

Original Article - Year 2014 - Volume 29 -
Breast reduction with the lower pedicle technique: an observational study
Mamoplastia redutora pela técnica de pedículo inferior: estudo descritivo
ABSTRACT
INTRODUCTION: Reduction mammaplasty with the inferior pedicle nipple-areolar technique is widely used in North America but not in Brazil. Its main advantage lies in maintaining the sensitivity of the areola in large mammary ptoses. To describe the preoperative and postoperative characteristics of patients who underwent reduction mammaplasty with the inferior pedicle nipple-areolar technique at the Santa Casa de Campo Grande - MS in 2013.
METHOD: We performed interview, physical examination, and review of medical records of patients operated by using this technique at this institution in 2013.
RESULTS: Forty patients were evaluated. Their ages ranged from 21 to 68 years, with a mean of 40.62 years. The comorbidities reported were hypertension, diabetes, ulcerative colitis, disc herniation, and anxiety disorder. The average weight of resected tissue was 600.6 g from the right breast and 609.6 g from the left breast. The most common presurgery complaint was low back pain, followed by shoulder pain. The most frequent complications in the early postoperative phase were dehiscence of the mid-point of the strand (10%) and hematoma (5%). The predominant type of anesthesia was general anesthesia. All patients showed benign breast dysplasia in the postoperative histopathological examination.
CONCLUSION: The inferior pedicle nipple-areolar technique was adequate for the treatment of major hypertrophies and mammary ptoses.
Keywords: Breast cancer; Plastic surgery; Reduction mammaplasty; Blood irrigation.
RESUMO
INTRODUÇÃO: A mamoplastia redutora utilizando pedículo inferior incluindo complexo aréolopapilar é muito utilizada na América do Norte, mas pouco difundida no Brasil. Sua principal vantagem é a utilização em grandes ptoses mamárias, mantendo a sensibilidade da aréola.
OBJETIVO: O objetivo é descrever as características pré e pós-operatórias de pacientes submetidos a mamoplastia redutora pela técnica do pedículo inferior areolado na Santa Casa de Campo Grande - MS em 2013.
MÉTODO: Entrevista, exame físico e dados de prontuário das pacientes operadas por esta técnica nessa instituição no ano de 2013.
RESULTADOS: Foram avaliadas 40 pacientes, sendo que a idade variou de 21 a 68 anos, com média de 40,62 anos. As comorbidades relatadas foram hipertensão arterial sistêmica, diabetes, retocolite ulcerativa, hérnia de disco e distúrbio de ansiedade. O peso médio de tecido mamário ressecado foi 600,6g na mama direita e 609,6g na mama esquerda. Dentre as queixas pré-operatória, a mais comum foi a lombalgia, seguida por dor nos ombros. As mais frequentes complicações no pós-operatório recente foram a deiscência do ponto médio da vertente (10%) e o hematoma (5%).O tipo de Anestesia predominante foi a anestesia geral. Todas as pacientes apresentaram displasias benignas da mama nos histopatológicos de pós-operatórios.
CONCLUSÃO: A técnica do pedículo inferior areolado mostrou-se adequada para o tratamento de grandes hipertrofias e ptoses mamárias.
Palavras-chave: Mama; Cirurgia plástica; Mamoplastia redutora; Irrigação sanguínea.
Reduction mammaplasty with the inferior pedicle, which includes the nipple-areola complex (NAC), continues to be widely used in North America; however, the technique is still little known in Brazil1. Many reports in the international literature have proven the safety of the technique, the reproducibility of the results, the absence of major complications even in larger resections, and, mainly, the advantage of its use in large ptoses, when considering amputation of the breast with a free nipple-areola graft, in addition to the important preservation of the NAC sensitivity2,3. Hypertrophies and mammary ptoses can cause physical and emotional distress to patients. The objectives of mammaplasty are to reduce the size of the breasts, reposition the NAC, reshape the breast parenchyma, improve the position of the upper pole, adjust the skin envelope to the breast volume, and achieve lasting results.
OBJECTIVE
To describe the preoperative and postoperative characteristics of 40 patients who underwent breast reduction with the inferior pedicle nipple-areolar technique, at the Santa Casa de Misericórdia de Campo Grande - MS, in 2013.
METHOD
This work was a prospective, observational study performed through interview and physical examination of patients operated at the plastic surgery service of the Hospital Santa Casa de Misericordia de Campo Grande - MS in 2013.
Forty women who underwent reduction mammaplasty with the inferior pedicle nipple-areolar technique were evaluated. The following data were collected: age, origin, weight removed from each breast, comorbidities, preoperative complaints of excessive breasts, recent postoperative complications, hospitalization time, type of anesthesia, histopathological examination, profession, and deaths. All patients were operated by second- or third-year residents of the plastic surgery service with the aid of tutors. All patients signed an informed consent form concerning the use of their images. This work was not submitted to a research ethics committee because the institution does not have one; however, a declaration of the department responsible for authorizing the implementation of the study is available.
Surgical Technique
Initially described by several authors since the mid-1970s, this technique was modified by Georgiade et al. in 1989. Marking of the skin is routinely performed with the patient in the sitting position; guide lines are drawn from the manubrium of the sternum to the xiphoid process and the midclavicular line to the midpoint of the submammary fold, passing through the areola. Initially, point A is marked, which corresponds to the projection above the areola of the midpoint of the submammary fold and coincides with the midline of the arm; then, the AB and AC arms of the flap, forming a 90º angle between them and extends from 7 to 9 cm, according to the evaluation performed with bidigital clamping, are also marked. The excess subcutaneous tissue to be resected is marked without extending beyond the anatomical limits of the breast (Figure 1).
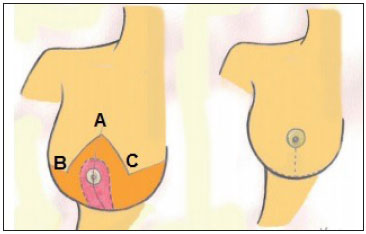
Figure 1. Marking points of the areolar inferior pedicle technique.
The surgery begins with the patient in the supine position and under anesthesia. The epithelization of the inferior pedicle is performed with an extension of 6-10cm at the base and thickness of at least 5-6cm, extending to overcome the NAC at 4-5cm. The detached dermoglandular flaps must have a minimum thickness of 2cm, and the upper pole of these flaps is kept as thick as possible to prevent flattening of the upper pole of the breast.
After the resection of the lateral (mainly) and medial excess tissue of the mammary gland, the pedicle is fixed to the fascia of the greater pectoral muscle with absorbable suture to prevent lateralization. Sutures joining the dermoglandular flaps are placed, and the new site of the NAC is marked, with its transposition done naturally and without tension. Absorbable Vycril 3-0 is used for the suture, in two layers, and the skin suture is done with Monocryl 4-0. The technique proceeds with placement of a Penrose drain, exteriorized through the surgical incision.
The drain is removed on day 2 after surgery, at the time of hospital discharge. The external sutures are removed on the 14th postoperative day. Consultations are held weekly until the 30th postoperative day, and then at 3, 6, 12, and 24 months postoperatively.
RESULTS
The age of the patients ranged from 21 to 68 years, with a mean of 40.62 years (Figure 2).
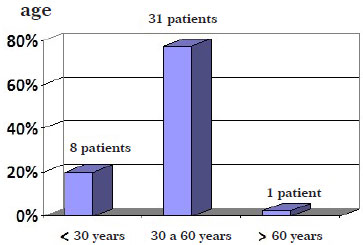
Figure 2. Graph showing the patients> age.
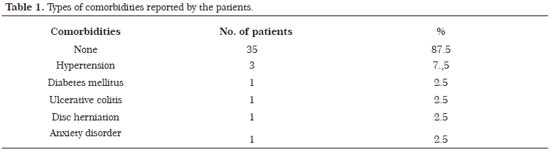
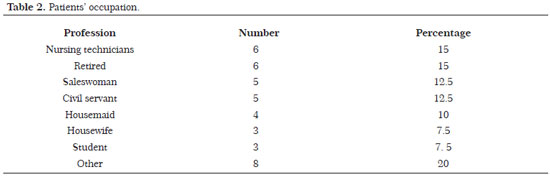
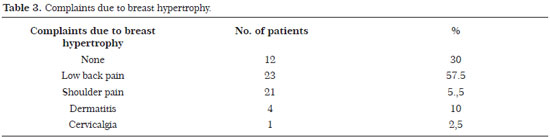
Concerning their origin, 35 of the patients were living in the city of Campo Grande - MS, and only 5 were living in the state of Mato Grosso do Sul. All patients were subjected to reduction mammaplasty with the inferior pedicle nipple-areolar technique. The comorbidities reported were hypertension, diabetes, ulcerative colitis, disc herniation, and anxiety disorder (Table 1). No patient reported a previous bariatric surgery. Concerning the predominant occupation, six patients were nursing technicians and six were retired (Table 2).
The weight of the resected breast tissue ranged from 195 to 1260 g in the right breast, with an average weight of 600.6 g, and from 140 to 1700 g in the left breast, with an average weight of 609.6 g (Figure 3).
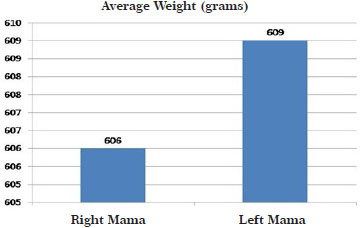
Figure 3. Graphical representation of the mean weight of the resected breast tissue.
All patients showed benign breast dysplasia in the postoperative histopathological examinations. There were no deaths in this study.
DISCUSSION
The search for more satisfactory (adequate volume, suspension, and shape of the breast) and lasting breast reconstructions has led to the proposal of several reduction mammaplasty techniques. In this regard, the pedicle, which is responsible for the vascular supply of the NAC, has received great attention. However, tissue changes associated with the influence of gravity over time changes the location of the anatomical structures. This breast sagging phenomenon is always expected to a greater or lesser degree after a reduction mammaplasty; however, to date, it has not been studied objectively4. The inferior pedicled flap was described in 1975, in Brazil, by Liacyr Ribeiro et al.5, who, in 2002, presented their experience with this technique performed in 2000 patients. The authors reported five types of flap variation in a 30-year period. In their results, they observed a reduction of the sagging effect, projection, a more harmonious shape, and longer-lasting results.
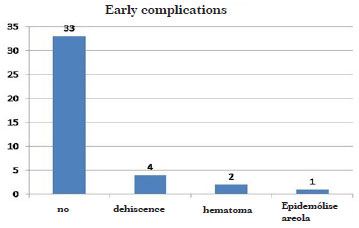
Figure 4. Graphical representation of the complications encountered.
Jalma Jurado6, at the 12th Brazilian Congress of Plastic Surgery in 1976, presented his work of transposing the NAC through a deepithelized dermoglandular inferior areolar flap, resulting in an inverted T scar. Robbins7, in 1977, used an inferior dermal areolar pedicle technique, with the objective of assessing the viability and sensitivity of the NAC. The author noted that the sensitivity of the NAC was maintained, and repositioning of the areola occurred without tension and without distortion of the pedicle. In addition, the technique allowed the possibility of excising a large amount of breast tissue. Courtiss and Goldwyn8, in 1977, reported the results of the same technique in 24 breast reduction mammaplasties, in a 2.5-year period, as an alternative to the use of a free nipple and areola graft in large breast reductions. They noted the advantages of maintenance of the sensitivity, contour, pigmentation, and erection of the nipple, even in cases of gigantomastia or serious ptoses. Georgiade et al.2, in 1989, presented modifications to the inferior pedicle technique, by using a wide-based pyramidal breast parenchyma with a dermal flap including the NAC. They used this technique in 1001 breast reductions, in a 12-year interval, and recommended the maintenance of a thin layer of breast stroma on the greater pectoral muscle to allow better preservation of NAC sensitivity.
Calderon Ortega et al.9, in 1992, performed an anatomical and clinical study about the origin of the vascularization of the inferior pedicle, showing that it has an axial origin from branches of the internal mammary artery (emerging from the fourth and fifth intercostal space). They reported the ease of ascension of the NAC to the new position, even in large mammary ptoses.
Mandrekas et al.10, in 1996, performed a retrospective study on 371 operated patients to assess early and late surgical complications. They concluded that the inferior pedicle technique was reliable, even in the reduction of breasts with varying sizes, with preservation of the sensitivity of the nipple and the potential of breast-feeding. Wallace et al.11, in 1998, discussed the postoperative results, rates of complications, and level of patient satisfaction. O
According to the literature, the inferior pedicled flap is feasible for breasts of different shapes and sizes, with reproducible results. Moreover, it can be used without increasing the duration of surgery, in addition to being an alternative to the free nipple-graft technique. Despite the criticism from some authors that the use of the inferior pedicle technique results in breasts without projection, this can be avoided by leaving an areolar flap with greater volume at its central portion associated with a greater thickness of the superior dermocutaneous flap, providing an adequate size and projection of the breasts, without altering the resected volume15.
CONCLUSION
Most of the patients in this study were in their fourth decade of life and had a complaint of lower back pain. There was a need for excision of >500 g of tissue from each breast. The patients presented a good postoperative evolution and were satisfied with the results of the surgery. The inferior pedicle technique was adequate for the treatment of major hypertrophies and mammary ptoses.
REFERENCES
1. Rohrich RJ, Gosman AA, Brown SA, Tonadapu P, Foster B. Current preferences for breast reduction techniques: a survey of board-certified plastic surgeons 2002. Plast Reconstr Surg. 2004;114(7):1724-36.
2. Georgiade GS, Riefkohl RE, Georgiade NG. The inferior dermal-pyramidal type breast reduction: long-term evaluation. Ann Plast Surg. 1989;23(3):203-11.
3. Scott GR, Carson CL, Borah GL. Maximizing outcomes in breast reduction surgery: a review of 518 consecutive patients. Plast Reconstr Surg. 2005;116(6):1633-41.
4. Pérez-Macias JM. Long-lasting evolution of ptosis control after reduction mammaplasty using the hammock technique. Aesthetic Plast Surg. 2007;31(3):266-74.
5. Ribeiro L, Accorsi A Jr, Buss A, Marcal-Pessoa M. Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Reconstr Surg. 2002;110(3):960-70.
6. Jurado J. Plásticas mamárias de redução baseadas em retalho dérmico vertical monopediculado. Anais XII Congresso Brasileiro de Cirurgia Plástica 1976;29.
7. Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59(1):64-7.
8. Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique: an alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59(4):500-7.
9. Calderon Ortega W, Arriagada Stuven J, Godoy Silanes M, Gomes SL. Anatomia y clinica de las mamoplastias de reducción según técnica del pedículo inferior. Rev Chil Cir. 1992;44(4):437-41.
10. Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas DA. Reduction mammaplasty with the inferior pedicle technique: early and late complications in 371 patients. Br J Plast Surg. 1996;49(7):442-6.
11. Wallace WH, Thompson WO, Smith RA, Barraza KR, Davidson SF, Thompson JT 2nd. Reduction mammaplasty using the inferior pedicle technique. Ann Plast Surg. 1998;40(3):235-40.
12. O'Grady KF, Thoma A, Dal Cin A. A comparison of complication rates in large and small inferior pedicle reduction mammaplasty. Plast Reconstr Surg. 2005;115(3):736-42.
13. Zambacos GJ, Mandrekas AD. Complication rates in inferior pedicle reduction mammaplasty. Plast Reconstr Surg. 2006;118(1):274-6.
14. Hunter JG, Ceydeli A. Correlation between complication rate and tissue resection volume in inferior pedicle reduction mammaplasty: a retrospective study. Aesthetic Surg J. 2006;26(2):153-6.
15. Nahabedian MY, Mofid MM. Viability and sensation of the nipple-areolar complex after reduction mammaplasty. Ann Plast Surg. 2002;49(1):24-32.
1. Second-year Resident in Plastic Surgery of the Santa Casa Misericórdia de Campo Grande - MS
2. Full Member of the Brazilian Society of Plastic Surgery and the Brazilian Society of Hyperbaric Medicine
3. Full Member of the Brazilian Society of Plastic Surgery
4. First-year Resident in Plastic Surgery, Santa Casa Misericórdia de Campo Grande - MS
5. Third-year Resident in Plastic Surgery, Santa Casa Misericórdia de Campo Grande - MS
6. Third-year Resident in Plastic Surgery, Santa Casa Misericórdia de Campo Grande - MS
7. Second-year Resident in Plastic Surgery, Santa Casa Misericórdia de Campo Grande - MS
Institution: Santa Casa de Misericordia de Campo Grande - MS.
Corresponding Author:
Elson Taveira Adorno Filho
Rua São Paulo, 661 - Ed Manhhattan - Apto 901 - Bairro Monte Castelo
Campo Grande, MS, Brazil Zip code: 79010-050
E-mail: elsonadorno@hotmail.com
Article submitted: January 26, 2014.
Article accepted: December 13, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter