

Original Article - Year 2014 - Volume 29 -
Plastic surgeons as hand surgeons: residents' perceptions
Cirurgiões plásticos como cirurgiões de mão: a visão dos residentes
ABSTRACT
INTRODUCTION: Previous studies have revealed that residents have misconceptions about plastic surgeons as hand surgery specialists. Until now, however, there have been no specific data on this trend in Brazilian scientific literature. Therefore, the aim of this study was to evaluate Brazilian residents' knowledge and perceptions about the role of plastic surgeons in the field of hand surgery.
METHOD: Brazilian residents chose one or two specialists they believed to be experts for eight scenarios related to hand surgery. The responses were categorized as "plastic surgeons", "without plastic surgeons", "only plastic surgeons", "plastic surgeons combined with other specialists", or "plastic surgeons absent".
RESULT: Responses without plastic surgeons and with plastic surgeons absent were chosen more often than all other responses in all scenarios (p<0.05 for all comparisons). Plastic surgeons were less often recognized as experts compared to orthopedic (six scenarios), general (one scenario), and neurosurgeons (one scenario) (p<0.05 for all comparisons).
CONCLUSION: Brazilian residents have limited knowledge and perceptions about hand surgery performed by plastic surgeons.
Keywords: Brazil; Field; Plastic surgery; Hand; Perceptions; Residents.
RESUMO
INTRODUÇÃO: Pesquisas prévias têm revelado que residentes têm conhecimentos equivocados sobre a atuação dos cirurgiões plásticos como especialistas em cirurgia da mão. No entanto, até o momento, não existem dados específicos abordando tal aspecto na literatura científica brasileira. Portanto, o objetivo deste estudo foi avaliar os conhecimentos e as percepções dos residentes sobre o papel dos cirurgiões plásticos no campo cirurgia da mão no Brasil.
MÉTODO: Residentes brasileiros escolheram um ou dois especialistas que eles acreditassem ser experts para oito cenários relacionados à cirurgia de mão. Os padrões de respostas foram distribuídos como "cirurgiões plásticos" ou "sem cirurgiões plásticos", e "apenas cirurgiões plásticos", "cirurgiões plásticos combinados com outros especialistas" ou "cirurgiões plásticos ausentes".
RESULTADO: "Sem cirurgiões plásticos" e "cirurgiões plásticos ausentes" foram mais (p<0,05, para todas as comparações) escolhidos que todos os outros padrões de respostas, em todos os cenários. Cirurgiões plásticos foram menos (p<0,05, para todas as comparações) reconhecidos que cirurgiões ortopédicos (seis cenários), cirurgiões gerais (um cenário) e neurocirurgiões (um cenário).
CONCLUSÃO: Os conhecimentos e as percepções dos residentes brasileiros sobre o trabalho realizado por cirurgiões plásticos no campo cirurgia da mão são limitados.
Palavras-chave: Brasil; Campo; Cirurgia plástica; Mão; Percepções; Residentes.
Plastic surgeons and plastic surgery as a specialty have been the subjects of numerous publications,1 and a new paradigm has recently incorporated this idea. In addition to traditionally defined cosmetic and reconstructive roles of plastic surgeons, the concept of restorative plastic surgeons has proposed based on principles established by Dr. Joseph Murray, a Nobel Prize winner, plastic surgeon, and pioneer in organ transplantation that culminated in immeasurable progress in vascularized composite allotransplantation2.
While plastic surgeons should continue to focus on developing and improving surgical techniques and technologies with the goal of consolidating and developing the art and science of plastic surgery2, it is also important that they be aware of alarming data presented in a growing list of international studies on the lack of knowledge, incorrect perceptions, and underestimation by the lay public, patients, medical students, and health professionals on the scope of work done by plastic surgeons3-7. Among the many areas evaluated (for example, aesthetic surgery, craniofacial surgery, burns, etc.)3-7, the lack of knowledge among medical students and American and Indian residents on the role of plastic surgeons in scenarios related to hand surgery was prominent3-7.
Because residents are an important source of patient information on the complex and wide range of therapeutic options offered by plastic surgeons, and also refer patients for specialist care, it is of utmost importance that their knowledge and perceptions about the complexity and breadth of practice of plastic surgeons be fully understood and defined3-5. Thus, special educational measures can be established that may positively impact the proper referral of patients with hand diseases3-7. However, to the best of our knowledge, no study in the national plastic surgery literature has evaluated the knowledge of residents regarding the role of plastic surgeons in the field of hand surgery.
Therefore, the objective of this study was to assess the knowledge and perceptions of Brazilian residents about the role of plastic surgeons in the field of hand surgery.
METHODS
This was a cross-sectional analysis of residents in training at medical residency programs in general surgery, internal medicine, and pediatrics at the Dr. Mário Gatti Municipal Hospital (HMMG) in Campinas, Sao Paulo, Brazil. All residents responded to an anonymous survey in the fourth quarter of 2013; previous studies6,7 reported that the majority of residents have completed their didactic training and practice during this period; therefore, global and specific knowledge from the first and second years of training are considered in their responses. To reduce bias, no resident received explanations about the study purpose6,7. This study was approved by the Committee on Ethics in Research on Humans at HMMG, via the National System of Information on Ethics in Research involving Human Beings (SISNEP), and is in accordance with the 1975 Declaration of Helsinki and its 1983 revision. Completion of the survey was considered implied consent for participation.
The survey contained eight scenarios related to hand surgery adapted from similar studies3-7. The residents chose one or two specialists they believed to be experts for each scenario (for example: "Who do you think are experts in hand surgeries?")3. General, plastic, orthopedic, vascular, and neurosurgeons were listed as multiple-choice options. All scenarios were arranged randomly and the residents could not access previously answered questions. Residents were also asked if they had been exposed to plastic surgery during rotations, internships, or curriculum and formal subjects during their medical undergraduate courses or residencies6,7. Demographic variables [gender (male or female), residency program (general surgery, internal medicine or pediatrics) and year of training (first or second year)] were also queried. Residents who did not choose at least one answer to each question were excluded.
Statistical Analysis
All information was compiled in Excel 2013 for Windows (Microsoft Corporation, USA). For descriptive analysis, means and percentages were calculated for metric and categorical variables, respectively. The scenario responses were divided into "plastic surgeons often chosen" (>70% of resident responses) and "plastic surgeons rarely chosen" (< 30% of responses, including overall absence of plastic surgeons, or 0%)6. Two standard response profiles were defined3: "plastic surgeons" versus "without plastic surgeons" and "only plastic surgeons" versus "plastic surgeons combined with other specialists" versus "plastic surgeons absent". The frequency of distribution (percentage of scenarios in which each expert appeared in one of the responses) was calculated for each expert, and plastic surgeons were considered the variable of primary interest3,6. Comparisons were made between gender (female versus male), residency programs (general surgery versus clinical medicine versus pediatrics), years of training (first year versus second year) and previous exposure to plastic surgery ("with exposure" versus "without exposure"). Different tests, including analysis of variance (ANOVA), Tukey test, equality of two proportions, paired T-test, and confidence interval for the mean, were used for statistical comparisons. SPSS Statistics for Windows, version 17.0 (SPSS, Inc., Chicago, IL, USA) and Minitab 16 Statistical Software (Minitab, Inc., State College, PA, USA) were used for statistical analyses. Values with a 95% confidence interval (p< 0.05) were considered statistically significant.
RESULTS
Forty-seven (97.92%) residents completed the survey. There was a female (74.5%) over male predominance (25.5%) (p< 0.05), with no significant differences between residency programs (general surgery, 32%; clinical medicine, 34%; pediatrics, 34%) or years of residence (first year, 51%; second year, 49%)(p>0.05 for all comparisons). Twenty-nine residents (62% of the total; p< 0.05) reported having rotated in plastic surgery internships during their undergraduate medical courses, and seven (all second-year general surgery residents; 15% of the total; p< 0.05) had rotated in plastic surgery internships during their residency.
Plastic surgeons were rarely (< 70%) chosen in 62.5% of the scenarios, were not chosen by any resident in 25% of the scenarios, and were not often chosen (>70%) by residents in any scenario (Table 1). Considering the patterns of answers, "plastic surgeons", "only plastic surgeons", and "plastic surgeons combined with other specialists", were chosen by less than 30% of the residents in 87.5%, 100%, and 100% of the scenarios, respectively. "Plastic surgeons", "only plastic surgeons" and "plastic surgeons combined with other specialists" were not chosen by any resident in two (25%) scenarios. "Without plastic surgeons" and "plastic surgeons absent" were chosen by more than 70% of the residents in 87.5% of the scenarios. "Plastic surgeons", "only plastic surgeons", and "plastic surgeons combined with other specialists" were not chosen by more than 70% of the residents in any scenario (Figures 1 and 2).
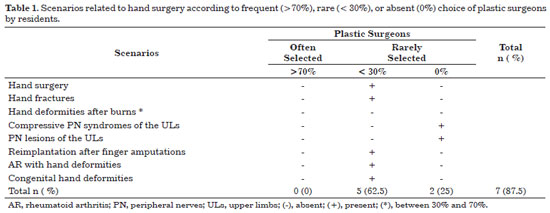
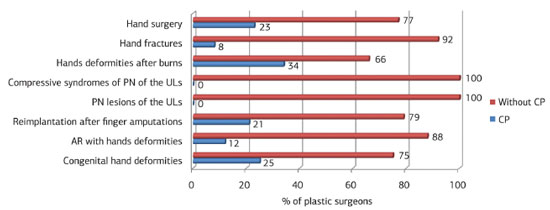
Figure 1. Percentages of "plastic surgeons" (CP) and "without plastic surgeons" (without CP) selected for eight scenarios related to hand surgery. "CP" were chosen significantly (p<0.02 for all comparisons) less often than "without CP" for all scenarios. AR, rheumatoid arthritis; NP, peripheral nerves; ULs, upper limbs.
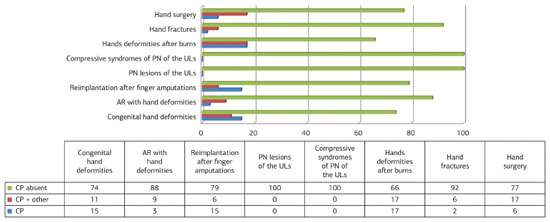
Figure 2. Percentages of "only plastic surgeons" (CP), "plastic surgeons combined with other specialists" (CP + other), and "plastic surgeons absent" (CP absent) responses according to eight scenarios related to hand surgery. "CP missing" was significantly (p<0.001 for all comparisons) more common than "CP" and "CP + other" in all scenarios. There were no significant differences (p>0.05 for all comparisons) between "CP" and "CP + other" in any scenario. AR, rheumatoid arthritis; NP, peripheral nerves; ULs, upper limbs.
Overall analysis of all scenarios together revealed that the "without plastic surgeons" (84.63% ± 12.35%) and "plastic surgeons absent" (84.5% ± 12.47%) response patterns were significantly more common than the other response patterns ("plastic surgeons", 15.37% ± 12.35%; "only plastic surgeons", 7.25 % ± 7.24 %; and "plastic surgeons combined with other specialists", 8.25% ± 6.63%) (p<0.05 for all comparisons). The individual analysis of each scenario revealed that the response patterns "without plastic surgeons" and "plastic surgeons absent" were significantly more often chosen by residents than the other patterns in all scenarios (p<0.05 for all comparisons). The proportion of responses corresponding to "only plastic surgeons" and "plastic surgeons combined with other specialists" were similar (p>0.05 for all comparisons) in all scenarios (Figures 1 and 2).
Among specialists (Figure 3), plastic surgeons were not considered the main experts in any scenario. Orthopedic surgeons were significantly (p<0.05 for all comparisons) more often chosen as the preferred specialists in 75% of scenarios. General and neurosurgeons were significantly (p<0.05 for all comparisons) chosen as the leading experts in one (12.5%) scenario each.
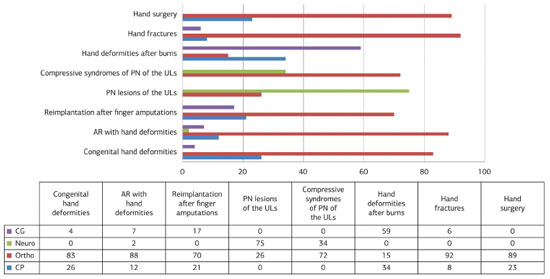
Figure 3. Percentages of specialists selected for eight scenarios related to hand surgery. Comparison between "CP" (if present) and each specialist in isolation revealed statistical significant differences (p<0.001) for all comparisons, except for "CP" versus "CG" in the scenarios: AR with deformities of hands, reimplantation after amputation of fingers and fractures of the hands, with p>0.05. CG- general surgeons; Neuro, neurosurgeons; Ortho, orthopedic surgeons; CP, plastic surgeons; AR, rheumatoid arthritis; NP, peripheral nerves; MMSS, upper limbs. Note: the total may be greater than 100% because residents could choose one or two specialists for each scenario.
Analysis of "plastic surgeons" responses did not show significant differences between genders, the three residency programs, years of training, or previous exposure to plastic surgery (p>0.05 for all comparisons).
DISCUSSION
Hand surgery is commonly considered to have evolved from work performed by general, plastic, orthopedic, vascular, and neurosurgeons to treat injuries of the extremities during the Second World War. At that time, a section designated specifically for hand surgery was created and led by the plastic surgeon Dr. J. William Littler8. Dr. Sterling Bunnell (the "father of hand surgery") also introduced concept of the regional surgeon, describing specialists in specific anatomical regions that could deal with all the structures and tissues in that region, who could, therefore, perform any surgical procedures and repair all the necessary structures in a single surgical procedure. In the 1940s, hand surgery became a skill, with formation of regional hand centers and hand societies as well as publication of the Surgery of the Hand monograph by Dr. Bunnell8. Since then, interest in hand surgery has continued to increase and many surgeons have contributed to the development of this field, including, Drs. Allen Kanavel, Sumner Koch, Michael Mason, Earle Peacock, Harry J. Buncke, Alípio Pernet, Orlando Graner, Lauro Barros de Abreu, Henrique Bulcão de Moraes and, more recently, Dr. Joseph Upton, a plastic surgeon who has valuable experience in treating children with congenital hand deformities. Thus, in addition to treating hand injuries, hand surgeons also currently deal with a range of hand, wrist, and distal forearm disorders such as congenital defects, deformities secondary to rheumatoid arthritis, Dupuytren's contracture, peripheral nerve compression, repair and reconstructions of tendons and nerves, and tissue reimplantation and microsurgical procedures7-9.
In the United States, this field of practice is currently composed predominantly of orthopedic surgeons, followed by plastic and general surgeons; only those certified in some of these specialties may participate in the selection process to enter hand surgeon training centers9. In Brazil, hand surgery is a medical specialty with its own medical residency recognized by the Ministry of Education (MEC). Only orthopedic and plastic surgeons may participate in selection processes to enter hand surgery training centers organized by the Brazilian Society of Hand Surgery (SBCM) in conjunction with the Brazilian Medical Association (AMB), and receive certification in hand surgery. In this context, it should be noted that the overlapping practice of these specialists can cause confusion among those outside the hand surgery field (for example, lay public, medical students, health workers, and residents)3-7, since the dividing lines between some of those specialties (mainly, plastic and orthopedic surgery) are vague and often absent7.
The plastic surgery literature has shown limited knowledge and perceptions about the work performed by plastic surgeons in the field of hand surgery that often underestimates the versatility and magnitude of therapeutic modalities offered by well-trained plastic surgeons3-7. However, data related to resident perceptions of plastic surgery in the field of hand surgery are restricted to international studies3-5, which include only some scenarios specific to hand surgery. In fact, only one study7 focused on the elucidation of American medical student perceptions of plastic surgeons as hand surgeons.
In this context, the present study investigated resident knowledge and perceptions about the role of plastic surgeons in the context of hand surgery, since the surgeons focus on the comprehensive care of countless patients with congenital hand deformities, including reconstruction of complex symmetric acrocephalosyndactylia and patients with Apert syndrome, which has positively impacted the quality of life of these patients10,11. For this reason, we evaluated residents in training in the same city as the Institute of Plastic Surgery12. Thus, this analysis will allow us to adapt and strengthen our educational programs to address the specific needs of residents in this region, because it can directly affect the care provided to patients with congenital or acquired developmental hand deformities. In addition, this study may also act as a model for other institutions to assess their own residents and those working in their regions, and also establish educational programs to increase appreciation of plastic surgery as a specialty that deals with resection, repair, replacement, and reconstruction of any abnormalities of skin form and function, the musculoskeletal system, the skull and face, hands, and limbs, among other tissues and anatomical areas1. Ultimately, such data, initiatives, and future modifications may also ensure that hand surgery remains an integral part of plastic surgery7.
Our research revealed that plastic surgeons were significantly less often recognized as experts compared to orthopedic, general, and neurosurgeons, in all evaluated scenarios related to hand surgery. In addition, as other specialists (general and orthopedic surgeons) were significantly more often chosen as experts in scenarios relevant to plastic surgery (hand deformities after burns and congenital deformities), our data reinforce previous analyses3-7 that highlighted knowledge deficits even in traditional areas of practice.
Similar to the global trends described in previous studies3-7, our results demonstrate widespread limited knowledge about the practice of plastic surgeons in the field of hand surgery among the Brazilian residents queried. However, the study findings differ3-7 when the outcomes of each scenario are analyzed individually. The percentage of Brazilian residents in our study who chose plastic surgeons as experts ranged from 0% (for both compressive syndromes and lesions of peripheral nerves of the upper limbs) to 39% (hand deformities after burn injuries), with an average of 15.5%. In the international literature, the percentage of medical students and residents who chose plastic surgeons ranged from 8.7% (brachial plexus injury) to 97% (burned hands) 3-7, with an average of 32.3%7. In addition, the percentage of Brazilian residents that selected orthopedic surgeons as experts ranged from 15% (hands deformities after burn injuries) to 92% (hand fractures), with an average of 66.88%. Similarly, the percentage of medical students and residents in other studies3-7 who selected orthopedic surgeons ranged from 3.0% (burned hands) to 100% (fractured hands), with an average of 59.7%7.
Definitive explanations for the findings of the current study will require additional studies. However, it is important to discuss likely reasons for the lack of recognition of plastic surgeons as hand surgeons, evidenced by the results presented here and elsewhere3-7. The importance of this field of activity for plastic surgery has been described by the American Society of Plastic Surgeons (ASPS)13, which reported that hand surgeries are among the five reconstructive procedures most commonly performed by plastic surgeons.
The high percentage of residents who did not appreciate plastic surgeons may reflect increased marketing, promotion and education of other specialties3. In addition, the proportion of specialists who practice hand surgery and increased overlap of the practice of these specialists contribute to the lack of differentiation of the specific role of each surgeon in the treatment of many hand diseases7. In recent years, the proportion of American plastic surgeons participating in hand surgery training programs has been lower than the proportion of orthopedic surgeons9. This discrepancy may be even greater in Brazil, mainly because the number of plastic surgery training centers that perform hand surgeries is limited and are located primarily in the southeast region. In fact, in accordance with the charters of the bodies that regulate training in plastic surgery in Brazil - the National Committee for Medical Residency (CNRM) of the MEC and the Department of Accredited Education Services of the Brazilian Society of Plastic Surgery (SBCP) - all plastic surgery residents should receive mandatory training in hand surgery14. However, according to a recent survey14, less than 30% of the residents of plastic surgery residency programs in the Federal District had received training in hand. In addition to cosmetic surgery, the members of our residency program in plastic surgery have taught future plastic surgeons the principles of reconstructive plastic surgery (underpinnings of the plastic surgery specialty and the basis of the foundation and consolidation of our Institute12), because we believe, like others1,15, that the therapeutic arsenal should be as diverse as possible in an increasingly competitive plastic surgery market15. In this way, the residents in training have acquired theoretical and practical knowledge, including surgical skills to treat numerous hand diseases. Nevertheless, regardless of training, the senior author (CERA) notes that, in the wake of this training program, residents do not remain in this specific field of practice after completing their residencies and, therefore, do not extend their expertise in this area or participate in the certification process to obtain a title of hand surgery specialist, from the SBCM/AMB. As our perceptions are anecdotes and there are no official Brazilian data to confirm our hypothesis, future studies should clarify the impact of training of Brazilian plastic surgeons and the proportion of plastic surgeons who work in the field of hand surgery in the absence of knowledge about the plastic surgeons as hand surgeons.
Various international studies3-6 have revealed that plastic surgeons are mainly recognized as aesthetic surgeons. In Brazil, plastic surgeons were selected as experts only in scenarios related to cosmetic surgery (rhinoplasty and problems with facial appearance)16. Thus, perceptions related to the aesthetics of plastic surgery can obscure the work performed by plastic surgeons in many areas such as craniofacial, hand, and microsurgery and, therefore, may also partially explain the results presented here and in other studies3-7. These perceptions probably originated from the media and television programs ("reality shows") that have disseminated the aesthetic aspects of plastic surgery, as revealed in an international study17, which reported that the majority of articles published in magazines and newspapers in the United Kingdom used the term "plastic surgery" in the context of "cosmetic surgery" and only a small portion in the context of "reconstructive procedures". In addition, medical students have reported that their knowledge regarding plastic surgery is predominantly acquired from the media18,19. Future research should investigate the real impact of the media on Brazilian resident perceptions of plastic surgeons as hand surgeons, because we did not assess this particular aspect in this study.
Similar to findings in another study7, some specific scenarios such as hand fractures, compressive syndromes and lesions of peripheral nerves of the upper limbs, validate our research findings because they reflect the pattern of distribution of hand surgeries in the hospital under study. Thus, another factor that could explain our results is the nature of the practice and plastic surgery training at this hospital. This hospital has residency programs in orthopedics, plastic surgery, and neurosurgery, and, therefore, professionals from all these specialties. However, hand fractures are handled almost exclusively by orthopedic surgeons. Surgeries on patients with tendon and nerve disorders of the upper limbs are performed by orthopedic or neurosurgeons. Initial treatment of burn patients is performed by plastic surgeons; however, as there is no specific unit for treatment of burn patients, the patients are always referred to other services, and there is, therefore, no longitudinal follow-up of burns. In addition, patients with hand deformities secondary to burns or with congenital hand deformities are not treated by any group at the hospital and are routinely sent to our Institute. As the residents of the three residency programs in this study acquire theoretical and practical skills, and have contacts with residents and professionals from other specialties, predominantly in the hospital environment, the pattern of distribution of hand surgeries may have influenced the responses of each scenario.
In addition, we found no significant differences between residency programs and years of training. A previous study3 showed that pediatric residents had a greater awareness of the extent of plastic surgeons' practice, and also reported that years of training did not significantly affect the results; however, there was no specific analysis on scenarios related to hand surgery3. They also demonstrated that there were no significant differences between the presence and the absence of prior exposure to plastic surgery during the undergraduate medical course and/or residency. Another study7 also revealed that more than half of medical students did not choose plastic surgeons as hand surgery specialists, even after having prior exposure to plastic surgery. In addition, medical students with previous exposure to orthopedic and general surgery were less likely to choose plastic surgeons as specialists for treatment of carpal tunnel syndrome and burned hands7.
Our findings, together with those described in other studies3-7, indicate an educational deficiency during undergraduate medical courses3 and residency7 on the scope of plastic surgery. In fact, the curricula of the residency programs evaluated in this study devote little time to plastic surgery, as demonstrated in our results; only second-year general surgery residents receive formal training in plastic surgery. Thus, as we have demonstrated that there are no differences between the training programs, years of training, and previous exposure to plastic surgery, there are limited opportunities to learn about the specific roles of plastic surgeons in the field of hand surgery during the training of this specific group of residents. In addition, in our study, 61.70% of the participants reported previous exposure to plastic surgery during graduation, comparable the percentage reported in a recent international study20. These findings are in accordance with previous data, which report that the proportion of medical schools with plastic surgery in the undergraduate curricula decreased from 78% in 1986 to 13% in 200820. In addition, as many aspects of plastic surgery have been taught in other specialties that overlap within the curricula20, knowledge about the role of plastic surgeons is obscured. This was revealed in a previous study7, which demonstrated that previous exposure to orthopedic or general surgery alone is not sufficient to obtain an understanding of the role of plastic surgeons in hand surgery.
A plastic surgeon can establish a working area only in aesthetic surgery. However, plastic surgery as a skill cannot be restricted and must be understood and disseminated as a field of medicine in constant expansion and evolution, with surgical interventions ranging from aesthetic procedures to reconstructions based on complex microsurgeries, such as hand transplants21. Therefore, the lack of knowledge on the work of plastic surgeons as hand surgeons reported here and in other analyses3-7 suggests the need for educational measures during undergraduate medical courses and residencies3-7,20. Since exposure to hand surgery can positively influence the perception of medical students on hand surgery22, all Brazilian plastic surgeons, the Brazilian Society of Plastic Surgery (SBCP), and all Services accredited by the SBCP should actively participate in this education, with the ultimate goal of improving the overall care provided to patients with any hand disease. In accordance with the proposals in other studies3-7, the education of undergraduate students on plastic surgery should be brief (for example, curriculum rotations in plastic surgery, multidisciplinary events, academic leagues, practical sessions with surgical skills, publication of review articles on plastic surgery in journals related to medical students and residents, among others), but should include a broad overview of the scope of plastic surgery, and should concentrate on areas that are poorly associated with plastic surgery, such as hand surgery, and also on the role of this specialty in the health care system (Single Health System, SUS, Brazil). The media must also be encouraged to disseminate information on the reconstructive role of our specialty17. In addition, as plastic surgeons, Drs. Littler, Peacock, and Buncke, among others, have played a key role in the foundation and development of hand surgery8,9, it is important that all plastic surgeons remember and preserve the rich heritage of these pioneering plastic surgeons, and also contribute to development and advances in hand surgery8. For this reason, it is important that some plastic surgeons become leaders in hand surgery and that medical residency programs in plastic surgery maintain and encourage resident involvement with hand surgery8. Residents must have experience in many aspects of hand surgery23, including, the principles of orthopedic surgery, such as rigid bone fixation, which has been widely used in plastic surgery for treatment of mandible fractures and craniofacial reconstructions8. In addition, residents interested in hand surgery should be encouraged to continue their formal training in this area8, because exposure to hand surgery may increase resident interest in a hand surgery career24. We and others7-9,24 believe that all of these efforts have the potential to increase the recognition of plastic surgeons as hand surgeons, which will also ensure that plastic surgeons continue to contribute to hand surgery and, therefore, have a positive impact in ensuring the permanence of plastic surgery as a specialty with no anatomical or tissue limits1, in addition to maintaining our historic tradition of innovation and leadership in the field of hand surgery. As described in other plastic surgery initiatives25,26, these long-term goals are only possible with the support of all Brazilian plastic surgeons and the SBCP.
Although this study represents the first Brazilian initiative to study the knowledge and perceptions of residents on plastic surgeons as hand surgeons, there are some limitations. As in other analyses6,7, the observations cannot be generalized because only one hospital was assessed. In addition, the perceptions of residents of other Brazilian institutions, as well as the general public, health professionals, medical students, among others, can provide a better overall understanding of perceptions about the practice of plastic surgery in the field of hand surgery in Brazil. We believe that the explanations for the results described here are overlapping; however, we recognize that future studies may elucidate the real reasons for our findings. It is also important to emphasize that our study did not evaluate the full scope of practice of plastic surgeons in the context of hand surgery, although it included the same number of scenarios as the previous study7 that evaluated scenarios related to hand surgery. Despite these limitations, we believe that our data are relevant to Brazilian plastic surgery, because they provide data for a more in-depth discussion on the importance of hand surgery for our specialty, in addition to proposing measures to change the trends discussed in this report. Future research should address our limitations and expand on our findings.
CONCLUSION
The present study demonstrated that Brazilian residents do not perceive plastic surgeons as hand surgeons.
REFERENCES
1. Mast BA. The power of diversification: survival of our specialty. Ann Plast Surg. 2014;72(2):133-4. http://dx.doi.org/10.1097/SAP.0000000000000071. PMid:24374397
2. Carty MJ, Pribaz JJ, Talbot SG, Caterson EJ, Pomahac B. The advent of the restorative plastic surgeon. Plast Reconstr Surg. 2014;133(1):182-6. http://dx.doi.org/10.1097/01.prs.0000436806.35294.e0. PMid:24374677
3. Tanna N, Patel NJ, Azhar H, Granzow JW. Professional perceptions of plastic and reconstructive surgery: what primary care physicians think. Plast Reconstr Surg. 2010;126(2):643-50. http://dx.doi.org/10.1097/PRS.0b013e3181de1a16. PMid:20375766
4. Kumar V, Singh AK, Faisal A, Nandini R. Awareness among medical fraternity regarding the role of plastic surgeon. Indian J Plast Surg. 2011;44(3):494-7. http://dx.doi.org/10.4103/0970-0358.90835. PMid:22279287
5. Panse N, Panse S, Kulkarni P, Dhongde R, Sahasrabudhe P. Awareness and perception of plastic surgery among healthcare professionals in Pune, India: do they really know what we do? Plast Surg Int. 2012;2012:962169. http://dx.doi.org/10.1155/2012/962169. PMid:22685647
6. Agarwal JP, Mendenhall SD, Moran LA, Hopkins PN. Medical student perceptions of the scope of plastic and reconstructive surgery. Ann Plast Surg. 2013;70(3):343-9. PMid:23038146.
7. Agarwal JP, Mendenhall SD, Hopkins PN. Medical student perceptions of plastic surgeons as hand surgery specialists. Ann Plast Surg. 2014;72(1):89-93. http://dx.doi.org/10.1097/SAP.0b013e3182583f3b. PMid:24149406
8. Chang J, Hentz VR, Chase RA. Plastic surgeons in American hand surgery: the past, present, and future. Plast Reconstr Surg. 2000;106(2):406-12. http://dx.doi.org/10.1097/00006534-200008000-00025. PMid:10946941
9. Higgins JP. The diminishing presence of plastic surgeons in hand surgery: a critical analysis. Plast Reconstr Surg. 2010;125(1):248-60. http://dx.doi.org/10.1097/PRS.0b013e3181c496a2c. PMid:20048616
10. Raposo-Amaral CE, Neto JG, Denadai R, Raposo-Amaral CM, Raposo-Amaral CA. Patient-reported quality of life in highestfunctioning Apert and Crouzon syndromes: a comparative study. Plast Reconstr Surg. 2014;133(2):182e-91e. http://dx.doi.org/10.1097/01.prs.0000437260.31693.75. PMid:24469189
11. Raposo-Amaral CE, Raposo-Amaral CA, Garcia Neto JJ, Farias DB, Somensi RS. Apert syndrome: quality of life and challenges of a management protocol in Brazil. J Craniofac Surg. 2012;23(4):1104-8. http://dx.doi.org/10.1097/SCS.0b013e318258814a. PMid:22777480
12. Raposo-Amaral CE, Raposo-Amaral CA. Changing face of cleft care: specialized centers in developing countries. J Craniofac Surg. 2012;23(1):206-9. http://dx.doi.org/10.1097/SCS.0b013e318241ae70. PMid:22337409
13. American Society of Plastic Surgeons - ASPS. 2012 Plastic Surgery Statistics Report [Internet]. Arlington Heights: ASPS; 2012 [cited 2014 Jan 10]. Available from: http://www.plasticsurgery.org.
14. Batista KT, Pacheco LMS, Silva LM. Evaluation of plastic surgery residency programs in Distrito Federal. Rev Bras Cir Plást. 2013;28(1):20-8. http://dx.doi.org/10.1590/S1983-51752013000100005.
15. Gordon CR, Pryor L, Afifi AM, Gatherwright JR, Evans PJ, Hendrickson M, et al. Hand surgery volume and the US economy: is there a statistical correlation? Ann Plast Surg. 2010;65(5):471-4. http://dx.doi.org/10.1097/SAP.0b013e3181d377ac. PMid:20948427
16. Rocha NS, Laureano Filho JR, Silva ED, Almeida RC. Perception of oral maxillofacial surgery by health-care professionals. Int J Oral Maxillofac Surg. 2008;37(1):41-6. http://dx.doi.org/10.1016/j.ijom.2007.07.001. PMid:17881191
17. Reid AJ, Malone PS. Plastic surgery in the press. J Plast Reconstr Aesthet Surg. 2008;61(8):866-9. http://dx.doi.org/10.1016/j.bjps.2008.06.012. PMid:18675242
18. Park AJ, Scerri GV, Benamore R, McDiarmid JG, Lamberty BG. What do plastic surgeons do? J R Coll Surg Edinb. 1998;43(3):189-93. PMid:9654882.
19. Agarwal P. Perception of plastic surgery in the society. Indian J Plast Surg. 2004;37(2):110-4.
20. Mahalingam S, Kalia P, Nagendran A, Oakeshott P. Undergraduate exposure to plastic surgery: the medical student perspective. J Plast Reconstr Aesthet Surg. 2014;67(5):e125-6. http://dx.doi.org/10.1016/j.bjps.2013.12.044. PMid:24444798
21. Landin L. Transplantation and surgery of the hand. Ann Plast Surg. 2014;72(1):1. http://dx.doi.org/10.1097/01.SAP.0000440930.04993.a1. PMid:24343317
22. Smith AA, Duncan SF, Esparra BC. Can brief interventions by hand surgeons influence medical students toward a career in hand surgery? J Hand Surg Am. 2007;32(8):1267-70. http://dx.doi.org/10.1016/j.jhsa.2007.06.004. PMid:17923314
23. Noland SS, Fischer LH, Lee GK, Friedrich JB, Hentz VR. Essential hand surgery procedures for mastery by graduating plastic surgery residents: a survey of program directors. Plast Reconstr Surg. 2013;132(6):977e-84e. http://dx.doi.org/10.1097/PRS.0b013e3182a8066b. PMid:24281644
24. Chung KC, Lau FH, Kotsis SV, Kim HM. Factors influencing residents' decisions to pursue a career in hand surgery: a national survey. J Hand Surg Am. 2004;29(4):738-47. http://dx.doi.org/10.1016/j.jhsa.2004.04.009. PMid:15249103
25. Denadai R, Raposo-Amaral CE. The level of evidence published in a partner journal of plastic and reconstructive surgery: revista brasileira de cirurgia plástica. Plast Reconstr Surg. 2014;133(2):242e-4e. http://dx.doi.org/10.1097/01.prs.0000437232.15553.b2. PMid:24469216
26. Rohrich RJ, Eaves FF 3rd. So you want to be an evidence-based plastic surgeon? A lifelong journey. Plast Reconstr Surg. 2011;127(1):467-72. http://dx.doi.org/10.1097/PRS.0b013e318203a2dd. PMid:21200243
1. MD, Aspiring Member in Training of the Brazilian Society of Plastic Surgery (SBCP), Resident in Plastic Surgery at the Prof. Dr. Cassio M. Raposo Amaral Plastic Surgery Service, Instituto de Cirurgia Plástica Craniofacial, Hospital SOBRAPAR, Campinas, SP, Brazil
2. MD, Full Member of the Brazilian College of Surgeons (CBC) and the Brazilian Society of Vídeosurgery (SOBRACIL), Tutor in the Surgery Department of the Dr. Mario Gatti Municipal Hospital, Campinas, SP, Brazil
3. MD, PhD, Member of the Brazilian Society of Plastic Surgery (SBCP) and the Brazilian Association of Cranio-maxillo-facial Surgery, PhD by the Program by Clinical Surgery of the University of Sao Paulo (USP), Vice-president of the Instituto de Cirurgia Plástica Craniofacial, Hospital SOBRAPAR, Campinas, SP, Brazil
Institution: Work carried out in the Surgery Department of the Dr. Mario Gatti Municipal Hospital and the Instituto de Cirurgia Plástica Craniofacial, SOBRAPAR Hospital, Campinas, SP, Brazil.
Corresponding author:
Rafael Denadai
Hospital de Crânio e Face SOBRAPAR
Av. Adolpho Lutz, 100 - Cidade Universitária
Campinas, SP, Brazil CEP 13083-880; Caixa-postal 6028
E-mail: denadai.rafael@hotmail.com
Article received: March 22, 2014.
Article accepted: July 3, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter