

Ideas and Innovation - Year 2014 - Volume 29 -
Single layer closure of hard palate cleft and oronasal fistula
Palatoplastia em plano único e fístula oronasal
ABSTRACT
INTRODUCTION: Traditionally, cleft of the hard palate is repaired in two layers, with a nasal mucosal layer and an oral mucoperiosteal layer. The aim of this study was to evaluate the results of one layer closure of hard palate cleft compared to the traditional two layers closure.
METHODS: The charts of 101 consecutive cases of repair of hard palate cleft performed by the authors from 1981 to 2012 at a tertiary care clinic/hospital in central Wisconsin were reviewed. The cases utilized the single layer closure and were followed in the Cleft Palate Clinic on a yearly basis. Cases included unilateral and bilateral cleft lip and palate as well as isolated cleft palate.
RESULTS: All cases healed satisfactorily except for two cases that later required small fistulae repair.
CONCLUSION: Single layer closure of the hard palate cleft is as effective as traditional two-layer closure, with minimal complications.
Keywords: Cleft palate; Craniofacial; Hard palate repair; Oronasal fistula.
RESUMO
INTRODUÇÃO: Tradicionamente, a fissura palatina é corrigida em duas camadas - uma camada mucosa nasal e camada mucoperiosteal oral. Este estudo avaliou os resultados do fechamento em camada única de fissura palatina comparado ao fechamento tradicional em camada dupla.
MÉTODOS: Tratase de revisão de pronturários de 101 casos de correção de fissura palatina realizados entre 1981 e 2012 em uma clínica assistencial/hospital terciário localizado no centro de Wisconsin. Os casos utilizaram fechamento em camada única e foram acompanhados em Clínica de Lábio Leporino por 12 meses. Foram incluidas fissura labial e palatina também como fissura palatina isolada.
RESULTADOS: Todos os casos apresentaram cicatrização satisfatória exceto dois casos que necessitaram de correção posterior de pequena fistula.
CONCLUSÃO: O fechamento em camada única de fissura palatina é tão efetivo quanto o fechamento tradicional em camada dupla, além disso apresenta mínimas complicações.
Palavras-chave: Fissura palatine; Craniofacila; Correção de Palato Duro; Fístula Oronasal.
The hard palate acts as a partition between the nasal and oral cavities, preventing regurgitation of fluids into nasal cavity, and promoting resonance of voice during speech. Traditionally, hard palate cleft has been repaired in two layers, with a nasal mucosal layer and an oral mucoperiosteal layer. This paper reviews 101 cases of hard palate clefts repaired by the authors using only the mucoperiosteal layer, as a single layer closure. All cases were done at Marshfield Clinic/St. Joseph's Hospital, a tertiary care center in central Wisconsin, where patients were followed in the Cleft Palate Clinic on a yearly basis. The Cleft Palate Clinic team consists of plastic surgeons, oral surgeons, an orthodontist, a speech therapist, an audiologist, pediatricians, a geneticist, and social workers.
METHODS
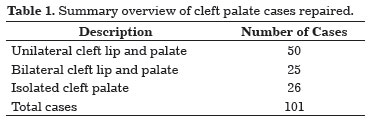
The study was reviewed and determined to be exempt by the Marshfield Clinic Institutional Review Board, and the requirement for consent was waived. The total number of cases reviewed was 101. Of these cases, 50 were unilateral cleft lip and palate (UCLP), 25 were bilateral cleft lip and palate (BCLP), and 26 were isolated cleft palate. Bilateral cases had wider gaps than unilateral clefts. The average gap at the posterior border of the hard palate before repair was 1 cm to 1.5 cm as measured using calipers (Table 1). Cases excluded from the study were submucus clefts, cleft lip with alveolar cleft only, and cases with severe cognitive deficiency.
The protocol followed for repair of the cleft cases was: lip repair at age 3-4 months, soft palate repair at age 6-7 months, and hard palate repair at age 12-18 months. Following repair of the soft palate, the hard palate cleft was obturated by an acrylic plate to prevent regurgitation of food and fluid and to continue speech therapy. During this waiting period before the hard palate repair, the palatal gap narrowed with the growth of the child, and more palatal tissues become available for repair of the cleft with minimal tension. The method of hard palate repair was the two flap technique as described by Bardach1, raising mucoperiosteal layers on both sides as unipedicle axial flaps based on greater palatine vessels. Lateral relaxing incisions were made from the maxillary tuberosity to the anterior end of the palatal cleft. Flaps were mobilized towards the midline from each side and closure was done with 4-0 Vicryl sutures after freshening the cleft edges with a No. 11 surgical blade. Oral feeding was started with clear liquids on the day of surgery, and infant formula was given beginning the day after surgery. The child was kept in the hospital for 2 days.
The raw areas at the gingival margins were narrowed down by placing two or three 4-0 Vicryl sutures. Alveolar gaps greater than 5 mm at the anterior end were closed by a labial mucosal or vomer flap. Alveolar gaps less than 5 mm were left open, to be repaired at the time of bone grafting. Figures 1 through 6 illustrate six cases of unilateral cleft palate repair pre-operatively and then post-operatively at approximately 2.5 years of age.
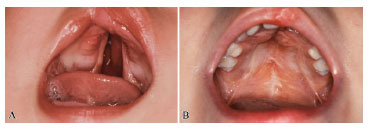
Figure 1. Photograph showing unilateral cleft palate: (A) preoperative at 3 months, and (B) post-operative at 2.5 years of age.

Figure 2. Photograph showing unilateral cleft palate: (A) preoperative at 3 months, and (B) post-operative at 2.5 years of age.

Figure 3. Photograph showing unilateral cleft palate: (A) preoperative at 3 months, and (B) post-operative at 2.5 years of age.
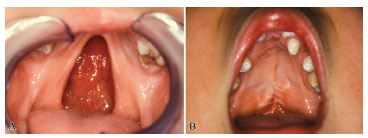
Figure 4. Photograph showing unilateral cleft palate: (A) preoperative at 3 months, and (B) post-operative at 2.5 years of age.
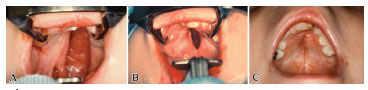
Figure 5. Photograph showing unilateral cleft palate: (A) preoperative at 3 months, (B) post-operative closure of the soft palate at 6 months, and (C) final result at 2.5 years of age.
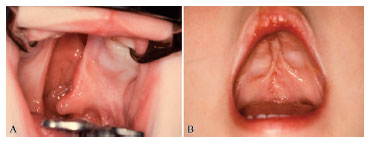
Figure 6. Photograph showing unilateral cleft palate: (A) preoperative at 3 months, and (B) post-operative at 2.5 years of age.
RESULTS
All cases healed well, except for two patients who developed small fistulas at the operative site; one at the anterior end in a UCLP case and one at the junction of the hard and soft palates in a BCLP case. These were repaired at a later period when scar tissue had softened.
DISCUSSION
Although hard palate cleft repair has been traditionally performed using two layers, personal experience of the authors with the above-described 101 cases shows that effective repair can be done in one layer using a mucoperiosteal flap. This flap is an axial flap, well-vascularized and tough in texture. In early delayed, two-stage palatoplasty (i.e., repairing between the ages of 12-18 months)2, the hard palate gap becomes narrowed, and repair can be performed with minimal tension. Even the gaps at the gingival margins as a result of lateral release can be narrowed down by using two to three 4-0 Vicryl sutures, thus leaving a minimal bony raw area. Single mucosal flaps are not elevated, and the palatal shelves are not completely denuded. An intact hard palate acts as a resonator of voice, so avoiding a fistula of the hard palate aids in speech.
In the authors' experience, the incidence of fistula has been low-only 2 cases in 101 patients. Fistula has been defined as a breakdown after palatal repair3. Small openings (< 5mm) at the anterior end do not cause any functional problem and can be left alone, thus, not producing any scaring in the area, which would be helpful during bone grafting at a future date. Common causes for fistula include wide palatal gap4,5, tension at the suture line6, infection7, technique and experience of the surgeon7, and age of the patient at time of repair8. Common sites for fistula formation (in order of rate of occurrence) are (1) at the junction of the hard and soft palates, (2) the mid-palatal area, and (3) anterior palate-post alveolar areas9. Recurrent fistulas are difficult to repair due to scarring, and failure is quite common; therefore, it is very important to do everything possible to avoid recurrence.
The true incidence of fistula formation is difficult to assess from the literature due to lack of clarity in defining true fistula. Some authors have defined true fistula as a breakdown after palatal repair, while others have included all palatal openings present on operated or non-operated areas. The reported incidence of fistula formation in the literature ranges from 0% to 37%10-22, with recent publications reporting a recurrence rate between 25% to 40%9. The incidence in the study reported here is 2%. This low incidence can be attributed to: (1) repair with minimum tension; (2) good vascularity of the flaps; and (3) operating when the palatal gap gets narrower, at age 12-18 months.
CONCLUSIONS
Repair of hard palate cleft can be successfully achieved with minimal complications, using a one layer closure. In this approach, the mucoperiosteal flap is well vascularized. Attention must be paid to careful elevation of the flap and to completing the repair with minimum tension. Sparing the nasal mucosa avoids complete denudation of the palatal shelves and does not increase fistula formation.
REFERENCES
1. Bardach J. Two-flap palatoplasty: Bardach's technique. Operative Tech Plast Surg. 1995;2(4):211-4. http://dx.doi.org/10.1016/S1071-0949(06)80034-X.
2. Rohrich RJ, Byrd HS. Optimal timing of cleft palate closure. Speech, facial growth, and hearing considerations. Clin Plast Surg. 1990;17(1):27-36. PMid:2406096.
3. Cohen SR, Kalinowski J, LaRossa D, Randall P. Cleft palate fistulas: a multivariate statistical analysis of prevalence, etiology, and surgical management. Plast Reconstr Surg. 1991;87(6):1041-7. http://dx.doi.org/10.1097/00006534-199106000-00005. PMid:2034725
4. Musgrave RH, Bremner JC. Complications of cleft palate surgery. Plast Reconstr Surg Transplant Bull. 1960;26(2):180-9. http://dx.doi.org/10.1097/00006534-196008000-00003. PMid:14425494
5. Parwaz MA, Sharma RK, Parashar A, Nanda V, Biswas G, Makkar S. Width of cleft palate and postoperative palatal fistula-do they correlate? J Plast Reconstr Aesthet Surg. 2009;62(12):1559-63. http://dx.doi.org/10.1016/j.bjps.2008.05.048. PMid:18838320
6. Sadhu P. Oronasal fistula in cleft palate surgery. Indian J Plast Surg. 2009;42(3 Suppl):S123-8. http://dx.doi.org/10.4103/0970-0358.57203. PMid:19884667
7. Kilner TP. Cleft lip and palate repair technique. St. Thomas' Hosp Report. 1937;2:127.
8. Andersson EM, Sandvik L, Semb G, Abyholm F. Palatal fistulas after primary repair of clefts of the secondary palate. Scand J Plast Reconstr Surg Hand Surg. 2008;42(6):296-9. http://dx.doi.org/10.1080/02844310802299676. PMid:18991171
9. Diah E, Lo LJ, Yun C, Wang R, Wahyuni LK, Chen YR. Cleft oronasal fistula: a review of treatment results and a surgical management algorithm proposal. Chang Gung Med J. 2007;30(6):529-37. PMid:18350736.
10. Brusati R, Mannucci N. Repair of the cleft palate without lateral release incisions: results concerning 124 cases. J Craniomaxillofac Surg. 1994;22(3):138-43. http://dx.doi.org/10.1016/S1010-5182(05)80378-6. PMid:8063904
11. Muzaffar AR, Byrd HS, Rohrich RJ, Johns DF, LeBlanc D, Beran SJ, et al. Incidence of cleft palate fistula: an institutional experience with two-stage palatal repair. Plast Reconstr Surg. 2001;108(6):1515-8. http://dx.doi.org/10.1097/00006534-200111000-00011. PMid:11711920
12. Wilhelmi BJ, Appelt EA, Hill L, Blackwell SJ. Palatal fistulas: rare with the two-flap palatoplasty repair. Plast Reconstr Surg. 2001;107(2):315-8. http://dx.doi.org/10.1097/00006534-200102000-00002. PMid:11214043
13. Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112(6):1542-8. http://dx.doi.org/10.1097/01.PRS.0000085599.84458.D2. PMid:14578783
14. Bekerecioglu M, Isik D, Bulut O. Comparison of the rate of palatal fistulation after two-flap and four-flap palatoplasty. Scand J Plast Reconstr Surg Hand Surg. 2005;39(5):287-9. http://dx.doi.org/10.1080/02844310510006529. PMid:16320405
15. Inman DS, Thomas P, Hodgkinson PD, Reid CA. Oro-nasal fistula development and velopharyngeal insufficiency following primary cleft palate surgery-an audit of 148 children born between 1985 and 1997. Br J Plast Surg. 2005;58(8):1051-4. http://dx.doi.org/10.1016/j.bjps.2005.05.019. PMid:16084930
16. Khosla RK, Mabry K, Castiglione CL. Clinical outcomes of the Furlow Z-plasty for primary cleft palate repair. Cleft Palate Craniofac J. 2008;45(5):501-10. http://dx.doi.org/10.1597/07-063.1. PMid:18788872
17. Losee JE, Smith DM, Afifi AM, Jiang S, Ford M, Vecchione L, et al. A successful algorithm for limiting postoperative fistulae following palatal procedures in the patient with orofacial clefting. Plast Reconstr Surg. 2008;122(2):544-54. http://dx.doi.org/10.1097/PRS.0b013e31817d6223. PMid:18626373
18. Phua YS, de Chalain T. Incidence of oronasal fistulae and velopharyngeal insufficiency after cleft palate repair: an audit of 211 children born between 1990 and 2004. Cleft Palate Craniofac J. 2008;45(2):172-8. http://dx.doi.org/10.1597/06-205.1. PMid:18333650
19. Stewart TL, Fisher DM, Olson JL. Modified Von Langenbeck cleft palate repair using an anterior triangular flap: decreased incidence of anterior oronasal fistulas. Cleft Palate Craniofac J. 2009;46(3):299-304. http://dx.doi.org/10.1597/07-185.1. PMid:19642748
20. Eberlinc A, Kozelj V. Incidence of residual oronasal fistulas: a 20-year experience. Cleft Palate Craniofac J. 2012;49(6):643-8. http://dx.doi.org/10.1597/10-146. PMid:21740163
21. Steinbacher DM, McGrath JL, Low DW. Is nasal mucoperiosteal closure necessary in cleft palate repair? Plast Reconstr Surg. 2011;127(2):768-73. http://dx.doi.org/10.1097/PRS.0b013e3181fed80a. PMid:21285779
22. Jain H, Rao D, Sharma S, Gupta S. Assessment of speech in primary cleft palate by two-layer closure (conservative management). J Surg Tech Case Rep. 2012;4(1):6-9. http://dx.doi.org/10.4103/2006-8808.100344. PMid:23066454
1. Dr., Retired, former plastic surgeon, Marshfield Clinic, Marshfield, Wisconsin, USA
2. Dr., Plastic Surgeon, Marshfield Clinic, Marshfield, Wisconsin, USA
Institution: Study performed at the Marshfield Clinic, Marshfield, Wisconsin, USA.
Corresponding author:
Julio Hochberg
Plastic Surgery Department 3F, Marshfield Clinic
100 North Oak Av.
Marshfield, Wisconsin, USA 54449
E-mail: dr.hamburger@gmail.com
Article received: September 30, 2013.
Article accepted: January 11, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter