the late postoperative period after gastroplasty; this is also the period during which the patient becomes a candidate for plastic surgery repair procedures. Therefore, the plastic surgeon may encounter complications in this surgery that occur secondary to wound-healing disorders caused by nutritional deficiencies (Figure 1).

Figure 1. Partial dehiscence in abdominoplasty after bariatric surgery.
It is critical for the plastic surgeon to determine the prevalence of major nutritional deficiencies in this group of patients. Anemia, deficits of specific vitamins and minerals, and low protein and lipid reserves may interfere in the different phases of the healing process. On the basis of the high frequency of patients submitted to gastroplasty, we aimed to present a survey on the prevalence of the main nutritional disorders related to healing. The results will alert the plastic surgeon about the necessity for proper preoperative care, and will provide information that could be used to better guide the patients.
OBJECTIVE
We aimed to determine the prevalence of the main nutritional disorders related to healing in patients at a specialized outpatient clinic in plastic surgery who underwent gastroplasty at the plastic surgery department of the Institute of Integral Medicine Prof. Fernando Figueira (IMIP). We also aimed to propose a panel of laboratory tests that can guide the development of preoperative protocols in this group of patients.
METHOD
The study was performed in the plastic surgery outpatient clinic of IMIP between February 2013 and January 2014, with the approval of the research ethics committee of the institution. This is an observational, cross-sectional, and descriptive study. The patients included in the study all underwent gastroplasty at least 2 years presented and had weight stability for at least 6 months. The patients were evaluated from a clinical and laboratory point of view, regardless of whether they were using nutritional supplements. The items evaluated were sex, age, percentage of weight loss, presence of comorbidities, and laboratory parameters (blood count, coagulation, serum iron level, ferritin level, transferrin level, calcium level, sodium level, potassium level, magnesium level, chloride level, vitamin B12 level, total proteins and fractions, lipid profile-total cholesterol level, low-density lipoprotein [LDL] level, high-density lipoprotein [HDL], very low-density lipoprotein [VLDL level], and triglyceride level ).
RESULTS
Thirty-two patients were evaluated in this study, including 31 women and 1 man; all underwent Roux-en-Y gastric bypass. The average age was 38.4 years (range, 23-60 years). The average weight loss was 41.6% of the initial weight, with the higher index being 53% and the lower index being 32%. Approximately 37.5% of the patients (n=12) showed several comorbidities, with systemic arterial hypertension being the most frequent (seven patients), followed by incisional hernias (three patients), and diabetes mellitus, dyslipidemia, osteoarthritis, osteoporosis, and labyrinthitis (one patient each). Of these patients, three among the hypertensive patients and one diabetic patient reported a significant clinical improvement of their respective comorbidities after the bariatric surgery.
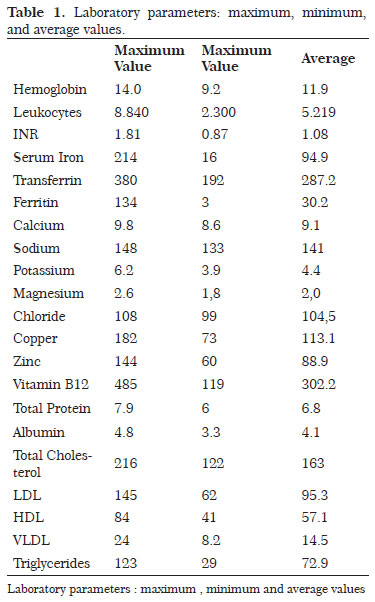
Among laboratory disorders, the most prevalent was anemia, which accounted for 56% (18) of the patients. These patients presented different types of anemia, with microcytic and hypochromic anemia being the most common. The average hemoglobin level was 11.9 g/dL (range, 9-14 g/dL). Seven patients (21.8%) presented with leukopenia. Concerning the coagulation tests, there was approximately a 10% rate of coagulation disorders (three patients), specifically affecting the extrinsic pathway and suggesting that vitamin K and calcium deficiencies are important cofactors of this pathway. This ion deficiency did not appear in any of the patients. The average serum calcium level was 9.1 mg/dL (range, 8.6-9.8 mg/dL). Iron biochemistry appeared frequently altered in the patients included in this study. Serum iron deficiencies were observed in 12.5% (4) of the patients analyzed, and deficiencies in the levels of ferritin in 31.2% (10) of the patients. The average serum iron level was 94.9 µg/dL (range, 16-214 µg/dL); the average ferritin level was 30.2 µg/L (range, 3.0-134 µg/L). Only one patient presented an abnormal transferrin level, with an average of 287 mg/dL (range, 192-380 mg/dL).
No changes in the basic ionograms of sodium, potassium, magnesium, and chloride were observed. The deficiency rate of the other two important ions in the healing process, namely copper and zinc, was low. Copper deficiency was detected in only one patient, whereas zinc deficiency was observed in six patients (18.7%). The average copper level was 113 µg/dL (range, 73-182 µg/dL); the average zinc level was 88.9 µg/dL, with a maximum value of 144 µg/dL and a minimum value of 60 µg/dL. Vitamin B12 level was altered in eight patients (25%), as shown by laboratory tests, with an average value of 302 pg/mL (range, 119-485 pg/mL). The laboratory profile of proteins showed satisfactory results, and presented few and mild deficiencies. The average total protein level was 6.8 g/dL (range, 6.0-7.9 g/dL), with three patients being deficient (9.3%). The average albumin level was 4.1 g/dL (range, 3.3-4.8 g/dL), with one patient being deficient. The lipid profile was normal in all the patients studied. No changes in triglyceride or total cholesterol fractions (LDL, HDL, and VLDL) were observed (Tables 1 and 2).
DISCUSSION
Howes et al.5 had already described the relation between malnutrition and impaired wound healing, as specific nutrients are required at various stages of the complex healing process. According to Andrade et al.6, it is known that patients undergoing bariatric surgery present nutritional and metabolic changes, which require particular attention in the preparation for plastic surgery repair procedures. In the study published by these authors in 2007, the main altered indices were hemoglobin, proteins, serum iron, chromium, and zinc. According to Richards and Schirmer7, the main metabolic complications of Y-en-Roux gastric bypass are iron and vitamin B12 deficiencies, with variation between the series reported. These authors cite that iron deficiency has a prevalence of between 15% and 40%, with iron deficiency anemia occurring in up to 20% of the patients. This deficiency occurs because iron is preferentially absorbed in the diverted intestinal segments, i.e., duodenum and proximal jejunum. Vitamin B12 deficiency is seen in 15-20% of the patients, although it is rarely the cause of anemia or neuropathies. This deficiency occurs owing to a combination of late and intrinsic factors responsible for its absorption. The results of this study corroborate those found in the literature about the elevated prevalence of deficits of these elements. Moreover, according to Richards and Schirmer7, calcium deficiency may occur in up to 8% of patients who undergo gastric bypass, in addition to the deficiency of liposoluble vitamins in different proportions reported in the literature. Calcium and vitamin K, specifically among the liposoluble vitamins, are essential for the coagulation cascade that occurs in the first phase of healing. Moreover, calcium also serves as cofactor for enzymes involved in other steps8.
In our series, there were about 10% of disorders of the extrinsic pathway of the coagulation process, although they were unrelated to calcium deficiencies. Protein-calorie malnutrition is more likely to occur in the recent postoperative period after gastroplasty. However, the late occurrence of protein malnutrition suggests that these patients may always be at a risk for such complications7. Adequate protein intake is essential for the healing process as collagen is the primary component of the scar. Our study identified a low rate of protein deficiencies. When inadequate amounts of lipids are ingested, the healing occurs slowly, and this process is accompanied by the subsequent self-protein consumption for energy generation. Essential fatty acids are also essential for normal healing8. The lipid profile was within the parameters of normality. Concerning the ionogram, it is known that electrolyte balance is essential to maintain homeostasis, and thus the healing process. No change was observed for this parameter, except for copper ions and zinc, which are cofactors of several enzymes involved in the healing process, and as such could compromise cell proliferation and the formation of granulation tissue9.
CONCLUSION
Even with the improvements of bariatric surgery techniques, correct dietary supplementation, and increased access to information, it is common for postbariatric patients to report some nutritional deficiencies to the plastic surgeon. Therefore, a preoperative evaluation is required to investigate, at least, the most frequent disorders found in this study by checking the blood count, coagulation, total proteins and fractions, iron biochemistry, and serum levels of copper, zinc, and vitamin B12. If the surgeon does not feel qualified to handle a certain nutritional deficiency, the support of the multidisciplinary team, involving a nutritionist, endocrinologist, and digestive system surgeon, may be sought10, 11. Fundamental is being with the patient fully compensated before the plastic intervention. In conclusion, despite the already known relation between nutritional deficiencies and healing disorders, more studies would be necessary to correlate any food deficiency with the postoperative complications observed in this group of patients.
REFERENCES
1. Ogden C, Carroll M, Kit B, Flegal K. Prevalence of the Obesity in the United States, 2009/2010. NCHS Data Brief; 2012:82.
2. WHO World Health Organization. Obesity and Overweight, Fact Sheet nº 311. [home page on the internet] Cited March 2013. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.
3. MS Ministério da Saúde. Portal da Saúde SUS: Saúde reduz idade para cirurgia bariátrica no SUS. Ascom [ home page on the internet] Cited october 2012. Available from: http://portalsaude.saude.gov.br/portalsaude/noticia/7663/162/ministerioreduzidademinima%3Cbr%3Eparacirurgiabariatricanosus.html
4. André FS. Cirurgia Plástica após Grande Perda Ponderal. Rev Soc Bras Cir Plast 2010;25(3):532-539.
5. Howes EL, Briggs H, Shea R, et al. Effect of complete and partial Starvation on the Rate of Fibroplasia in the Healing Wound. Arch Surg. 1933;27(5):846-858.
6. Andrade I, Meira A, Ferreira F. Abdominoplastia após a Cirurgia Bariátrica: Aspecto Laboratorial. Rev Soc Bras Cir Plast 2007;22(3):158-161.
7. Richards W, Schirmer B. Sabiston, Tratado de Cirurgia. 18ª Ed. Rio de Janeiro: Elsevier, 2010.
8. Levenson SM, Seifter E. Dysnutrition, Wound Healing and Resistance to Infection. Clin Plast Surg. 1977;4(3):375-88.
9. Fernandez-Madrid F, Prasad AS, Oberleas D. Effect of zinc deficiency on nucleic acids, collagen and noncollagenous protein of the connective tissue. J Lab Clin Med. 1973;82:951-961.
10. Chvapil M. Zinc and wound healing. In Zedeffeldt B (ed): Symposium on Zinc. Lund, Sweden, AB Tika, 1974.
11. Gerk PO. Cirurgia do Contorno Corporal após Grandes Perdas Ponderais. Rev Soc Bras Cir Plast. 2007;22(3):143-152.
12. Furtado IR, Nogueira CH, Júnior EM. Cirurgia Plástica após Gastroplastia Redutora: Planejamento das Cirurgias e Técnicas. Rev Soc Bras Cir Plast 2004;19(2):35-40.
1. Resident Physician at the Plastic Surgery Service of IMIP-PE
2. Titular Member of BSPS - Staff Member at the Plastic Surgery Service of IMIP-PE
3. Titular Member of BSPS - Staff Member at the Plastic Surgery Service of IMIP-PE
4. Resident Physician at the Plastic Surgery Service of IMIP-PE
5. Medical Student at the University of Pernambuco (UPE)
6. Titular Member of BSPS - Regent of the Plastic Surgery Service of IMIP-PE
Institution: Institute of Integral Medicine Prof. Fernando Figueira.
Corresponding author:
Igor Chaves Gomes Luna
Rua Reinaldo Tavares de Melo, 142, Apto 1301 - Manaíra
João Pessoa, PB, Brazil Zip code: 58038-300
E-mail: igorluna_med@hotmail.com
Article submitted: January 8, 2014.
Article accepted: August 31, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter