

Original Article - Year 2014 - Volume 29 -
Analysis of Basal Cell Carcinoma Treatment
Análise do Tratamento do Carcinoma Basocelular
ABSTRACT
INTRODUCTION: Skin cancer is the most common neoplasm in the Brazilian population. It most frequently presents on the face, causing functional and aesthetic morbidity in patients. Its treatment consists in resection of the lesion while preserving the skin's function with the least possible deformity. The most common skin cancer is basal cell carcinoma (BCC), representing 70-80% of all cases.
METHODS: We retrospectively evaluated 73 patients with 95 BCCs from March 2010 to May 2012. The following characteristics were analyzed: age, sex, skin color, comorbidities, sun exposure, prior dermatological consultation, lesion site, lesion size, clinical type, histological type, reconstruction type, surgical complications, surgical margins, management of compromised surgical margins, anatomical pathology after reintervention, recurrence, and appearance of another primary lesion in the same patient.
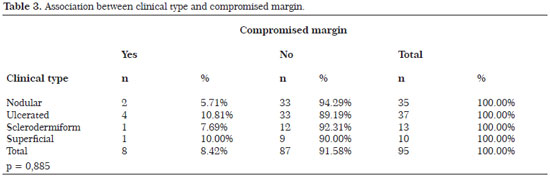
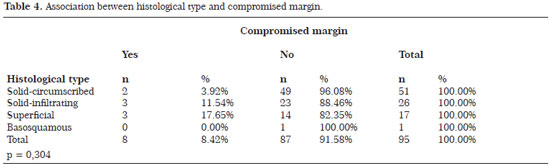
RESULTS: The mean age of the patients was 60.73 years. Female patients accounted for 56.16%. Sun exposure was reported in 73.97% of patients. The mean lesion size was 0.91 cm, and the most common lesion site was the face (71.58%). A local flap was used in 54.74% of cases. Circumscribed solid BCC was the most common type. Compromised margins occurred in 8.42% of cases, demonstrating a relation between lesions >2 cm and the nose but without statistical significance.
CONCLUSION: The plastic surgeon plays an important role in the treatment of BCC, aiming to perform resection following oncological principles, repair the affected area, and maintain the skin's functionality with the least possible cosmetic alterations.
Keywords: Carcinoma; Therapy; Skin; Epidemiology; Cutaneous neoplasms.
RESUMO
INTRODUÇÃO: O câncer de pele na população brasileira é a neoplasia mais comum. Localiza-se com mais frequência na face, causando morbidade tanto funcional quanto estética aos pacientes. O tratamento consiste na ressecção oncológica da lesão, preservando a função com a menor deformidade possível. O câncer de pele mais comum é o carcinoma basocelular (CBC), correspondendo entre 70-80% dos casos.
MÉTODO: Avaliamos retrospectivamente 73 pacientes com 95 carcinomas basocelulares no período de março de 2010 a maio de 2012. Foram analisados os seguintes critérios: idade, sexo, cor, comorbidades, exposição solar, presença de consulta prévia com dermatologia, localização da lesão, tamanho da lesão, tipo clínico, tipo histológico, tipo de reconstrução, complicações cirúrgicas, margem cirúrgicas, conduta na margem cirúrgica comprometida, anatomopatológico após reintervenção, presença de recidiva e aparecimento de outra lesão primária no mesmo paciente.
RESULTADOS: A idade média foi de 60,73 anos. O sexo feminino correspondeu a 56,16%. A Exposição solar foi referida em 73,97% dos casos. O tamanho médio da lesão foi 0,91 cm. O local mais frequente foi a face (71,58%). O retalho local foi utilizado em 54,74% dos casos. O CBC sólido circunscrito foi o mais frequente. As margens comprometidas ocorreram em 8,42% dos casos, demonstrando relação com lesões maiores de 2cm e com o nariz sem significância estatística.
CONCLUSÃO: No tratamento do carcinoma basocelular é importante a participação do cirurgião plástico, objetivando a ressecção sob princípios oncológicos, realizando a reparação da área afetada, a manutenção funcional e a menor alteração estética possível.
Palavras-chave: Carcinoma; Terapêutica; Pele; Epidemiologia; Neoplasias cutâneas.
Skin cancer is the most common neoplasm in the Brazilian population. According to the National Cancer Institute, an estimated 62,680 new cases of nonmelanoma skin cancer among men and 71,490 in women were recorded in 20121. Skin cancer most often presents on the face, causing both functional and aesthetic morbidity that result in reduced self-esteem in patients2. The treatment aims of oncologic resection of the lesion are to preserve the skin's function and cause the least possible deformity3.
The most common skin cancer is basal cell carcinoma (BCC), representing from 70% to 80% of all cases4,5. The most common type of BCC is the nodular type. The risk factors for the development of BCC are as follows: Fitzpatrick skin type I and II6, old age, history of sun exposure, a previous nonmelanoma skin cancer, presence of actinic keratosis, xeroderma pigmentosum, and Gorlin-Goltz syndrome6,7. In the literature, a higher frequency was found in men; however, some studies showed a higher frequency in women4,8.
The most common treatment is surgical resection with a safe margin. The margin advocated in the literature is between 3 and 4 mm for circumscribed lesions, such as the nodular form and lesions with a size of <2 cm, and between 5 and 6 mm for tumors with poorly defined margins, such as superficial and infiltrating forms, or those with a size of >2 cm4,5,9. In the literature, the rate of compromised margins ranges from 4% to 18%, and the management of positive margins is controversial as only one-third of patients have residual disease at reoperation6,10-14.
OBJECTIVE
The objective of this work is to study the treatment of BCC, by analyzing the clinical, histological, and therapeutic profile of patients in a series of cases seen by the author during a period of 2 years.
METHOD
Files of patients operated for BCC at the Plastic Surgery Clinic Reference Center Afonso Celso Liberato, municipality of Itajaí-SC, and at the private practice of the author, from March 2010 to May 2012, were reviewed retrospectively.
The inclusion criteria were: 1) a diagnosis of BCC, 2) patients operated by the author, and 3) complete outpatient follow-up up to 6 months after surgery. The exclusion criteria were: 1) incomplete data in the medical record and 2) patients who underwent the surgical procedure but were absent for the follow-up.
The following characteristics were analyzed: age, sex, skin color, comorbidities, sun exposure, prior dermatological consultation, lesion site, lesion size, clinical type, histological type, reconstruction type, surgical complications, surgical margin, conduct in surgical safety margin, pathology after reintervention, recurrence, and appearance of another primary lesion in the same patient.
One hundred eight patients were operated during this period; by applying the inclusion and exclusion criteria, 95 lesions in 73 patients were selected. Of these 73 patients, 71 were from the reference center and two were from the private practice. The evaluated patients were operated at the day surgery unit of the reference center, under a local anesthetic (lidocaine) at the maximum limit of 50% of the allowable dose. The reference center has a day surgery unit. The patients from the private practice underwent the procedure at a private hospital in the region.
The surgical margins adopted were 4 mm for tumors <2 cm with defined margins, and 6 mm for tumors >2 cm and/or with poorly defined margins. The principal treatment of positive margins was surgical enlargement.
For classification purposes, the BCCs were classified clinically into nodular, ulcerated, superficial, and sclerodermiform types as in Bariani5 and Quintas15. The histological type was classified as either solid-circumscribed, solid-infiltrative, metatypical or basosquamous, superficial or multicentric, or sclerodermiform. In terms of diameter, the lesions were divided into the following categories: ≤1 cm, 1.1-2 cm, and >2 cm15.
To analyze the variables of compromised surgical margins, the chi-square test was used. A significance level of 5% (p < 0.05) was adopted. Because this study was a retrospective study of patients operated by the author, it was not submitted to the ethics committee.
RESULTS
The mean age of patients was 60.73 years, and 50.68% were in the age group of 60-80 years. The total patients ranged in age between 29 and 83 years. The distribution of patients by sex was 56.16% female and 43.84% male. The postoperative follow-up duration was a mean of 12.3 months (range, 6-19 months). All patients studied were white (Fitzpatrick phototype I and II). Concerning the patient's comorbidities, 19.18% had hypertension and 13.70% had diabetes mellitus. Sun exposure was reported in 73.97%, and patients in the farming and fishing profession accounted for 40.74%.
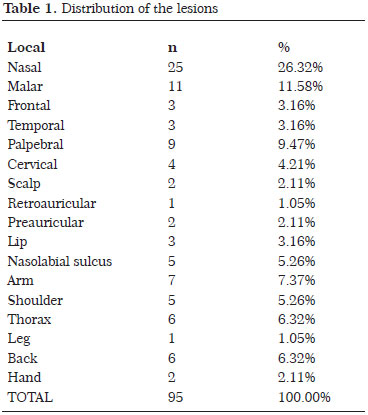
The operated patients had a previous biopsy and a referral by a dermatologist in 43.84% of cases. The average lesion size was 0.91 cm (range, 0.2-3.5 cm). There were 1.33 lesions per patient. Of the operated patients, 13.70% had a second primary lesion diagnosed, occurring at 7.5 months after the first surgery, on average. In 71.58% of the patients, the most common lesion site was the face. Table 1 shows the distribution of lesions according to location.
The distribution of clinical types was nodular in 36.84% (n = 35), ulcerated in 38.95% (n = 37), sclerodermiform in 13.68% (n = 13), and superficial in 10.53% (n = 10).
The distribution of histological types was solid-circumscribed in 53.68% (n = 51), solid-infiltrating in 27.37% (n = 26), superficial or multicenter in 17.89% (n = 17), and basosquamous in 1.05% (n = 1). The type of reconstruction used in patients was local flap in 54.74%, primary closure in 40%, and skin autograft in 5.26%. The most commonly used flap was the bilobed flap (30.91%). Figures 1 (A-C), 2 (A-F), and 3 (A-E) show the types of reconstruction used.

Figure 1. (A) Preoperative image of an 81-year-old female patient. (B). Intraoperative image showing the skin graft on the nasal tip. (C). Postoperative image at 4 months. Pathological examination showed free surgical margins.
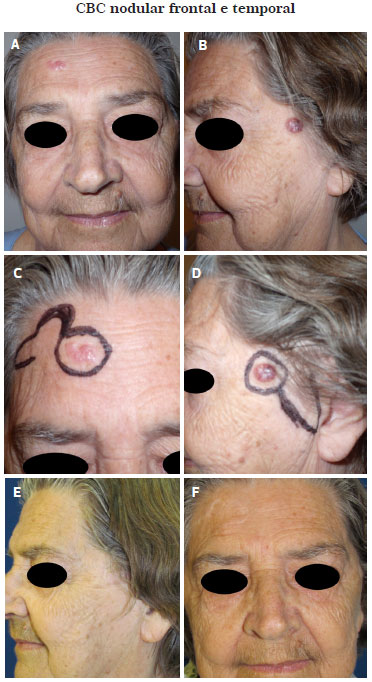
Figure 2. (A). Preoperative image of a 69-year-old female patient with lesion in the frontal region. (B). Preoperative image of a 69-year-old female patient with a lesion in the temporal region. (C). Preoperative markup of the bilobed flap for repair. (D). Preoperative markup of the preauricular rotation flap for repair. (E). Postoperative image at 1 year. Pathological examination showed free surgical margins. (F). Postoperative image at 1 year. Pathological examination showed free surgical margins.
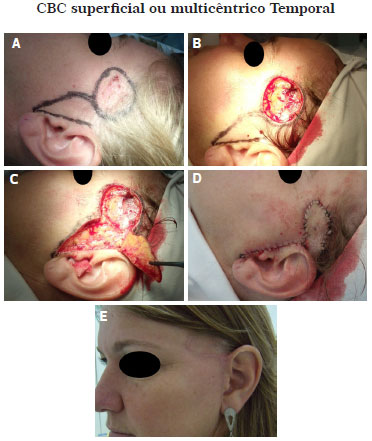
Figure 3 (A). Preoperative image of a 36-year-old female patient showing the markup of the preauricular flap rotation. (B). Resected lesion. (C). Flap rotation. (D). The flap was moved and sutured into the defect site. (E). Postoperative image at 6 months. Pathological examination showed free surgical margins.
Initial complications occurred in seven patients (7.37%), with the most frequent complication being partial flap necrosis in three patients (5.77% of flaps). There were two cases of wound infection and two cases of partial dehiscence of the suture. Late complications occurred in five patients (5.26%), with an unaesthetic scar as the most common complication (three patients), followed by flap edema (one patient), and excess skin in the rotation area (one patient). Figure 4 (A-D) shows some of the postoperative complications.

Figure 4 (A). Persistent edema in the bilobed flap. Lymphatic drainage and local massage was performed, improving the edema without surgical intervention. (B). Local infection and dehiscence of the suture. The patient was submitted to antibiotic therapy and to local dressings with antibiotic ointments, leading to improvement of the infection and wound healing by secondary intention. This patient is diabetic. (C). Necrosis of the bilobed flap. Local dressing of the wound and healing by secondary intention was chosen. (D). Results of healing of the necrosis by secondary intention. To refine the reconstruction, a second operation was proposed. The patient was already satisfied with the result and declined the second procedure.
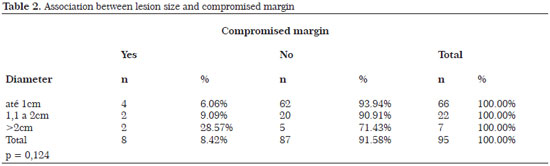
Tables 2 to 5 show some variables related to the surgical margin, with the corresponding levels of statistical significance. In BCCs with compromised margins, 87.50% were located on the face, of which 71.43% were found in the nasal region.
Histopathological examination revealed compromised margins in 8.42% of patients, in which the lateral margin was the most often affected (62.50%). The adjacent skin showed actinic keratosis in 27.37% of the excised BCCs. The management consisted of extension of the surgical margin in seven patients (87.50%) and clinical follow-up in one patient (12.50%). The patient who received clinical follow-up showed a compromised lateral margin, for which enlargement of the margin was proposed. However, because of the patient's age (82 years), the family preferred clinical monitoring. No recurrence has occurred after 12 months.
In lesions for which surgical enlargement was performed (six lesions [85.71%]), the pathological examination revealed no residual tumor. Only one case of enlargement was positive for neoplasia, and it was possible to achieve free surgical margins in a second procedure. No recurrence of cancer was observed in the patients during the study period.
DISCUSSION
BCC occurs more frequently in persons older than 60 years, as shown by the results of previous studies16-18. The literature shows that it presents more frequently in men with a history of sun exposure and professions that involve exposure to the sun (e.g., farming)7,8,15,19. In our study, we observed BCC more frequently in women, as did Nasser6,9. There was a higher frequency of BCC in patients with Fitzpatrick skin type I and II5,7. Our patients consisted of Caucasians, probably because of the large number of descendants of European immigrants in the Itajai Valley region.
The average lesion size was smaller than that reported in the literature5,20. This is probably because early diagnosis and referral from the dermatologist allowed us to treat lesions with a smaller diameter, and almost half of our patients had previously been evaluated by a dermatologist. We work together with four dermatologists at our reference center both for early detection and patient follow-up in case of recurrence or new primary lesions.
Patients with BCC are likely to have new BCC, and our rate was compatible with that of Bariani5. Quintas15 states that in the scientific literature, the head is most the commonly affected region, with the nose being the most frequent location12,15. The nodular/ulcerated BCC is the most common type5,12,15, and there may be variations according to the nomenclature used for the classification of these neoplasms15. The presence of actinic keratosis demonstrates the skin damage caused by prolonged exposure to the sun5.
The surgical margin in the literature varies between 1 and 10mm, with an average of 4-6mm. Moreover, a surgical margin of 3-4mm is recommended for lesions <2cm with well-defined margins, such as the nodular type, and 5-6mm for lesions >2cm and with ill-defined margins, such as superficial and sclerodermiform types12,20.
In this study, local flaps were used for the reconstruction of the defect after the resection of the BCC, followed by primary closure. Depending on the topography of the defect, the most appropriate reconstruction must be used, aiming for a better functional and aesthetic results6,17,21.
The bilobed flap was the most frequently used flap for the reconstructions, as it is a versatile flap that can be applied in various anatomical sites, allowing for various forms of reconstruction21. In this study, the surgical complications were more frequent than that observed by Veríssimo6.
The rate of involvement of surgical margins in our study is in agreement with that reported in the literature, which ranges from 5% to 25%11,15. The lateral margin was the most compromised in our study, and we chose to enlarge the margins in most cases6,15. The management of positive margins is not uniform in the literature; however, there is a greater tendency for surgeons to enlarge the margins. According to the literature, the tumor invasion of the surgical margins leads to the recurrence of, on average, 30% of BCC. However, the literature also shows that in the enlargements carried out, only one-third of patients showed residual disease12. We propose conservative treatment for compromised margins and clinical follow-up, especially for patients with a higher surgical risk6,12.
No recurrence was observed during the study period. In this study, we adopted a minimum follow-up duration of 6 months, with one case followed for up to 19 months. According to the literature, the recurrence rate can reach 14%6. A longer clinical follow-up of our patients should show the recurrence rate.
The diameter of the lesion, clinical type, histological type, and topography in relation to surgical margin were found to have no statistical significance in this study. Nasal and periorbital areas, lesions >2 cm, and the superficial and sclerodermiform types are more likely to have positive margins12. The lack of statistical significance is probably due to the number of cases studied. A larger sample might show significance.
CONCLUSION
The present study showed a higher frequency of BCC in women older than 60 years and with a history of sun exposure. The face was the most affected site. Solid-circumscribed BCC was the most frequent lesion observed. Compromised margins occurred in 8.42% of cases, showing a relation between lesions >2cm and the nasal region but with no statistical significance. The most common type of reconstruction was with the local flap.
In the treatment of BCC, the surgeon plays an important role, aiming to perform resection following oncological principles, repair the affected area, and maintain the skin's functionality with the least possible cosmetic alterations.
REFERENCES
1. Brasil. Ministério da Saúde. Instituto Nacional do Câncer. Estimativa 2012: Incidência do Câncer no Brasil. Disponível em: http://www.inca.gov.br.
2. Carvalho MP, Filho RS, Gomes HC, Veiga DF, Juliano Y, Ferreira LM. Auto-Estima em Pacientes com Carcinomas de Pele. Rev Col Bras. Cir. 2007;34(6):361-6.
3. Feijó MJ, Santana HW, Viana H. Machado AA, Pereira RMR. Uma Análise retrospectiva dos pacientes com tumoração em face sugestiva de câncer de pele submetidos a tratamento cirúrgico no IMIP. Rev Bras Cir Plást. 2010;25(suppl):39.
4. Bariani RL, Nahas FX, Barbosa MVJ, Farah AB, Ferreira LM. Basal cell carcinoma: an updated epidemiological and therapeutically profile of an urban population. Acta Cir Bras. 2006 Mar-Apr;21(2):66-73.
5. Veríssimo P, Barbosa MVJ. Tratamento cirúrgico dos tumores de pele nasal em idosos. Rev Bras Cir Plást. 2009;24(2l):219-33.
6. Maia M, Proença NG, Moraes JC. Risk factors for basal cell carcinoma: a case-control study. Rev Saúde Púb. 1995;29(1):27-37.
7. Chinem VP, Miot há. Epidemiology of basal cell carcinoma. An Bras Dermatol. 2011;86(2):292-305.
8. Nasser N. Epidemiologia dos carcinomas basocelulares em Blumenau, SC, Brasil, de 1980 a 1999. An Bras Dermatol. 2005;80(4):363-8.
9. Mélega J. Cirurgia Plástica Fundamentos e Arte: Princípios Gerais Rio de Janeiro: Medsi; 2002.
10. Su Y, Giorlando F, Ek EW, Dieu T. Incomplete excision of basal cell carcinoma: a prospective trial. Plast Reconstr Surg. 2007;120(5):1240-8.
11. Gregorio TCR, Sbalchiero JC, Leal, PRA. Acompanhamento a longo prazo de carcinomas basocelulares com margens comprometidas. Rev Soc Bras Cir Plást. 2005;20(1):8-11.
12. Eliezri YD, Cohen PR. Cancer recurrence following Mohs micrographic surgery: a mechanism of tumor persistence. Plast Reconstr Surg. 1992;90(1):121-5.
13. Holmikvist K, Rogers G, Dahl PA. Incidence of residual basal cell carcinoma in patients who appear free after biopsy. J Am Acad Dermatol. 2002;46(4):549-53.
14. Quintas RCS, Coutinho ALF. Fatores de risco para o comprometimento de margens cirúrgicas nas ressecções de carcinomas basocelular. Rev Bras Cir Plást. 2008;23(2):116-9.
15. Sbalchiero JC, Gregorio TCR, Leitão L, Leal, PRA, Dibe MJA. Conduta na reconstrução da Ponta Nasal no tratamento das neoplasias cutâneas. Rev Soc Bras Cir Plást. 2005;20(1):12-6.
16. Gallo JRB, Monteiro, EHF, Rossi RHP, Bicudo FPS, Seba JLV, Zuanazzi, GM, Alves RM, et al. Impacto da implantação do intituto do câncer no tratamento das neoplasias de pele na região noroeste paulista. Rev Bras Cir Plást. 2009;24(3):362-7.
17. Chedid R, Borges KS, Santos P, Sbalchiero JC, Dibe MA, Leal PR. Perfil das reconstruções de pálpebra inferior no Instituto Nacional do Câncer: estudo retrospectivo de 137 casos.
18. Sociedade Brasileira de Cirurgia Plástica. Cirurgia Plástica. São Paulo: Atheneu; 2005.
19. Gulleth Y, Goldberg N, Silverman RP, Gastman BR. What is the best surgical margin for a basal cell carcinoma: a meta-analysis of the literature. Plast Reconstr Surg. 2010;126(4):1222-31.
20. Tissiani LAL, Alonso N, Carneiro MH, Bazzi K, Rocco M. Versatilidade do retalho bilobado. Rev Bras Cir Plást. 2011;26(3):411-7.
1. Plastic Surgeon - Senior Member of the Brazilian Society of Plastic Surgery
2. Medical Student at the Universidade do Vale do Itajaí - UNIVALI - Medical Student
3. Medical Student at the Universidade do Vale do Itajaí - UNIVALI - Medical Student
Institution: Clinic of Plastic Surgery - Centro de Referência São Judas - Municipality of Itajaí-SC and private practice of the author.
Corresponding author:
Eduardo Wiethorn Rodrigues
Rua Lauro Muller, 757 - Bairro Fazenda
Itajai, SC, Brazil Zip code: 88301-401
E-mail: eduardorodriguesplastica@gmail.com
Article Submitted: June 23, 2012.
Article Accepted: November 9, 2014.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter