

Original Article - Year 2014 - Volume 29 -
Breast reconstruction with the transverse rectus abdominis flap: an alternative technique for the closure of abdominal defects
Reconstrução mamária com TRAM: uma técnica alternativa para o fechamento do defeito abdominal
ABSTRACT
INTRODUCTION: The transverse rectus abdominis muscle (TRAM) flap, described by Drever in 1977, was subsequently modified and since then, has rapidly become an important alternative for breast reconstructions. However, bulges and abdominal hernias in the donor area are some of the complications arising from the TRAM flap. This study proposes an alternative technique for the repair of the abdominal defect that minimizes complications and provides better results.
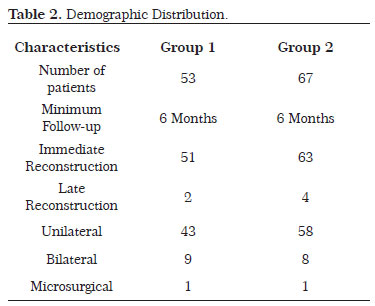
METHOD: The retrospective included 120 women who underwent breast reconstruction with TRAM with placement of an abdominal mesh between May 2003 and November 2012, with follow-up of at least six months. Patients were divided into two groups: Group 1 (53 cases) underwent reconstruction with polypropylene mesh positioned between the aponeurotic layers of the external and internal oblique muscles and Group 2 (67 cases) underwent closure of the arcuate Douglas' line and the remaining lower aponeurosis of the rectus abdominis muscle and reinforcement with mesh.
RESULTS: The patients were evaluated by the same surgeon, according to the same criteria. The rate of bulging was 18.9% in group 1 and 3% in group 2, a statistically significant difference. Bulges and hernias in the hypogastrium varied from 20% to 44% and 12.5% to 20% respectively, when closed primarily. When synthetic mesh was used, these percentages decreased to 1.5% to 6%. The technical improvement and comparison of results aims to minimize such complications.
CONCLUSION: The technique described is advantageous in that, it significantly reduced the occurrence of the most common complication, and increased the aesthetic and functional satisfaction of the patients.
Keywords: Breast reconstruction; Transverse rectus abdominis muscle Flap; Reconstruction of the abdominal wall; Bulging.
RESUMO
INTRODUÇÃO: O retalho do músculo reto abdominal, descrito por Drever em 1977, foi posteriormente modificado e, desde então, se tornou rapidamente uma importante alternativa para reconstrução da mama. Dentre as complicações do TRAM, citam-se os abaulamentos e hérnias abdominais na área doadora. Este estudo vem propor uma técnica alternativa de reparo do defeito abdominal, com o objetivo de minimizar tais inconvenientes e proporcionar melhores resultados.
MÉTODO: O estudo é de caráter retrospectivo, totalizando 120 mulheres submetidas à reconstrução mamária com TRAM com colocação de tela abdominal, e seguimento mínimo de seis meses, entre Maio de 2003 e Novembro de 2012. As pacientes foram divididas em dois grupos: Grupo 1 (53 casos) reconstruídos com tela de polipropileno posicionada entre os folhetos aponeuróticos dos músculos oblíquo externo e interno, e Grupo 2 (67 casos) realizado fechamento da linha arqueada de Douglas e o remanescente inferior da aponeurose do músculo reto abdominal e reforço com tela.
RESULTADOS: As pacientes foram avaliadas pelo mesmo cirurgião, obedecendo aos mesmos critérios. Os resultados obtidos foram 18,9% de abaulamentos no grupo 1 e 3% no grupo 2, estatisticamente significativo. Abaulamentos e hérnias no hipogástrio variam de 20% a 44% e 12,5% a 20% respectivamente, quando fechados primariamente. Quando associado a aplicações de telas sintéticas, esses percentuais diminuem para 1,5% a 6%. O aprimoramento técnico e a comparação de resultados têm a finalidade de minimizar tais complicações.
CONCLUSÃO: A técnica descrita mostra-se vantajosa, pois permitiu significativa diminuição da complicação mais comum, permitindo satisfação estética e funcional das pacientes.
Palavras-chave: Reconstrução mamária; Retalho transverso do músculo reto abdominal; Reconstrução da parede abdominal; abaulamentos.
Drever in 1977 first described the use of a vertical rectus abdominis myocutaneous flap, based on the rectus abdominis muscle for reconstruction of the thoracic and abdominal wall1. Subsequently, in 1979, Robbins described the same vertical flap, but for breast reconstruction 3, which, in 1982, was modified by Hartrampf, followed by Gandolfo and Bentett, who changed it to a transverse orientation, resulting in the transverse rectus abdominis muscle flap (TRAM)1,2,3, which had rapidly become an important alternative for breast reconstruction.
With the development of the TRAM and its large-scale use since the 90s, complications related to the closure of the donor site on the abdominal wall also were identified. Among them, abdominal bulging and hernia have been the major challenges for plastic surgeons, who during the 90s began using synthetic fabrics to reconstruct the abdominal wall after removal of the muscle. The incidence of these complications depends largely on the experience of the surgeon conducting the procedure2,3, but even for a skilled professional, long-term bulging often persists resulting in a drawback in the patient's quality of life. Better knowledge of the anatomy, in particular, that of blood circulation and rectus abdominis muscles, has reduced the incidence of adverse events and complications inherent to this type of breast reconstruction4.
This complication has been further minimized with the development of microsurgical techniques for free TRAM flaps, enabling the preservation of a larger part of the musculature and anterior aponeurosis of the rectus abdominis. However, this method is not always available to all plastic surgery services that routinely perform breast reconstruction, which makes it necessary to develop and improve techniques that can minimize these complications in cases without access to microsurgical techniques.
OBJECTIVE
The objective of this study was to describe a technique to repair abdominal defects that occur during the preparation of the TRAM flap, owing to reinforcing the region's anatomical weakness, in order to reduce the incidence of bulging, which is common to this region; further, this study presents results after the introduction of this new technique on the incidence of this complication compared to the results with the conventional technique used previously.
METHODS
This was a retrospective cohort study, in which breast cancer patients who underwent breast reconstruction with the TRAM flap by a fixed team were assessed. The study was performed from May 2003 to November 2012. The patients were divided into 2 groups on the basis of the technique used for closure of the abdominal wall. The number of patients studied was 134, and these were selected through a review of medical records, excluding those who had no record of the technique used, those who were not operated on by the same team or in whom the technique was different from those included in the study, and those who were inaccessible for long-term follow-up. After these exclusions, the number of patients totaled 120, all of whom were asked to sign a consent Form. This work has not been submitted to the Plataforma Brasil as the initiation date was prior to the creation of this platform.
The first group comprised 53 women who had undergone breast reconstruction with TRAM, in which the abdominal defect was closed by the placing a surgical polypropylene mesh between the aponeurosis of the external oblique and internal oblique muscles, which was then covered by the external oblique muscle aponeurosis. The second group comprised 67 women who had undergone closure of the abdominal defect performed in the same manner as group 1; however, in this group, the region below the arcuate line of the abdomen (Douglas' line) was strengthened before fixing the mesh, because this is a region of anatomical weakness. We joined Douglas' line and the remaining lower part of the aponeurosis of the rectus abdominis muscle with separate absorbable sutures. Later, the closure was performed in the same way as described previously for group 1.
The technique that we propose enables preservation of the inferior portion of the anterior aponeurosis of the rectus abdominis muscle because in this technique, the muscle section was performed at a higher level and was importance to allow coverage of the region. This enabled closure of Douglas' line, which is a highly fragile region where bulging often occurs (Figures 1 to 4).
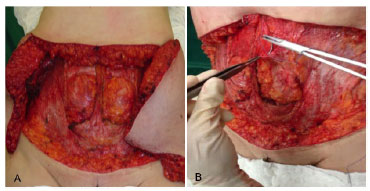
Figura1. Surgical Technique. In A, The defect produced after the TRAM flap was removed. In B, Closure of the remaining lower aponeurosis of the rectus abdominis to Douglas' line.
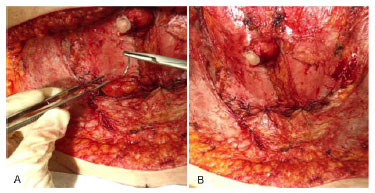
Figure 2. Surgical Technique. In A, Separate stitches with absorbable sutures. In B, full closure between the arcuate Douglas' line and the lower portion of the aponeurosis of the rectus abdominis.
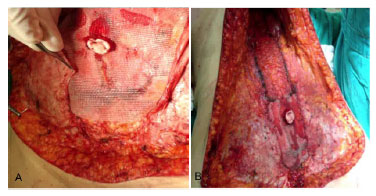
Figure 3. Surgical Technique. In A, the polypropylene mesh is positioned. In B, the mesh is covered with the external oblique muscle aponeurosis.
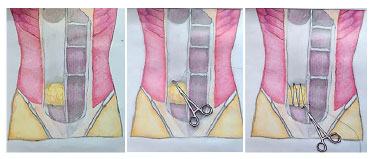
Figure 4. Surgical technique. Schematic drawing showing the defect produced after the completion of the unilateral TRAM and the technique with the closure of the remaining lower aponeurosis below the arcuate Douglas' line.
All patients were operated on by the same surgeon and reassessed weekly in the first month, then every 3 weeks for 3 months, then after 6 months and annually thereafter. During each follow-up, the same criteria were followed for the diagnosis of bulging: physical examination in the supine, dorsal decubitus position, and after Valsalva maneuver, performed by the same surgeon; and comments and complaints made by patients themselves. The difference between bulging and herniation was identified by the absence of a hernial sac. If hernias, a hernial sac is present, with an acute angle between the sac and the abdominal wall, while in bulges, the angle between the bulge and the abdominal wall is obtuse, in addition to the absence of a hernial sac.
Statistical analysis was performed with the assumption that the variable "measure of bulging" showed normality, depending on the type of technique. None of the techniques presented a normal distribution, according to the Kolmogorov-Smirnov and Shapiro-Wilk tests (p<0.05). Thus, the non-parametric Mann Whitney U-test for comparison of two independent groups was performed, because there is no need to specify the distribution of the population from which the sample originates, i.e., this analysis can account for random qualitative or quantitative ordinal variables.
RESULTS
In all, 120 patients who had undergone breast reconstruction with TRAM over a period of 9 years and 6 months were studied (Figure 5): 53 patients in group 1 and 67 patients in group 2. The mean age of the sample was 55.95 years (range 35-83 years) (Table 1).
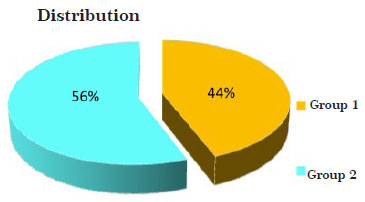
Figure 5. Distribution of the patient groups.
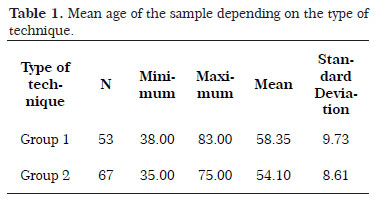
Group 1 comprised 53 women, of whom 43 underwent reconstruction with monopedicled TRAM, 9 with bipedicled TRAM, and 1 with a "turbo-charged" microsurgical TRAM. There were only two cases of late reconstruction; the rest were immediate reconstruction. In group 2 that comprised 67 women, 62 underwent reconstruction with monopedicled TRAM, 8 with bipedicled TRAM, and 1 with microsurgical TRAM. Four cases underwent late reconstruction, and the others, immediate reconstruction (Table 2).
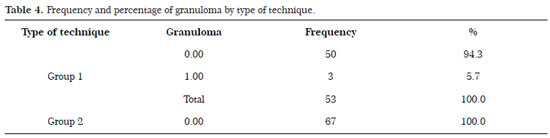
On obtaining data after a minimum follow-up of 1 year and a maximum follow-up of 9 years, with periodic reassessments performed by the same surgeon as described earlier, ten reports of bulging (18.9%) were observed in the first group of patients (53 cases) (Fig. 5 and 6) (Table 3). No other complications related to the mesh were documented in this group. There were three cases of granuloma caused by suture (prolene), which was treated with surgical excision of the suture in two cases, and the third received clinical treatment and did not experience major complications. After the third documented case, there was a change of suture used for fixing of the mesh and mononylon suture replaced the polypropylene used previously, with no further cases of suture granuloma (Table 4). In the second group of patients (67 cases), two cases of bulging were reported (3.0%) (Table 3). No other complications with the mesh or with surgical sutures were reported in the follow-up period (Fig. 7 and 8) (Table 4).
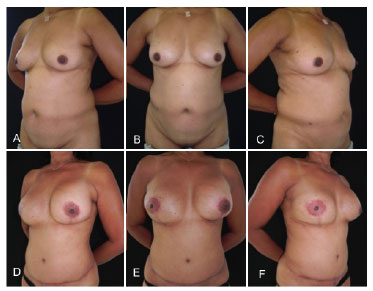
Figure 6. Breast Reconstruction with TRAM, group 2 patient. In A, B and C, pre surgery frontal view and oblique profile. In D, E, and F, front view and oblique profile, postoperative with 6-month follow-up period and absence of bulging.
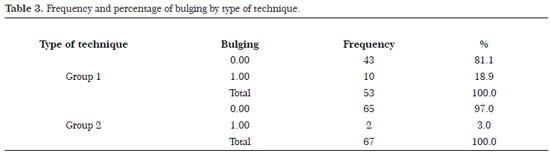

Figure 7. Breast Reconstruction with TRAM, group 1 patient. In A and B, bulging is shown in the left hypogastrium, front view and oblique profile, respectively. In C and D, postoperative aspect after correction of the defect, front view and oblique profile, respectively.

Figure 8. Breast Reconstruction with TRAM, group 1 patient. In A and B, bulging in the right hypogastrium, front view and oblique profile, respectively. In C and D, postoperative aspect after correction of the defect, front view and oblique profile, respectively.
The result of the Mann Whitney test suggested a significant difference between the two techniques (U=1192.50, p=0.015) (Table 5). Figure 10 and Table 3 show lower bulging rates with the new technique (Group 1). Therefore, the new technique is better than the conventional technique (Group 2).
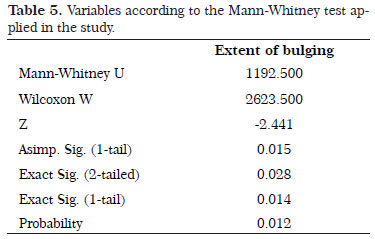

Figure 9. Breast Reconstruction with TRAM, group 2 patient. In A and B, showing absence of bulging in the 1-year postoperative period, front view and oblique profile.
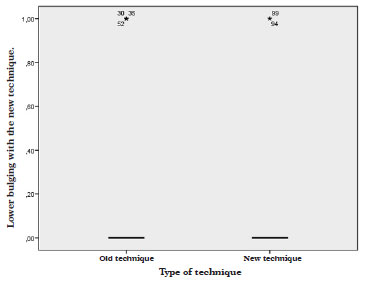
Figure 10. Distribution of results by the type of technique.
DISCUSSION
The rectus abdominis is a long and segmented muscle, between the front faces of the fifth to seventh costal cartilages and xiphoid process that penetrates the pubic symphysis and the body of the pubis. This muscle receives its blood supply from the superior and inferior epigastric arteries, and it is classified as Mathes and Nahai type III, and has between six and ten cutaneous perforators, the majority of which are in the periumbilical region. The rectus abdominis has been used since the mid-1980s for breast reconstructions as a TRAM flap.
The competence of the abdominal wall is one of the main concerns of plastic surgeons who use the TRAM in routine breast reconstructions. Low rates of hernias or bulges, abdominal stability, and low flaccidity are the more important current expectations for successful abdominal closure. Inevitably, reconstruction with a TRAM flap leaves a segmental deficit in the abdominal rectus muscle and exposes the region located below the arcuate Douglas' line, which, historically, is a region of anatomical weakness due to the absence of aponeurotic coverage. There is, therefore, an inherent risk of herniation or bulging if appropriate closure of this defect is not achieved.
For years, the TRAM has been used as the first option for breast reconstruction, and despite the rigorous technique used for placing the prolene mesh, bulging in this area of anatomical weakness has been repeatedly observed.
In 1987, Hartrampf et al reported, in a review of cases, a 1.5% complication rate related to the closure of the abdominal wall without the use of prostheses (mesh) when using a TRAM flap, and noted that this number was associated with the progressive improvement in surgical techniques2,7. However, other authors such as Lallement in 1994 and Suominen in 1996, showed in their studies that the percentage of hernias and bulging of the abdominal region after reconstruction using the TRAM flap, and reported primary closure of the donor site as, respectively, 12.5-20% and 20-44% 2,6-9,12, which is higher than the results published by Hartrampf in 1987, and more similar to both this study and worldwide studies.
Kroll in 1992 showed a 35% decrease in complication rates related to hernias and bulging after primary closure of the abdominal site, and that reduced to 6% by using routine marlex mesh with two suture layers 2,12, which was confirmed soon after by Watterson in 1995, showing a 16% to 4% decrease in complications with the use of polypropylene mesh2,13. While some authors published a 1.5% rate of complications using polypropylene mesh, and 0% with the use of Gore-Tex mesh2,4,10,11. These results are also not confirmed by the world literature.
In our study, in which a total of 120 patients were assessed, the bulging rate was 18.9% using synthetic mesh for abdominal strengthening. The follow-up of these patients revealed a frequent occurrence of bulging always in the same region. This rate was reduced to 3% when we performed the proposed technique, where a rapprochement between the arcuate Douglas' line and the remaining lower aponeurosis of the rectus abdominis muscle was performed, reinforcing the region at risk for bulging.
In the second group, we observed two cases of bulging. In one of the cases, there was a significant increase in body mass index (with a weight increase of >12 kg), which may have contributed to the failure of the method. Currently, we know, being a consensus in the literature, that weight gain is one of the risk factors for the development of bulging14. Thus, this is also a factor considered during the preparation of patients for this type of surgery.
The success achieved using synthetic mesh for closure of the abdominal defect, with regard to the incidence of bulging, recommends that synthetic mesh is the more accepted or more indicated method for this purpose. However, despite its routine use for reconstruction of the abdominal wall, there was an increase in the number of infections in some studies, such as those reported by Kroll and De Marchi, who reported a rate of 11.8%12, and in other studies, that showed an infection rate of 5.8% using the Gore-Tex mesh11 and 1.5% using the polypropylene mesh10. In three studies in which infection was noted at the surgical site, there was the need for a second procedure to remove the mesh. In our study with 120 patients, on the other hand, there were no cases of infection or indications to remove the synthetic mesh.
It is known that bulging and hernias develop in most cases in the lower region of the abdomen due to the absence of the posterior aponeurosis of the rectus abdominis muscle inferior to the arcuate Douglas' line, making this region a point of weakness in the abdominal wall predisposing it to such complications. For this reason, the rapprochement of the arcuate Douglas' line to the remaining lower aponeurosis of the preserved rectus abdominis muscle in its distal insertion after the completion of the pedicled TRAM, closing this anatomical defect, leads to satisfactory results, avoiding the appearance of bulging and restoring the tensile strength of the region.
CONCLUSION
The proposed technique has advantages compared to the other techniques discussed, and may be an important alternative for plastic surgeons in breast reconstructions using the pedicled TRAM flap. The surgical time is extended for no more than 10 minutes; therefore, the patient is not exposed to the risk of a prolonged procedure, and out study did not show any other complications with regard to the new technique.
REFERENCES
1. Bowman CC, Lennox PA, Clugston PA, Courtemanche DJ. Breast reconstruction in older women: Should age be an exclusion criterion? Plast Reconstr Surg. 2006;118(1):16-22.
2. Glasberg SB, D'Amico RA. Use of regenerative human acellular tissue (AlloDerm) to reconstruct the abdominal wall following pedicle TRAM flap breast reconstruction surgery. Plast Reconstr Surg. 2006;118(1):8-15.
3. Kind GM, Rademaker AW, Mustoe TA. Abdominal wall recovery following TRAM flap: A functional outcome study. Plast Reconstr Surg. 1997;99(2):417-28.
4. Keppke E. M. TRAM bipediculado com preservação dos músculos retos do abdomen abaixo da linha arqueda de douglas sem o uso de tela de reforço. Rev Bras Cir Plást. 2012;27(1):49-57.
5. Pennington DG, Lam T. Gore-Tex patch repair or the anterior rectus sheath in free rectus abdominis muscle and myocutaneous flaps. Plast Reconstr Surg. 1996;97(7):1436-40.
6. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69(2):216-25.
7. Hartrampf CR. Breast reconstruction with a transverse abdominal island flap: A retrospective evaluation of 355 patients. Plast Reconstr Surg. 1987;(1):123-127.
8. Lallement M, Missana MC, Bourgeon Y, et al. Closure of the abdominal wall after removal of a myocutaneous flap from the transverse rectus abdominis for breast reconstruction. Apropos of 48 Cases. Review of the literature. Ann Chir Plast Esthet. 1994;39:733.
9. Suominen S, Asko-Seljavaara S, Von Smitten K, et al. Sequelae in the abdominal wall after pedicle or free TRAM flap surgery. Ann Plast Surg. 1996;36:629.
10. Zienowicz RJ, May JW. Hernia prevention and aesthetic contouring of the abdomen following TRAM flap breast reconstruction by use of polypropylene mesh. Plast Reconstr Surg. 1995;96(6):1346-50.
11. Pennington DG, Lam T. Gore-Tex patch repair of the anterior rectus sheath in free rectus abdominis muscle and myocutaneous flap. Plast Reconstr Surg. 1996;97(7):1436-40.
12. Kroll SS, Marchi M. Comparison of strategies for preventing abdominal wall weakness after TRAM flap breast reconstruction. Plast Reconstr Surg. 1992;89(6):1045-51.
13. Watterson PA, Bostwick JIII, Heter JR, et al. TRAM flap anatomy: Correlated with a 10-Year clinical experience with 55 patients. Plast Reconstr Surg. 1995;95(7):1185-94.
14. Rossetto LA, Abla LE, Vidal R, Garcia EB, Gonzalez RJ, Gebrim LH, et al. Factors associated with hernia and bulge formation at the donor site of the pedicled TRAM flap. Eur J Plast Surg. 2010;33(4):203-208.
1. Resident in plastic surgery, Aspiring Member of the SBCP - Resident at the Plastic Surgery Service, Hospital Daher Lago Sul, Brasília, DF, Brazil
2. Plastic Surgeon, Full Member of the SBCP - Preceptor of the Plastic Surgery Service, Hospital Daher Lago Sul, Brasília, DF, Brazil
3. Plastic Surgeon Full Member of the SBCP - Regent of the Plastic Surgery Service, Hospital Daher Lago Sul, Brasília, DF, Brazil
4. Resident in plastic surgery, Aspiring Member of the SBCP - Resident at the Plastic Surgery Service, Hospital Daher Lago Sul, Brasília, DF, Brazil
5. Resident in plastic surgery Aspiring Member of the SBCP - Resident at the Plastic Surgery Service, Hospital Daher Lago Sul, Brasília, DF, Brazil
6. Resident in plastic surgery, Aspiring Member of the SBCP - Resident at the Plastic Surgery Service, Hospital Daher Lago Sul, Brasília, DF, Brazil
7. Resident in plastic surgery, Aspiring Member of the SBCP - Resident at the Plastic Surgery Service, Hospital Daher South Lake, Brasilia, DF, Brazil
8. Residente de cirurgia plástica, Membro aspirante da SBCP - Residente do Serviço de Cirurgia Plástica do Hospital Daher Lago Sul, Brasília, DF
Institution: Plastic Surgery Service, Hospital Daher Lago Sul (HDLS), Brasília, DF, Brazil.
Corresponding Author:
Conrado Miranda de Almeida
Centro de Estudos do Hospital Daher Lago Sul, SHIS QI 7 - Conjunto F - Lago Sul
Brasília, DF, Brazil. Zip code: 71615-570
E-mail: conradoma@hotmail.com
Article submitted: January 23, 2014.
Article accepted: November 25, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter