

Original Article - Year 2014 - Volume 29 -
Mammoplasty after massive weight loss
Mamoplastia após grande perda ponderal
ABSTRACT
INTRODUCTION: After massive weight loss, patients present with various mammary changes, such as sagging, different grades of ptosis, and empty upper pole. Different mammoplasty techniques are used to shape the mammary cone and to reposition the nipple-areolar complex (NAC). In this study, we evaluate how different surgical approaches can satisfy the requirements of each patient.
METHOD: Twenty-five patients who underwent mammoplasty following gastroplasty were analyzed. The mammoplasty techniques used were (1) mastopexy without implant with inferior flap; (2) mastopexy without implant with inferior areolar pedicle; (3) mastopexy with implant and coverage by inferior flap; (4) mastopexy with implant and plication of cross flaps (jacket procedure).
RESULTS: The average body mass index (BMI) before mammoplasty was 26.6 (ranging from 21.6 to 31.2). All patients who underwent this surgery rated the outcome obtained as good or great. In an evaluation carried out by an observer unaware of the techniques employed, the results obtained were considered to be satisfactory for breast shape, correction of breast ptosis, and filling of the upper pole. One patient who underwent mastopexy with implants and cross flaps developed seroma and subsequent capsular contracture, which required capsulectomy. Eight patients developed unilateral dehiscence: seven at the junction of skin flap in the inframammary fold, and one vertically, which were resolved with healing by secondary intention. No cases of necrosis or NAC epitheliosis were observed.
CONCLUSION: Using different mammoplasty techniques, which were personalized and analyzed on a case-by-case basis, good outcomes and a high level of patient satisfaction were achieved. Various factors, such as the furcula-papilla distance, the need to lift the NAC, pre-mammoplasty breast volume and the patient's desire to increase breast volume, influence the choice of the surgical technique.
Keywords: Body contour; Massive weight loss; Mastopexy; Mamomplasty.
RESUMO
INTRODUÇÃO: Após perda ponderal maciça, as pacientes apresentam alterações mamárias, como flacidez, ptose em graus variados e polo superior vazio. Diferentes técnicas de mamoplastia são empregadas para dar forma ao cone mamário e reposicionar o complexo aréolo-papilar (CAP). Neste trabalho, avaliamos diferentes abordagens cirúrgicas preenchendo as necessidades de cada caso.
MÉTODO: Vinte e cinco pacientes submetidas à gastroplastia antes da mamoplastia foram analisadas. As técnicas utilizadas foram (1) mastopexia sem prótese e retalho inferior; (2) mastopexia sem prótese e pedículo areolado inferior; (3) mastopexia com prótese com cobertura pelo retalho inferior;
(4) mastopexia com prótese com plicatura de retalhos cruzados (jaquetão).
RESULTADOS: A média do IMC antes da mamoplastia foi de 26,6 (variando de 21,6 a 31,2). Todas as pacientes submetidas à cirurgia consideraram o resultado bom ou ótimo. Em avaliação por observador cego às técnicas empregadas, os resultados foram considerados bons com relação à forma da mama, correção da ptose e preenchimento do polo superior. Uma paciente submetida à mastopexia com prótese com retalhos cruzados apresentou seroma e contratura capsular subsequente, necessitando capsulectomia. Oito pacientes apresentaram deiscências: sete, na junção dos retalhos cutâneos no sulco inframamário, e uma na vertical, unilateralmente, resolvidas por cicatrização por segunda intenção. Não houve caso de necrose ou epiteliólise do CAP.
CONCLUSÃO: Empregando-se diferentes técnicas de mamoplastia, individualizadas caso a caso, foram obtidos resultados agradáveis, alcançando satisfação das pacientes. Fatores, como distância fúrcula-papila, necessidade de elevação do CAP, volume mamário pré-mamoplastia e desejo de aumento de volume pela paciente, influenciam a escolha da técnica cirúrgica.
Palavras-chave: Contorno corporal; Perda ponderal maciça; Mastopexia; Mamoplastia.
Bariatric surgery has become more common as a treatment for obesity. After bariatric surgery, patients show a rapid weight loss and an improvement in obesity-related comorbidities. The weight loss stabilizes at around 12 to 24 months after bariatric surgery1. As a result of the weight loss presented by these patients, increased skin folds are also observed. The redundant skin and subcutaneous tissue interferes with the wearing of clothes, physical and sexual activity, and hygiene, and can lead to recurrent infections. Therefore, a higher demand for plastic surgeries by these patients in the search for a better quality of life has been noticed.
In the postoperative period, women who have undergone bariatric surgery present with sagging breasts and ptosis, with empty and flat upper poles2-6. The appearance of the breast after weight loss varies greatly between one patient and the other. Therefore, many techniques can be employed, and the surgical indications should be analyzed according to each case. The treatment of breast cancer in patients that have experienced massive weight loss, either after bariatric surgery or through diet, requires filling the breast volume with autologous tissue or implants and repositioning the nipple-areolar complex (NAC).
Post-bariatric breasts can be classified according to the Pittsburgh rating scale7 and addressed as follows:
0- Normal - No treatment needed.
1- Moderate ptosis (grade I/II) or severe macromastia - mastopexy with increased or decreased volume, depending on the case.
2- Significant ptosis (grade III) or moderate volume loss - mastopexy with or without increased volume, depending on the case and patient's desire.
3- Significant ptosis, presence of lateral folds, large skin sagging and loss of breast volume -parenchyma remodeling and auto-augmentation.
Type 1, depending on the patient, requires mastopexy with increased or decreased volume.
In type 2, mastopexy with a Liacyr type 1 flap and suspension of the superiorly pedicled NAC provides highly satisfactory results2. This technique can be performed in conjunction with breast implant inclusion when the patient wants to increase the breast size.
Mansur and Bozola8 described a technique using the inferior pedicle flap to cover the implant in cases of mastopexy with prosthesis. Supporting the implant in the inferior inframammary fold prevented its sliding down the groove and the emptying of the breast cone, in addition to providing better protection for the prosthesis. Garcia et al.9 reported that the inferior flap reduces the weight effect of the implant on the skin, thus contributing to prevent ptosis recurrence and implant extrusion.
Resende and Fiorelli10 use the transverse bipedicled flap to protect the prosthesis against the extrusion.
In case of breast implant inclusion, plication of medial and lateral cross flaps (jacket procedure) likewise enables protection of the implant. The parenchymal plication technique also aids in preventing premature ptosis11.
In patients presenting with grade III ptosis, with the NAC well below the inframammary fold in addition to large amounts of sagging skin and breast volume loss (type 3 in Pittsburgh's rating scale), techniques for NAC repositioning should be considered. Among these techniques, inferior areolar pedicle, type 512 or superior-medial pedicle can be used5,13.
Massive weight loss following bariatric surgery usually results in breast volume loss and inelastic skin. This combination is challenging to treat, and requires special treatment to maintain breast shape over time. The two most important points in the initial management of these patients are to understand the deformities they present with and to establish treatment goals. Some authors state that traditional mastopexy techniques are often inadequate in patients presenting massive weight loss, due to the extent of the deformity, lack of structural support, and volume and lack of elasticity in the skin11,14. A single technique is not sufficient to address the different breast volumes that can be observed after massive weight loss.
OBJECTIVES
This study aims to evaluate the results of different mammoplasty techniques in patients after massive weight loss and to consider factors that may influence the choice of a particular technique.
METHODS
A total of 25 female patients, undergoing mammoplasty between November 2010 and July 2013, were included in the study.
All patients were submitted to a preoperative breast examination to exclude possible malignancies.
The maximum weight reached, BMI before bariatric surgery, BMI before mammoplasty and total weight loss were the parameters considered. As criteria for patients to undergo plastic surgery, the procedure should be performed at least 18 months after bariatric surgery and the patient should have maintained a stable weight for at least six months.
The techniques that were used were:
Group 1) Mastopexy without prosthesis, with superior pedicled NAC and inferior flap (Liacyr Ribeiro type 1 flap).
Group 2) Mastopexy without prosthesis with inferior areolar pedicle (type 5 flap).
Group 3) Mastopexy with prosthesis, superior pedicled NAC and coverage of the prosthesis with the inferior flap (Liacyr Ribeiro type 1 flap).
Group 4) Mastopexy with prosthesis, superior pedicled NAC and plication of medial and cross lateral flaps (jacket procedure).
Surgical Technique:
Marking: in all patients, the sternal notch, midline, breast meridians and inframammary folds were marked. The position of point A was determined by the Pitanguy Maneuver.
Points B and C were marked by the bimanual maneuver and their extensions to the inframammary fold were also defined in patients in whom a breast prosthesis was not included.
Where the Liacyr type 1 flap was used, this was designed with a base of 4 cm when used in conjunction with a prosthesis and from 5 to 6 cm, in cases in which it was used separately. Its thickness was 2 cm or more.
When we used the type 5 flap (inferior areolar flap), the base used was 8 to 10 cm depending on the degree of sagging, to maintain a maximum connection with the pectoral muscles up to the areola (Figure 1).
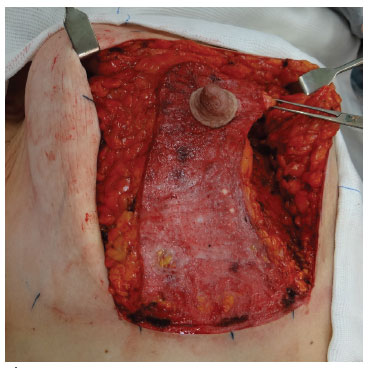
Figure 1. Inferior areolar flap.
In patients in whom an implant was inserted with a jacket plication, the incision was carried out vertically, in the meridian between the areola and the inframammary fold. After the detachment of the subglandular plane, the drain and implant were placed. Medial and lateral flaps of mammary parenchyma were generated in the inferior pole and separated by medial and lateral skin flaps (Figure 2). Skin resection was carried out only after the plication of medial and lateral flaps to the implant (Figures 3 and 4).
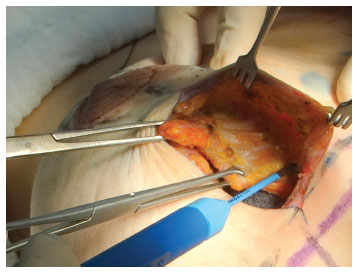
Figure 2. Generation of a medial flap from the breast parenchyma, separating it from the skin flap.
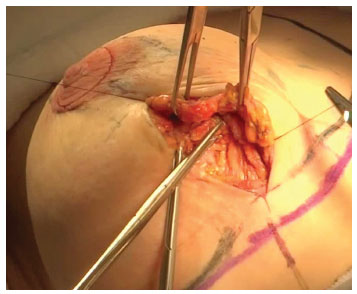
Figure 3. Plication of the lateral flap on the posterior face of the medial flap covering the prosthesis.

Figure 4. Plication of the medial flap on the anterior face of the lateral flap covering the prosthesis.
Prostheses were placed in the subglandular plane in all patients in whom they were used.
A portovac 3.2 drain was used for patients undergoing mastopexy with prosthesis, and a Penrose drain was used for patients undergoing mastopexy without prosthesis.
The patients were hospitalized for one to two days and instructed to use a postoperative bra for two months.
To evaluate the results, we considered the level of patient satisfaction and assessment by an observer unaware of the techniques that were employed, assessed through a scale varying from 1 to 4 (1- bad, 2- satisfactory, 3- good, 4- great).
RESULTS
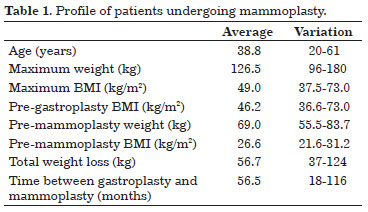
Mammoplasty was performed, on average, 56 months after gastroplasty (range 18 to 116 months). The average age was 38.8 years old (range 20 to 61 years) and average BMI before mammoplasty was 26.6 kg/m2 (range 21.6 to 31.2 kg/m2) (Table 1).
In Group 1 (mastopexy without prosthesis with type 1 flap) five patients were included (Figure 5). In Group 2 (mastopexy without prosthesis with inferior areolar pedicle) four patients were included (Figures 6 and 7). In Group 3 (mastopexy with prosthesis and type 1 flap) four patients were included (Figures 8 and 9). In Group 4 (mastopexy with prosthesis and plication of cross flaps) 12 patients were included (Figures 10 and 11).

Figure 5. Pre and post-operative aspects of the patient submitted to mastopexy with type 1 flap without prosthesis inclusion.

Figure 6. Pre and post-operative aspects of the patient submitted to mastopexy with inferior areolar flap without prosthesis inclusion.

Figure 7. Pre and post-operative aspects of the patient submitted to mastopexy with inferior areolar flap without prosthesis inclusion.

Figure 8. Pre and post-operative aspects of the patient submitted to mastopexy with prosthesis with type 1 flap coverage.
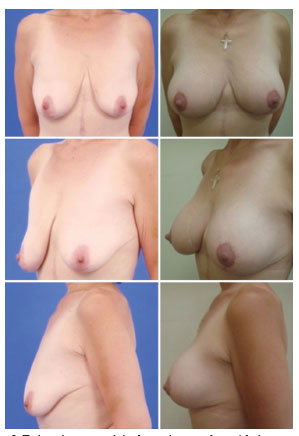
Figure 9. Pre and post-operative aspects of the patient submitted to mastopexy with prosthesis with type 1 flap coverage.

Figure 10. Pre and post-operative aspects of the patient submitted to mastopexy with prosthesis and plication of cross flaps.

Figure 11. Pre and post-operative aspects of the patient submitted to mastopexy with prosthesis and plication of cross flaps.
The volume of breast implants used was, on average, 255 cc, varying from 225 cc to 300 cc.
The patients were followed up for at least six months.
All patients reported that the result obtained was good or great, with improved self-esteem and quality of life following surgery.
In the evaluation carried out by the observer unaware of the techniques employed, the results were considered good, especially regarding the breast shape, ptosis correction and upper pole filling.
Seven patients (three from Group 1, two from Group 2 and two from Group 4) presented with dehiscence in the T-junction of the skin flap in the inframammary fold, and one patient (from Group 1) with unilateral vertical dehiscence, which were all healed by secondary intention.
One patient from Group 4 developed seroma with subsequent capsular contracture, thus needing capsulectomy.
One patient from Group 3 developed unilateral hematoma on the first postoperative day, which was immediately drained in the surgical center, with no other adverse complications arising after drainage.
No cases of necrosis or NAC epitheliosis were observed. Scar enlargement was observed in three patients, who underwent healing by secondary intention; other types of unaesthetic scars were not observed.
DISCUSSION
Ptosis and volume loss are the main problems to be corrected in breasts after massive weight loss15. Patients may present with different degrees of deformities, measured according to the Pittsburgh scale, which are difficult to correct with a single technique. Several surgical approaches can be employed and these should be personalized, on a case-by-case basis.
According to Migliori et al.15, the amount of breast tissue determines the choice of the surgical technique to be employed. If the existing volume is considered sufficient by the patient and the surgeon, breast remodeling should be performed. Mammoplasty with autologous breast tissue is an alternative for patients who do not want any implants16.
In patients who are satisfied with their breast volume and who do not want prosthesis implantation, an excellent technique is the inferior flap (Liacyr type 1)2. The inferior flap acts as a natural prosthesis, being anchored to the fascia of the pectoralis major muscle. This increases breast projection and fills the usually loose and empty upper pole, in addition to reducing the breast base through an inferior pole central tissue transposition16. The volume of the inferior flap depends on the distance between the areola and inframammary fold.
In the patients operated on, the inferior flap was associated with the superior pedicle by the areola, allowing very satisfactory results to be obtained with upper pole filling and breast projection, with a minimal complication rate. Few complications were observed, including dehiscence at the intersection of the skin flaps. No cases of necrosis or NAC epitheliosis were observed.
Compared with the lateral flap used for breast auto-augmentation, which offers limited recruitment of tissue17, the inferior flap is designed to give a better breast shape, with upper pole filling and a bigger volume16.
The choice of the pedicle for NAC depends on several factors, such as the grade of hypertrophy and ptosis, NAC position, and age of the patient. Bonomi et al.13 use the supero-medial pedicle if the NAC needs to be lifted more than 8 cm.
In patients in whom the NAC needed to be lifted less than 8 cm, the superior pedicle was used for the areola, whereas for patients requiring an elevation of more than 8 cm the inferior pedicle flap was used.
The choice of using the inferior pedicle for the areola rather than the supero-medial pedicle was based on the personal experience of the surgeon with this technique. In patients operated on with the type 5 flap technique, in addition to the large sterno-papilla distance the main characteristics were the lack of upper pole filling and poor projection of the mammary cone. The type 5 flap was fixed in its middle portion to the pectoral muscle. The mounting of the mammary parenchyma (lateral and medial pillars) on to the flap allowed a reasonable projection of the breast cone. In patients in whom the NAC needed to be lifted more than 8 cm, the inclusion of prosthesis in the same operation was avoided, as this would risk compression of the pedicle of the inferior areolar flap and NAC impairment. However, the four patients who this applied to were satisfied with their breast volume and shape, and rejected a second procedure to place the implant when this was proposed in the late postoperative period. According to several authors, in cases of extremely long and deflated breasts with grade III ptosis, a safer option is to perform first the mastopexy and then place the prosthesis, if this is desired by the patient, in a second surgery11,14. Due to the great amount of volume loss and reduction of the breast ligamentous support, the long length of the pedicle increases the risks of performing a single surgery, as proper planning is required to ensure that NAC perfusion is maintained14. The patients reported that NAC sensitivity is preserved after surgery. However, due to the small number of cases (only four cases were operated on with the inferior areolar pedicle), an objective evaluation to measure sensitivity was not carried out.
In cases of volume loss and less pronounced NAC ptosis when the areola could be lifted by the superior pedicle and the patient wanted to increase the volume, we chose to perform mastopexy with prosthesis in a single surgery.
In the ptotic breast with poor tissue in the upper pole of the breast, a partial or total retropectoral plane provides the additional coverage necessary for the prosthesis superiorly18,19. However, this increases the risk of double-bubble deformities. This deformity is the result of the sliding of the parenchyma inferiorly, below the pectoral muscle and the prosthesis19. Therefore, we decided to use the subglandular plane.
The type of implant used (round or anatomical) basically depends on the type of aesthetic defect: upper pole defects require round implants, and lower pole defects anatomical implants15. All implanted patients in this case series received round implants due to an empty upper pole, this being one of the main complaints.
The inferior flap as coverage for breast implant was chosen for patients with a greater degree of sagging and a distance between the inferior edge of the areola and the inframammary fold of 8 cm or more, which was enough to allow the subsequent fixation of the flap to the breast parenchyma along with the NAC. In these cases, a flap was generated with 4 cm of base, sufficient to protect the prosthesis and avoid cutaneous tension after its inclusion.
According to some authors9,18, the use of the inferior flap allows an increase in the distance between the implant and the suture lines, minimizing the implant weight on the skin and contributing to prevent recurrent ptosis, implant extrusion, and skin irregularities. These authors use the submuscular plane for prosthesis inclusion in patients after massive weight loss.
Mansur and Bozola8, in cases of mastopexy with prosthesis using the inferior flap to cover the implant placed in the subglandular plane, noted that patients who had previously undergone bariatric surgery showed a progressive ptosis after one year. We also observed this occurrence among patients operated on with this technique. However, these patients were satisfied with the shape and breast projection during the follow-up period.
In patients who wanted to increase the breast volume and who had a shorter distance between the lower edge of the areola and the inframammary fold, a plication of cross flaps (jacket procedure) was carried out. In this technique, the amount of skin to be excised is determined after prosthesis inclusion, which aids in preventing tension on the sutures and the skin. Plication of the inferior pole acts as an internal support to reduce recurrent ptosis11.
Mammoplasty techniques in patients after massive weight loss should be more based on glandular manipulation for shape preservation rather than on the cutaneous envelope. These techniques include parenchyma plication, suspension and auto-augmentation, favoring the maintenance of breast shape and symmetry11.
Complications in mammoplasty are uncommon and include prolonged healing, unsightly scarring, seroma, hematoma, infection, necrosis and NAC loss11.
The complications presented following the operations were hematoma (one patient, unilaterally); seroma, with capsular contracture (one patient, unilaterally), and skin dehiscence, which was healed by secondary intention.
Scar enlargement was observed in three patients, and healed by secondary intention. Other types of unsightly scars were not observed among the patients operated. De la Plaza20 reports that the satisfaction of the patient after mammoplasty is related to her subjective perception about the quality of the scar. This may have contributed to the satisfaction of the patients of this series with their outcomes result.
Early ptosis observed in patients undergoing mastopexy after bariatric surgery is more common when using implants11, as found in our series. However, the patients were satisfied with the result and a second surgery to improve this outcome was not required for any patient.
Due to the great diversity in the presentation of breast cases after massive weight loss, there is no mastopexy technique that can be used to correct all deformities.
CONCLUSION
Using different techniques of mammoplasty on a personalized, case-by-case basis, results were obtained which were satisfactory to both patients and surgeons. Factors such as the furcula-papilla distance, need to lift the NAC, pre-mammoplasty breast volume, and patient's desire for an increased breast volume, should influence the choice of the surgical technique.
REFERENCES
1. Hubbard VS, Hall WH. Gastrointestinal surgery for severe obesity. Obes Surg. 1991;1(3):257-65. PMid:10775921
2. Modolin M, Cintra W Jr, Silva MM, Ribeiro L, Gemperli R, Ferreira MC. Mammaplasty with inferior pedicle flap after massive weight loss. Aesthetic Plast Surg. 2010;34(5):596-602. http://dx.doi.org/10.1007/s00266-010-9516-8. PMid:20428869
3. Akyurek M. Short scar reduction mammaplasty in the bariatric patient. Ann Plast Surg. 2011;66(6):602-6. http://dx.doi.org/10.1097/SAP.0b013e3181e944b6. PMid:21372678
4. Coriddi M, Koltz PF, Gusenoff JA. Reduction mammaplasty, obesity, and massive weight loss: temporal relationships of satisfaction with breast contour. Plast Reconstr Surg. 2011;128(3):643-50. http://dx.doi.org/10.1097/PRS.0b013e318221da6b. PMid:21865997
5. Losken A, Holtz DJ. Versatility of the superomedial pedicle in managing the massive weight loss breast: the rotationadvancement technique. Plast Reconstr Surg. 2007;120(4):1060-8. http://dx.doi.org/10.1097/01.prs.0000278004.24650.e6. PMid:17805137
6. Hurwitz DJ, Agha-Mohammadi S. Postbariatric surgery breast reshaping: the spiral flap. Ann Plast Surg. 2006;56(5):481-6, discussion 486. http://dx.doi.org/10.1097/01.sap.0000208935.28789.2d. PMid:16641621
7. Song AY, Jean RD, Hurwitz DJ, Fernstrom MH, Scott JA, Rubin JP. A classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale. Plast Reconstr Surg. 2005;116(5):1535-44, discussion 1545-6. http://dx.doi.org/10.1097/01.prs.0000182606.92069.13. PMid:16217505
8. Mansur JRBBA, Bozola AR. Mastopexia e aumento das mamas com projeção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24(3):304-9.
9. Garcia EB, Fusaro R No, Arruda RF, Pereira JB, Ferreira LM. Inferior pedicle breast flap for submuscular implant coverage in mammaplasty after massive weight loss. Plast Reconstr Surg. 2010;125(2):74e-5e. http://dx.doi.org/10.1097/PRS.0b013e3181c72592. PMid:20124815
10. Resende JHCFR, Fiorelli RKA. Retrospective: mammoplasty with prosthesis after video-assisted bariatric surgery with transverse bipediculated flap. Modern Plastic Surgery. 2013;3(04):123-7. http://dx.doi.org/10.4236/mps.2013.34025.
11. Losken A. Breast reshaping following massive weight loss: principles and techniques. Plast Reconstr Surg. 2010;126(3):1075-85. http://dx.doi.org/10.1097/PRS.0b013e3181e60580. PMid:20811240
12. Ribeiro LPM, Accorsi A Jr, Buss A. Redução mamária: técnica com retalho de pedículo inferior. In: Mélega JM, Baroudi R, editores. Cirurgia plástica: fundamentos e arte: cirurgia estética. Rio de Janeiro: Medsi; 2003. p. 527-36.
13. Bonomi S, Salval A, Settembrini F, Gregorelli C, Musumarra G, Rapisarda V. Inferiorly based parenchymal flap mammaplasty: a safe, reliable, and versatile technique for breast reduction and mastopexy. Plast Reconstr Surg. 2012;130(1):116e-25e. http://dx.doi.org/10.1097/PRS.0b013e318254b552. PMid:22743895
14. Colwell AS, Driscoll D, Breuing KH. Mastopexy techniques after massive weight loss: an algorithmic approach and review of the literature. Ann Plast Surg. 2009;63(1):28-33. http://dx.doi.org/10.1097/SAP.0b013e318188b976. PMid:19546668
15. Migliori FC, Gabrielli A, Rizzo R, Serra Cervetti GG. Breast contouring in postbariatric patients: a technique selection algorithm. Obes Surg. 2010;20(5):651-6. http://dx.doi.org/10.1007/s11695-009-0058-6. PMid:20054715
16. Hönig JF, Frey HP, Hasse FM, Hasselberg J. Autoaugmentation mastopexy with an inferior-based pedicle. Aesthetic Plast Surg. 2009;33(3):302-7. http://dx.doi.org/10.1007/s00266-009-9310-7. PMid:19225831
17. Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29(3):379-91. http://dx.doi.org/10.1016/S0094-1298(02)00008-1. PMid:12365638
18. Lima EMGE Jr, Ferreira LM, Brasil AG Jr. Mamoplastia de aumento. In: Lima EML Jr, editor. Tratado de cirurgia plástica após grandes perdas ponderais. Rio de Janeiro: Atheneu; 2010. p. 87-96.
19. Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107(5):1255-72. http://dx.doi.org/10.1097/00006534-200104150-00027. PMid:11373572
20. de la Plaza R, de la Cruz L, Moreno C, Soto L. The crossed dermal flaps technique for breast reduction. Aesthetic Plast Surg. 2004;28(6):383-92. http://dx.doi.org/10.1007/s00266-004-0370-4. PMid:15633020
1. Post-doctorate, Titular Member of the Brazilian Society of Plastic Surgery (BSPS), Assistant Physician at the Plastic Surgery Service, Responsible for the Outpatient Post-bariatric Plastic Surgery at the Hospital das Clínicas of the Faculty of Medicine of Ribeirão Preto of the University of São Paulo (HCFMRPUSP), Ribeirão Preto, SP, Brazil
2. PhD, Titular Member of the Brazilian Society of Plastic Surgery (BSPS), Professor of Plastic Surgery at the Federal University of Goiás (UFG), Goiânia, GO, Brazil
Institution: Study performed at the Hospital das Clínicas of Ribeirão Preto (HCFMRP-USP), Ribeirão Preto, SP, Brazil and Master Hospital of Plastic Surgery, Goiânia, GO, Brazil.
Corresponding author:
Marina Junqueira Ferreira Rosique
Av. Antonio Diedrichsen, 400, room 1204
Ribeirão Preto, SP, Brazil ZIP 14020-250
E-mail: marina@rosique.com.br
Article received: January 17, 2014.
Article accepted: August 3, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter