

Original Article - Year 2014 - Volume 29 - Issue 3
Tattoo removal with Q-switched Nd:YAG laser in a Brazilian population
Remoção de tatuagem com laser Q-switched NdYAG em população brasileira
ABSTRACT
INTRODUCTION: Both dermabrasion and surgery have been used in the practice of tattoo removal. Currently, laser is also being used. The aim of this study is to evaluate tattoo removal with Q-switched Nd:YAG laser.
METHOD: This is a retrospective study on patients treated by using Q-switched Nd:YAG laser. The data were collected from medical records and patient photographs, and through phone or e-mail contact. Statistical tests were done through the analysis of distribution, multivariate regression, and logistic regression.
RESULTS: A total of 304 patients with an average age of 29.8 years (±7.86 years) were assessed. Of the total, 297 (97.69%) were classified as white (phototypes I, II, and III), 270 (88.81%) of whom had professional tattoos done. The oldest tattoo was 360 months old and the most recent was 1 month old, with an average of 64.56 months (±63.54 months). The tattoo size was, on average, 12.92 cm, with black being the predominant color (i.e., present in 291 [86.51%] tattoos). The average number of sessions per patient was 3.77 (±2.99), and the interval between sessions was 49.23 days. The therapist observed that 52.96% of the tattoos were partially removed, 21.38% were not removed, 86.51% showed normal healing, 8.55% developed a hypertrophic scar, and 3.29% developed a keloid. Of the 304 patients, 81 (26.64%) reported being satisfied and 179 (58.88%) reported being partially satisfied with the outcome. Hypochromia was present in 102 (33.55%) patients.
CONCLUSIONS: Q-switched Nd:YAG laser is a safe and effective method for tattoo removal that results in a good degree of patient satisfaction and few undesirable effects.
Keywords: Lasers; Tattoo; Nd:YAG Lasers; Scar.
RESUMO
INTRODUÇÃO: Na prática da remoção de tatuagem, já foram utilizadas a dermoabrasão e a cirurgia. Atualmente, se utiliza o laser. O objetivo deste trabalho foi avaliar a remoção de tatuagens utilizando-se o laser Q-switched NdYAG.
MÉTODO: Estudo retrospectivo, com pacientes tratados com laser Q-switched NdYAG. Foram coletados dados a partir de prontuários e fotos dos pacientes, e de contato por telefone ou e-mail. A análise estatística foi feita através da análise de distribuição, regressão multivariada e regressão logística.
RESULTADOS: Foram avaliados 304 pacientes com média de idade de 29,8 anos (±7,86), sendo que 297 (97,69%) foram classificados como brancos (fototipos I, II e III); destes, 270 (88,81%) haviam feito tatuagens profissionais. A tatuagem mais antiga tinha 360 meses e a mais recente, um mês, obtendo-se uma média de 64,56 meses (± 63,54). O tamanho das tatuagens foi, em média, de 12,92 cm, sendo preta a cor predominante, estando presente em 291(86,51%) tatuagens. A média de sessões por paciente foi de 3,77 sessões (±2,99) e o intervalo entre estas foi de 49,23 dias. Com isso, foi observado, pelo terapeuta, que 52,96% das tatuagens foram parcialmente removidas; 21,38%, não removidas; 86,51%, cicatrização normal; 8,55%, cicatriz hipertrófica, e 3,29%, queloide. Dos 304 pacientes, 26,64% (81) relataram estar satisfeitos e 58,88% (179) relataram estar parcialmente satisfeitos com o resultado. A hipocromia esteve presente em 33,55% (102) dos indivíduos.
CONCLUSÕES: O laser Q-switched NdYAG é um método seguro e eficaz, apresentando bom grau de satisfação e poucos efeitos indesejáveis na remoção de tatuagem.
Palavras-chave: Lasers; Tatuagem; Lasers de Nd-YAG; Cicatriz.
The first attempt at tattoo removal occurred >50 years ago1. The technique used in the past was dermabrasion, which involves the nonselective destruction of tissue and may remove the tattoo partially or completely2. Surgical procedure is an old technique that is also currently being used; however, it only shows good results if there is enough skin and if it presents an unfavorable condition, due to the scar as a result of incision3. Intense pulsed light as well as diode and alexandrite lasers, each with its own wavelength, are also current technologies used to remove tattoos4.
The abbreviation LASER means light amplification by stimulated emission of radiation. All laser equipment is composed of an active medium, a light delivery system, and a power source. The active medium, referred to as lasing medium (located inside the optical cavity), is the substance that produces the beam of light and determines the laser wavelength. It can be gaseous, liquid, or solid. The active laser medium Nd:YAG is composed of yttrium-aluminum-garnet and 3% neodymium-doped crystal. The delivery system determines how light will reach the tissue, and the power source is responsible for activating the laser light. After being triggered by the power source, the light beam needs to be distributed to the tissue. The distribution system modifies the laser beam and transports it from the optical cavity to the patient4.
In 1980, the selective photothermolysis process was created to enable the removal of pigments with minimal injury to adjacent tissue5,6. Q-switched lasers feature selective photothermolysis. Each skin chromophore (melanin, water, oxyhemoglobin, and exogenous pigments) has a preference for different absorption wavelengths. The energy absorbed by the chromophore is converted into heat. The smaller the target, the faster the heating would be; therefore, very small structures require rapid heating and smaller pulse duration, i.e., in nanoseconds (ns). The temperature relaxation time is the time required for the target to lose 50% of the heat obtained; that is, the laser exposure time is less than half of the thermal relaxation time, thus ensuring that the damage will be done to the chromophore only5,6.
The removal mechanism occurs from the release of high-power laser beam pulses that have an extremely short duration (ns). This leads to ink fragmentation and formation of acoustic waves due to high temperatures. The propagation of these waves causes the destruction of adjacent structures (chromophore)7,8. The pigment stays in the dermis, within the fibroblasts and macrophages. After exposure to the laser, the production of CO2 and water vapor in the dermis causes bleaching of the skin, which explains the removal of ink in parts. The other part of the pigment will be phagocytized9.
The removal depends on several factors: anatomical location and initial color, and if the color change is permanent or temporary10. The substances that make up the pigment ink will influence the result of the treatment11. Each chemical component is sensitive to a specific wavelength. In addition, the packaged inks used for tattoos include no description of their composition. All these factors result in a removal process that is not 100% guaranteed3. No method of tattoo removal is perfect; however, Q-switched laser is widely used and has been shown to be very effective12.
There are five types of tattoos: professional, amateur, cosmetic, traumatic, and medicated.13-16 There are also three types of commercially used Q-switched lasers: ruby, alexandrite, and Nd:YAG. Each one is more specific to one color than to others. In making the choice of laser to be used, the following factors should also be considered: the patient's skin color, spot size, pulse duration, area, and fluence17,18. In addition to the black pigment, Nd:YAG is very efficient in lightening red, brown, and orange pigments9,10. Yellow and white inks are more resistant, and the therapist may choose to use ablative lasers for these colors3.
There have been studies on Nd:YAG laser; however, in the Brazilian literature, the use of lasers for tattoo removal is scarce. The Brazilian population differs from others in terms of its high intermixing of races, variety of habits and customs, and diverse climate. The aim of this study is to assess tattoo removal in Brazilian patients submitted to sessions of Q-switched Nd:YAG laser treatment.
METHOD
This is a retrospective study of patients seen at the Clínica Leger locations in Porto Alegre and São Paulo, who were treated for tattoo removal with Nd:YAG laser (Palomar, Q-YAG 5 TM; no photo was inserted to avoid conflict of interest). In general, the wavelength used was 1064 nm for black ink removal and 532 nm for the remainder of the colors.
Data were collected by analyzing the medical records and photographs of patients. When necessary, contact with patients was made through phone calls or e-mail. Relevant aspects related to tattoo removal were analyzed, including patient information, tattoo characteristics, and treatment data, such as age, skin phototype, tattoo time, size, color, type, number of sessions, interval between sessions, the therapist's opinion and the patient's satisfaction in relation to the result, in addition to healing, hypochromia, and use of isotretinoin (which is a contraindication for laser if used in the 6 months before treatment).
The degree of patient satisfaction in relation to the treatment outcome was measured by using the Likert scale19.
Tattoo size was divided into four groups: small (1-3 cm), medium (3-6 cm), large (6-10 cm), and extra-large (>10 cm). The measurements were made by using the major axis of the tattooed area.
The phototype was defined, according to the Fitzpatrick scale, as white (phototypes I, II, and II) and black (phototypes IV, V, and VI)20.
The therapist's opinion was collected and was based on the last tattoo photograph. The tattoo was considered to have been removed when no pigment could be observed.
The interval between sessions for each patient was defined through the mean of interval days from one session to the next.
The use of isotretinoin was considered for the previous 6 months before starting the treatment.
The aspect of the skin after the tattoo removal was considered according to the coloring (normal, hyperchromic, or hypochromic) and healing (normal, atrophic, hypertrophic, or keloid) of the skin.
Statistical analysis was conducted through a multivariate regression analysis to quantify the data, except for the Likert scale analysis in which logistic regression and percentage distribution were used.
The inclusion criteria were as follows: patients seen at the Clínica Leger locations in Porto Alegre and São Paulo, treated for tattoo removal with Nd:YAG laser, who signed an informed consent form and received treatment from January 2008 to April 2012.
The exclusion criteria were as follows: patients who have cognitive impairment, abandoned treatment, started the tattoo removal treatment at a different clinic, have other nationalities, use substances that could influence the color of the skin, and had incomplete data.
The research project was approved by the Research Ethics Committee of the Institute of Cardiology of Rio Grande do Sul, under number 052012.
RESULTS
A total of 304 patients were assessed, 181 (59.53%) women and 123 (40.46%) men, with a mean age of 29.8 years (±7.86 years). In relation to the phototype, 297 (97.69%) persons were classified as white (phototypes I, II, and III) and 7 as black (phototypes IV, V, and VI).
Concerning the tattoo types, 272 (89.48%) were professional, 23 (7.57%) amateur, 8 (2.63%) aesthetic, and 1 (0.32%) traumatic. The oldest tattoo was 360 months old and the most recent was 1 month old, with an average of 64.56 months (±63.54 months). The average size of the tattoos was 12.92 cm. The predominant color was black, present in 291 [95.72%] tattoos, followed by red in 89 (29.27%), blue in 64 (21.05%), green in 58 (19.07%), yellow in 53 (17.43%), orange in 12 (3.94%), purple in 11 (3.61%), white in 9 (2.96%), pink in 8 (2.63%), brown in 2 (0.65%), and "other" in 1 (0.32%).
The average number of sessions per patient was 3.77 (±2.99); the highest number of sessions in a single patient was 16, whereas the least number of sessions was 1. Some patients still underwent treatment after the first tattoo removal session, whereas others abandoned the treatment. The average interval between sessions was 49.23 days.
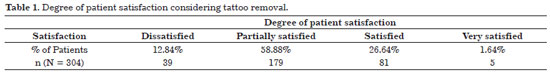
According to the therapist's assessment, 170 (55.92%) of the tattoos were partially removed (Figure 1), 69 (22.70%) were removed (Figure 2), and 65 (21.38%) were not removed. Concerning healing, 263 (86.51%) showed normal scarring, 26 (8.55%) showed hypertrophic scarring, and 10 (3.29%) showed keloid scarring. Hypochromia was present in 102 (33.55%) of patients and only 12.84% of patients were dissatisfied with the treatment (Table 1).

Figure 1. (A) Initial tattoo (before). (B) Partially removed tattoo with hypochromic areas (after).

Figure 2. (A) Initial tattoo (before). (B) Fully removed tattoo (after).
Of the patients assessed, five had undergone a previous tattoo removal treatment with intense pulsed light therapy and four had used other procedures. Of those who completed the tattoo removal treatment with Q-switched Nd:YAG laser, 14 underwent at least one fractional CO2 laser session after completing the removal. Clinically, it was observed that colorful tattoos showed hypochromia after being treated with Q-switched Nd:YAG laser at a wavelength of 532 nm.
DISCUSSION
YAG laser presents good results in the removal of the black pigment. Its advantage over the ruby laser is that, by having a 1064-nm wavelength, it protects the epidermis and has minor adverse effects, such as bubbling and hypochromia. It is therefore more suitable for higher phototypes21. In this study, 95.72% of the tattoos were black, which may justify why most tattoos (239 of 304) were considered by the assessor as removed or partially removed (78.62%). Kilmer et al.22 treated 39 tattoos by using Q-switched Nd:YAG laser; of these, 77% had black pigment and the removal of ink was obtained in 77% of the tattoos. These data are similar to those found in this study. Many of the patients assessed were still undergoing treatment or abandoned the treatment after the first few sessions, which can be the reason behind the highest rates of partially removed tattoos and partially satisfied patients.
Zelickson et al., while comparing the Nd:YAG, alexandrite and ruby lasers, examined the pigments histopathologically and noticed a better response in relation to the removal of red, brown, and orange inks, with Nd:YAG. In this study, red was found to be the second most prevalent color in tattoos, which was also sensitive to the same Nd:YAG laser used by Zelickson et al. The alexandrite laser was more effective in removing green and blue inks, and ruby was better in removing purple and violet inks. In addition, in relation to the black pigment, the efficacy of all lasers was equivalent9.
In another study, artificial skin in vitro (by using water and gelatin) was used with 21 tattoos in red, orange, pink, brown, yellow, blue, and green. Moreover, an in vivo model was used with two tattoos in red and pink. After removing the pigments from the artificial skins, morphological analyses were performed on the irradiated areas. The in vitro and in vivo tattoo models responded with similar efficacy. The authors realized that more than three pulses and very high fluencies could darken the ink. With smaller pulses, there are no bubbles or scars, and the interval time between sessions is 2 weeks. Fluences between 0.7 and 1.6 J/cm2 were more effective than 9.0 and 12 J/cm2.23
Of the 304 patients assessed, 102 (33.55%) presented hypochromia and 263 (86.51%) showed normal scarring. In addition to the predominant low phototypes (I, II, and II), another factor that may have influenced the low rate of hypopigmentation is the fact that most of the tattoos were treated with the 1064-nm wavelength, owing to the high prevalence of the black tattoos. It is known that longer wavelengths can protect the skin, whereas shorter pulses, such as 532 nm, can increase the absorption of melanin, which can lead to hypopigmentation21,24. This fact was also observed in this study, as the colored tattoos showed hypochromia after being irradiated with the Q-switched Nd:YAG laser at 532-nm wavelength.
Selective photothermolysis is known to protect the skin, as pulses with lasers in nanoseconds reach only very small structures such as ink particles6. When tattoos are treated with pulse durations in the range of milliseconds or with continuous lasers, heat is not limited to the target. Such heat transfer causes a nonspecific destruction of the surrounding tissue and can result in subsequent scarring25.
Scheibner et al. treated 163 tattoos, of which 101 were amateur and 62 were professional tattoos. Each tattoo received three Nd:YAG laser sessions. The amateur tattoos were observed to respond better to treatment26. In this study, 23 amateur and 272 professional tattoos were treated with satisfactory results.
There were no cases of anaphylaxis, as referenced by Sacks & Barcaui.27.
Furthermore, concerning the absorption spectrum of lasers, in particular the 532-nm (as used in this study) and 752-nm wavelengths, Beute et al.28 tested the effect of irradiation on 28 pigments and black from India, mixed into agar plates and analyzed spectrophotometrically. They observed that the highest absorption of red was in a complementary spectrum, whereas blue, yellow, and orange had their absorption peaks close to the spectrum of visible light. A large variation was observed in the absorption of the green pigment. Darkening of the pigment was observed in the two wavelengths tested, in all of the pigments containing iron, except black. There was some variation in pigments containing titanium. The pigments lightened or darkened in response to the 532-nm wavelength; however, the response was more limited at 752 nm. The absorption spectrum of the pigments can explain why some tattoo colors are more resistant to laser removal, as also observed in this study. The 1064-nm Nd:YAG laser, which decreased adjacent skin lesion and treated black tattoos better, was also used. Thus, no epidermal debris or darkening of the ink was observed, as in the report by Choudhary et al.29.
CONCLUSION
Treatment with Q-switched Nd:YAG laser is a safe and effective method of tattoo removal that results in a good degree of patient satisfaction and few undesirable effects.
REFERENCES
1. Manchester GH. Tattoo removal. A new simple technique. Calif Med. 1973;118(3):10-2. PMid:4689534.
2. Bernstein EF. Laser tattoo removal. Semin Plast Surg. 2007;21(3):175-92. http://dx.doi.org/10.1055/s-2007-991186. PMid:20567669
3. Kent KM, Graber EM. Laser tattoo removal: a review. Dermatol Surg. 2012;38(1):1-13. http://dx.doi.org/10.1111/j.1524-4725.2011.02187.x. PMid:22092752
4. Jedwab S. Laser e Outras Tecnologias na Dermatologia. 1st ed. Santos: Editora Santos; 2010.
5. Anderson RR, Parrish JA. Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med. 1981;1(3):263-76. http://dx.doi.org/10.1002/lsm.1900010310. PMid:7341895
6. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524-7. http://dx.doi.org/10.1126/science.6836297. PMid:6836297
7. Graber E, Iyengar V, Rohrer T, Arndt K. Laser treatment of tattoos and pigmented lesions. In: Robinson JK, Hanke CW, Siegel DM, Fratila A, editores. Surgery of the Skin: Procedural Dermatology. 2nd ed. China: Mosby; 2010. p. 537-48. http://dx.doi.org/10.1016/B978-0-323-06575-7.00032-8.
8. Ara G, Anderson RR, Mandel KG, Ottesen M, Oseroff AR. Irradiation of pigmented melanoma cells with high intensity pulsed radiation generates acoustic waves and kills cells. Lasers Surg Med. 1990;10(1):52-9. http://dx.doi.org/10.1002/lsm.1900100112. PMid:2308465
9. Zelickson BD, Mehregan DA, Zarrin AA, Coles C, Hartwig P, Olson S, et al. Clinical, histologic, and ultrastructural evaluation of tattoos treated with three laser systems. Lasers Surg Med. 1994;15(4):364-72. http://dx.doi.org/10.1002/lsm.1900150406. PMid:7885170
10. Anderson RR, Geronemus R, Kilmer SL, Farinelli W, Fitzpatrick RE. Cosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatment. Arch Dermatol. 1993;129(8):1010-4. http://dx.doi.org/10.1001/archderm.1993.01680290082012. PMid:8352605
11. Stafford TJ, Lizek R, Boll J, Tan OT. Removal of colored tattoos with the Q-switched alexandrite laser. Plast Reconstr Surg. 1995;95(2):313-20. http://dx.doi.org/10.1097/00006534-199502000-00011. PMid:7824611
12. Burris K, Kim K. Tattoo removal. Clin Dermatol. 2007;25(4):388-92. http://dx.doi.org/10.1016/j.clindermatol.2007.05.011. PMid:17697922
13. Choudhary S, Elsaie ML, Leiva A, Nouri K. Lasers for tattoo removal: a review. Lasers Med Sci. 2010;25(5):619-27. http://dx.doi.org/10.1007/s10103-010-0800-2. PMid:20549279
14. Fitzpatrick RE, Lupton JR. Successful treatment of treatment-resistant laser-induced pigment darkening of a cosmetic tattoo. Lasers Surg Med. 2000;27(4):358-61. http://dx.doi.org/10.1002/1096-9101(2000)27:4<358::AID-LSM9>3.0.CO;2-0. PMid:11074513
15. Spear SL, Arias J. Long-term experience with nipple-areola tattooing. Ann Plast Surg. 1995;35(3):232-6. http://dx.doi.org/10.1097/00000637-199509000-00002. PMid:7503514
16. Moreno-Arias GA, Casals-Andreu M, Camps-Fresneda A. Use of Q-switched alexandrite laser (755 nm, 100 nsec) for removal of traumatic tattoo of different origins. Lasers Surg Med. 1999;25(5):445-50. http://dx.doi.org/10.1002/(SICI)1096- 9101(1999)25:5<445::AID-LSM12>3.0.CO;2-Q. PMid:10602138
17. Levine VJ, Geronemus RG. Tattoo removal with the Q-switched ruby laser and the Q-switched Nd:YAG laser: a comparative study. Cutis. 1995;55(5):291-6. PMid:7614841.
18. Al-Mutairi N, Manchanda Y, Almutairi L. Tattooing in the Gulf region: a review of tattoo practices and response to treatment with the Q-switched ruby laser. J Cosmet Laser Ther. 2010;12(3):132-7. http://dx.doi.org/10.3109/14764170903463944. PMid:20141342
19. Coutinho CP. Metodologia de investigação em educação - texto de apoio: escalas de medida de variáveis. Braga: Universidade do Minho; 2006.
20. Guirro E, Guirro R. Fisioterapia dermatofuncional. 3rd ed. São Paulo: Manole; 2004.
21. Jones A, Roddey P, Orengo I, Rosen T. The Q-switched ND:YAG laser effectively treats tattoos in darkly pigmented skin. Dermatol Surg. 1996;22(12):999-1001. http://dx.doi.org/10.1111/j.1524-4725.1996.tb00651.x. PMid:9078310
22. Kilmer SL, Lee MS, Grevelink JM, Flotte TJ, Anderson RR. The Q-switched Nd:YAG laser effectively treats tattoos. A controlled, dose-response study. Arch Dermatol. 1993;129(8):971-8. http://dx.doi.org/10.1001/archderm.1993.01680290043007. PMid:8352621
23. Gómez C, Martin V, Sastre R, Costela A, García-Moreno I. In vitro and in vivo laser treatments of tattoos: high efficiency and low fluences. Arch Dermatol. 2010;146(1):39-45. http://dx.doi.org/10.1001/archdermatol.2009.321. PMid:20083691
24. Ho WS, Ying SY, Chan PC, Chan HH. Use of onion extract, heparin, allantoin gel in prevention of scarring in Chinese patients having laser removal of tattoos: a prospective randomized controlled trial. Dermatol Surg. 2006;32(7):891-6. PMid:16875470.
25. Anderson RR. Dermatologic history of the ruby laser: the long story of short pulses. Arch Dermatol. 2003;139(1):70-4. http://dx.doi.org/10.1001/archderm.139.1.70. PMid:12533169
26. Scheibner A, Kenny G, White W, Wheeland RG. A superior method of tattoo removal using the Q-switched ruby laser. J Dermatol Surg Oncol. 1990;16(12):1091-8. http://dx.doi.org/10.1111/j.1524-4725.1990.tb00018.x. PMid:2262615
27. Sacks T, Barcaui C. Laser e luz pulsada de alta energia: indução e tratamento de reações alérgicas relacionadas a tatuagens. An Bras Dermatol. 2004;79(6):709-14. http://dx.doi.org/10.1590/S0365-05962004000600007.
28. Beute TC, Miller CH, Timko AL, Ross EV. In vitro spectral analysis of tattoo pigments. Dermatol Surg. 2008;34(4):508-15, discussion 515-6. PMid:18248489.
29. Choudhary S, Elsaie ML, Leiva A, Nouri K. Lasers for tattoo removal: a review. Lasers Med Sci. 2010;25(5):619-27. http://dx.doi.org/10.1007/s10103-010-0800-2. PMid:20549279
1. MD, General Surgeon, Standing Member of the Brazilian Society for Laser (SBL) and the American Society for Laser Medicine and Surgery (ASLMS), Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
2. MD, Member of the Brazilian Society for Laser (SBL) and the American Society for Laser Medicine and Surgery (ASLMS), Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
3. MD, PhD, Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
4. Physical Therapist, Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
5. MD, Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
6. MD, Member of the Brazilian Society of Dermatology (SBD), Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
7. Scholarship Student, Member of the Leger Research Center, Clínica Leger, Porto Alegre, RS, Brazil
Institution: Study conducted at Clínica Leger, Porto Alegre, RS, Brazil.
Corresponding author:
Roberto Chacur
Avenida dos Flomboyantes, 155, bloco 004, apto. 1103
Rio de Janeiro, RJ, Brazil CEP 22776-070
Tel.: (21) 8425-7310
E-mail: chacurmd@hotmail.com
Article received: November 26, 2013.
Article accepted: August 3, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter