

Ideas and Innovation - Year 2014 - Volume 29 -
Prognosis of frontal region video surgery with a modified fixation technique
Prognóstico da videocirurgia da região frontal com técnica modificada de fixação
ABSTRACT
INTRODUCTION: Video endoscopy has become a procedure of choice for the treatment of eyebrow ptosis and forehead wrinkles. This minimally invasive technique has several advantages over traditional coronal incision. Several fixation methods are reported in the literature, with similar results. In this study, we describe direct needle fixation.
OBJECTIVE: To evaluate the prognosis of video endoscopic surgery using a direct needle technique.
METHOD: Computerized photographic evaluations of 37 patients undergoing video endoscopy of the frontal region with needle direct fixation were conducted in two private hospitals in the city of Porto Alegre in Rio Grande do Sul, Brazil.
RESULTS: The mean eyebrow elevations were 5.7 and 4.4 mm in the lateral and middle third measurements. After a small dip in elevation in the first month after surgery, the repositioning of the eyebrow remained unchanged in subsequent measurements up to 24 months later.
CONCLUSION: Direct needle fixation produced lasting, reliable, and reproducible results during the period in which measurements were made.
Keywords: Video Endoscopy; Eyebrow; Fixation; Periosteum; Case Series; Prognosis.
RESUMO
INTRODUÇÃO: A videoendoscopia tem se estabelecido como procedimento de escolha no tratamento da ptose do supercílio e das rugas da região frontal. O acesso minimamente invasivo produz vantagens em relação à tradicional incisão coronal. Diversos métodos de fixação são relatados na literatura, apresentando resultados semelhantes. Nesta série de casos, descrevemos a fixação direta com agulha.
OBJETIVO: Avaliar o prognóstico da videocirurgia, utilizando-se a técnica direta com agulha.
MÉTODO: Avaliação fotográfica computadorizada de 37 pacientes submetidos à videoendoscopia da região frontal com a fixação direta com agulha, realizada em dois hospitais privados na cidade de Porto Alegre-RS. Resultados: A elevação média do supercílio foi de 5,7 mm no terço lateral e de 4,4 mm no terço medial. Após um pequeno descenso da elevação, no primeiro mês pós-operatório, o reposicionamento do supercílio permaneceu inalterado nas medidas subsequentes até 24 meses.
CONCLUSÃO: A fixação direta com agulha é capaz de produzir resultados duráveis, seguros e reprodutíveis no período em que foram realizadas as medições.
Palavras-chave: Videoendoscopia; Supercílio; Fixação; Periósteo; Série de Casos; Prognóstico.
Facial video endoscopic surgery has become a procedure of choice for the treatment of eyebrow ptosis and forehead wrinkles. This minimally invasive approach offers reduced scarring and quick recovery, in contrast to the traditional coronal incision method. Nerve and scar changes resulting from open access do not seem to justify its broad use1-3. Standardization of the video endoscopic method has proven to be a durable and reproducible solution when certain principles are followed, such as suitable detachment, wide mobilization, and fixation of tissues in their new position2,4. The literature has shown that various fixation methods produce good and comparable results5-7. We performed direct fixation with a needle8, which in our experience produces adequate results, requiring little preparation time and offering low operating cost. This report discusses the application and the experience of the authors after a series of cases using the direct needle fixation technique, and evaluates long-term outcomes.
METHOD
A total of 37 patients who underwent video surgery of the frontal region were enrolled from June 2009 to July 2011, and medical records and pre- and postoperative photographs were reviewed, following research protocol. A computer analysis of photographs was performed using Mirror medical imaging software, version 6.0 (Canfield Imaging Systems, Inc., Fairfield, NJ, USA). Measurements were made 1, 6, 12, and 24 months after the procedure (Table 1). In the photographic assessment, we measured two points (Figure 1): A. From the pupil to the body of eyebrow (PU-BOE - middle third) and B. Between the external corner of the eye and eyebrow tail (EC-ET - lateral third). All patients underwent fixation with needle and thread using the double "V" technique after subperiosteal detachment. The results were subjected to statistical analysis using Student t and chi-square tests with 95% confidence intervals.
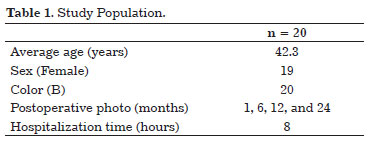

Figure 1. Measurements: (A) From the pupil to the body of the eyebrow (PU-BOE) and (B) from the external corner of the eye and eyebrow tail (EC-ET).
The double "V" fixation technique
Casagrande8 first described this technique, which involves direct fixation of tissue using a needle developed by the authors. The needle is similar to a Reverdaim needle, is malleable, and has the hole closest to the end.
The needle is introduced percutaneously in the vector of desired elevation, and an endoscope used to evaluate the grasp of the periosteum that must be mobilized in the tissue group. After the needle reaches the exterior through one of the incisions, a nylon 3.0 monofilament is passed through the hole at the end of the needle, returning to conduct a small dermal route, which serves as a fixed point of traction when the needle externalizes again.
The authors of this study used a double "V" in the frontal region, which functions as a three-pulley system (two dermal passages and a suture among traction cables in the midline incision) with two fixed points on the temporal muscle aponeurosis (Figure 2).

Figure 2. Technique proposed by the authors: a double "V" in the frontal region.
RESULTS
Of the patients included in this study, 95% were female Caucasians with a mean age of 44.2 years (+/- 4.3 years). They underwent video endoscopy of the upper third of their faces (Table 1). The average eyebrow elevation was 5.7 mm (+/- 0.8 mm) in the lateral third and 4.4 mm (+/- 0.4 mm) in the middle third. Of the four postoperative measurements, the eyebrow elevation at the second measurement (6 months after the procedure) had declined compared to the first measurement (1 month after surgery). The average ptosis was 1.4 mm (P < 0.05). This motion stabilized in later measurements 6, 12, and 24 months after surgery, with no statistically significant differences between them (P > 0.05).
DISCUSSION
Numerous methods such as external compressive dressings, glue, sutures, screws, and absorbable and nonabsorbable microplates have been proposed for tissue fixation after subperiosteal detachment9. Their access methods also varied, including intraosseous tunnels, incisions for tissue advancement and resection, and sutures along deeper structures such as the galea and temporal9,10 muscle aponeurosis.
The diversity of proposed materials must conform to the basic principles governing the endoscopic approach: limited inconvenience and postoperative complications, reduced trauma, low cost, and rapid implementation.
We believe that needle direct fixation follows all these principles. It is probably the fastest and cheapest option of all other proposed methods. Its implementation is simple and requires only the previously described needle and nylon8,11 wire.
Of course, broad and correct release and mobilization of tissues as well as treatment of eyebrow musculature depression are essential for obtaining good results and durability6,8,10,11. Maneuvers such as periosteum incisions near the superior orbital ridge and dermal detachment in the procerus muscles, corrugators, and parts of the orbicularis (group of eyebrow depressant muscles) are part of the proposed technical arsenal.
The maintenance of the results
There was a small drop in eyebrow elevation measurements in this study between 1 and 6 months after surgery. This downward trend had stabilized in subsequent follow-ups (12 and 24 months) (Figure 3). These observations suggest that the initial decline may be related to a loss of tensile strength of the Mononylon 3.0 suture while there is no fixation and the complete periosteal healing, preventing the progression of decline. These findings suggest that external fixation, regardless of method, should work, maintaining the elevation while the tissue heals in its new position. Experimental studies by Romo12 suggested that this type of complete fixation requires around 6 weeks in animal models.

Figure 3. Stabilization of eyebrow descent 12 and 24 months after surgery.
CONCLUSION
Tissue dissection, mobilization, and fixation are primary cofactors required for good results using this surgical technique. All of these steps work together to ensure that the results are more aesthetically pleasing and durable. Direct needle fixation and the modifications proposed here are an applicable and capable assemblage to produce lasting, reliable, and reproducible results during the observation period (Figures 4 and 5).

Figure 4. Results 12 months after performing the technique described by the authors.

Figure 5. Results 6 months after performing the technique described by the authors.
REFERENCES
1. Knize DM. Anatomic concepts for brow lift procedures. Plast Reconstr Surg. 2009;124(6):2118-26. http://dx.doi.org/10.1097/PRS.0b013e3181bd0726. PMid:19952669
2. Rohrich RJ, Beran SJ. Evolving fixation methods in endoscopically assisted forehead rejuvenation: controversies and rationale. Plast Reconstr Surg. 1997;100(6):1575-84. http://dx.doi.org/10.1097/00006534-199711000-00032. PMid:9385975
3. Sozer O, Biggs TM. Our experience with endoscopic brow lifts. Aesthetic Plast Surg. 2000;24(2):90-6. http://dx.doi.org/10.1007/s002660010017. PMid:10833231
4. Troilius C. Subperiosteal brow lifts without fixation. Plast Reconstr Surg. 2004;114(6):1595-16045. http://dx.doi.org/10.1097/01.PRS.0000138758.48043.44. PMid:15509955
5. Jones BM, Grover R. Endoscopic brow lift: a personal review of 538 patients and comparison of fixation techniques. Plast Reconstr Surg. 2004;113(4):1242-52. http://dx.doi.org/10.1097/01.PRS.0000110206.25586.78. PMid:15083028
6. Graf RM, Tolazzi AR, Mansur AE, Teixeira V. Endoscopic periosteal brow lift: evaluation and follow-up of eyebrow height. Plast Reconstr Surg. 2008;121(2):609-19. http://dx.doi.org/10.1097/01.prs.0000298111.56163.3b. PMid:18300981
7. Gruber RP, Nahai F. Brow or forehead fixation with sutures only: a preliminary communication. Aesthetic Plast Surg. 2003;27(5):403-5. http://dx.doi.org/10.1007/s00266-003-3020-3. PMid:14648063
8. Casagrande C, Saltz R, Chem R, Pinto R, Collares MV. Direct Needle Fixation in Endoscopic Facial Rejuvenation. Aesthet Surg J. 2000;20(5):361-7.
9. Foustanos A, Zavrides H. An alternative fixation technique for the endoscopic brow lift. Ann Plast Surg. 2006;56(6):599-604. http://dx.doi.org/10.1097/01.sap.0000203317.50871.5c. PMid:16721069
10. Hönig JF, Frank MH, Knutti D, de La Fuente A. Video endoscopic-assisted brow lift: comparison of the eyebrow position after Endotine tissue fixation versus suture fixation. J Craniofac Surg. 2008;19(4):1140-7. http://dx.doi.org/10.1097/SCS.0b013e3181764b19. PMid:18650749
11. Badin AZ, Bittencourt LM, Balderrama CR. Lateral brow fixation in endoscopic forehead lift: long-term results with braided nylon percutaneous sutures. Aesthetic Plast Surg. 2010;34(1):78-87. http://dx.doi.org/10.1007/s00266-009-9401-5. PMid:19787395
12. Romo T 3rd, Sclafani AP, Yung RT, McCormick SA, Cocker R, McCormick SU. Endoscopic foreheadplasty: a histologic comparison of periosteal refixation after endoscopic versus bicoronal lift. Plast Reconstr Surg. 2000;105(3):1111-9. http://dx.doi.org/10.1097/00006534-200003000-00042. PMid:10724273
1. Plastic Surgeon, Full Member of the Brazilian Society of Plastic Surgery (BSPS), Preceptor of Serviço de Cirurgia Plástica of Santa Casa de Porto Alegre, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil
2. Plastic Surgeon, Full Member of the Brazilian Society of Plastic Surgery (BSPS), Chief of the Plastic Surgery Department of the "Irmandade Santa Casa de Misericórdia" of Porto Alegre, Adjunct Professor of the Departamento de Cirurgia Plástica of Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil
3. Resident of Plastic Surgery of Serviço de Cirurgia Plástica of Santa Casa de Porto Alegre, Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil
Institution: Work conducted at the Irmandade Santa Casa de Misericórdia Hospital, Porto Alegre, RS, Brazil, and in the Mãe de Deus Center Hospital, Porto Alegre, RS, Brazil.
Corresponding author:
Mariana Zancanaro
Serviço de Cirurgia Plástica da Santa Casa de Porto Alegre, Universidade Federal de Ciências da Saúde de Porto Alegre
Rua Sarmento Leite, 245
Porto Alegre, RS, Brazil CEP 90050-170
E-mail: mariana_zancanaro@hotmail.com
Article received: May 1, 2014.
Article accepted: August 3, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter