

Case Report - Year 2014 - Volume 29 -
Benign lipoblastoma of the upper limb: a case report and literature review
Lipoblastoma benigno de membro superior: relato de caso e revisão da literatura
ABSTRACT
Lipoblastoma is a rare mesenchymal tumor occurring primarily in pediatric patients and formed by lipoblasts that proliferate after the postnatal period. Despite its potential for local invasion and rapid growth, its prognosis is excellent. In this study, we report the case of a pediatric patient with a ponderous lesion in the right forearm that caused considerable functional impairment of the affected limb. We also discuss the relevant aspects concerning the differential diagnosis and management of the disease, as it has the potential to cause incapacity without proper treatment.
Keywords: Lipoblastoma; Lipomatous tumors; Soft tissue tumors; Lipoblastomatosis.
RESUMO
O lipoblastoma é um tumor mesenquimal raro, composto de lipoblastos que continuam sua proliferação após o período pós-natal e que acometem, predominantemente, a população pediátrica. Apresenta prognóstico excelente, apesar do potencial de invasão local e do crescimento rápido. Os autores relatam o caso de uma paciente pediátrica portadora de volumosa lesão em antebraço direito, ocasionando importante comprometimento funcional do membro acometido. Aspectos relevantes no diagnóstico diferencial e manejo são discutidos neste trabalho, visto tratar-se de lesão com potencial risco incapacitante futuro, caso não manejada corretamente.
Palavras-chave: Lipoblastoma; Tumores Lipomatosos; Tumoração de Partes Moles; Lipoblastomatose.
Benign lipoblastoma and lipoblastomosis are, respectively, the localized or diffuse forms of the same tumor. The tumor is itself a particular variation of lipoma and lipomatosis that occur almost exclusively during infancy and early childhood1. These are rare tumors arising from embryonic fat tissue, most often occurring in the limbs and trunk, and rarely in the head, neck, or other sites2. Although benign, the lesions can grow rapidly and compromise the development of surrounding structures, with critical compression-derived symptoms3.
The term "lipoblastoma" was used for the first time by Jaffe in 1926 to describe a benign tumor of immature adipocytes4, whereas "lipoblastomosis" was first introduced by Velios et al. in 1958. Since then, approximately 200 cases have been described in the literature3. The prognosis associated with lipoblastoma is excellent and, most of the times, the tumor is neither aggressive nor metastatic. The rate of local relapse varies between 9% and 25% of the cases, with most relapses occurring with the infiltrative form. Diagnosis can pose a dilemma, as these tumors can often be mistaken for, and clinically impossible to distinguish from, lipomas and liposarcomas. The treatment of choice consists in the complete, although conservative, surgical excision of the lesion2.
CLINICAL CASE
We report the case of a pediatric patient (age, 1 year 7 months) with a congenital lesion in the right forearm. The mother reported an asymptomatic lesion that appeared shortly after birth (size, approximately 1 cm3), without any functional impairments associated. The described lesion grew slowly and progressively up to 1 year of age, but started to progress faster thereafter, affecting the flexion and extension of the forearm, wrist, and hand fingers owing to its considerable volume (Figure 1). The general pediatrician performed a clinical evaluation, and the diagnosis suggested was lymphangioma of the upper extremity, which led to the appointment with a specialized hand surgeon.

Figure 1. Patient at the age of 1 year 7 months, with a ponderous tumor in the forearm that limits all movements of the right upper limb.
The examination revealed that the lesion consisted of a mass over the whole extent of the right forearm, fixed and with a consistency resembling that of a lipoma, and apparently attached to the deep planes (Figure 2). The ultrasound, required by the general pediatrician and performed the year before, showed a cystic lesion affecting the proximal third of the forearm, with a few internal septa and widespread deep vascularization (arterial and venous); the volume of the anterior portion of the lesion was 37 × 22 × 27 mm (11 cm3). The medical evaluation performed at the first appointment led to the request for a computed tomography angiography (CTA) of the upper right limb.

Figure 2. Tumor localized along the forearm and in the proximal third of the right arm, fixed, with the consistency of a lipoma and apparently attached to the deep planes, which occasionally leads to compression with relevant functional consequences.
The CTA examination, performed 1 year after the ultrasound, showed a fusiform thickening the soft tissues along the right upper limb, mostly affecting the two proximal ends of the forearm, with increased diameter of that portion of the arm (Figure 3). There was a significant increase in volume when compared with the previous examination: the size was now approximately 14.5 × 9.0 cm in the longitudinal and transversal axes, respectively. This significant increase in tumor volume was due to the increase in number and size of the cystic cavities and of loculi with internal septations. The CTA showed a ponderous lesion with venolymphatic malformations (lymphangioma) that extended form the distal third of the arm (above the elbow) to the right wrist; the radial, median, and ulnar arteries remained pulsatile and permeable (Figure 4). The bone structure of the right upper limb was preserved.

Figure 3. Computed tomography angiography (CTA). Fusiform thickening of the soft tissues along the right upper limb, mostly affecting the two proximal ends of the forearm, with increased diameter of that portion of the arm.
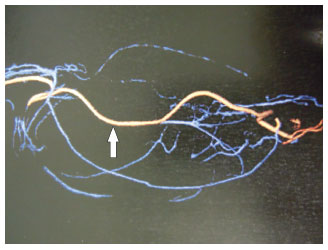
Figure 4. Computed tomography angiography (CTA) with image reconstruction, showing alterations in the normal vessels of the forearm due to compression by the tumor. The arrow points the radial artery, which remained pulsatile and permeable despite the proximity with the tumor.
On the basis of the CTA observations and on the clinical characteristics of the lesion, we decided to perform an embolization with the purpose of decreasing the size of the lesion and facilitate its resection; however, the procedure was not successful.
The patient was then submitted to the complete resection of the lesion. The appearance of the tumor was encapsulated, lipoid, and firm; the tumor contained septa and infiltrated the anterior, lateral, and posterior muscles of the right forearm, thus leading to occasional compression of the nerves and vases. The tumor was completely resected, and all muscles were preserved, as well as the major structures of the affected area (Figure 5).

Figure 5. Surgery for resection of the lesion resembling a lipoma, encapsulated and of considerable size. The lesion was approached through the anterior part of the forearm and was carefully detached form the critical structures in the affected area.
According to the anatomopathological examination, the lesion had a weight of 600 g, was yellow, of mixed appearance, and measured 12 × 10 × 6.5 cm, which led to the final diagnosis of a benign lipoblastoma.
The postoperative recovery progressed well, and none of the vessels of the arm was affected. After 4 months of follow-up, the patient was able to move the forearm, wrist, and fingers again. The only functional consequence was a partial impairment in the movement of the thumb, which was reverted with physiotherapy (Figures 6 and 7).

Figure 6. Four months after surgery. Important decrease in the volume of the forearm was observed after the previously described approach and resection of the tumor.

Figure 7. Four months after surgery. The movements of the hand were recovered after tumor resection. No functional consequences were detected.
DISCUSSION
Lipoblastoma is a rare benign mesenchymal tumor that grows rapidly, usually occurring within the first 3 years of life, but also occasionally from birth. Published data show that between 80% and 90% of the cases occur before 3 years of age and 40% before the first year2. Particular cases have been reported in older children1. Although rare, there are reported cases in adults. Carcassonne et al. have described a case of lipoblastoma of the mesenterium in a 63-year-old man. Stout and Lattes found six cases of lipoblastomas in adults2. There are no congenital malfunctions or syndromes associated with the tumor, and several studies have described a higher prevalence in males. Often, in the upper and lower limbs, the tumor is described as a painless mass, with 46% to 70% of all cases found in those regions of the body. Less frequent locations include the head and neck, trunk, mediastinum, mesenterium, and retroperitoneum1.
Two types of lipoblastomas have been described: localized (lipoblastoma benigno) and diffuse or infiltrative (lipoblastomatose benigna). The localized form, which is more common, develops in superficial soft tissues, clinically resembling a lipoma. The diffuse form has a tendency not only for subcutaneous infiltration but also for infiltrating the adjacent muscle tissue, with a higher propensity for local relapse (approximately 9-22%, according to the literature2,3). Most patients develop a tumor in soft tissues with slow and progressive growth; however, there are reports of tumors that undergo rapid growth periods, such as the case of the present patient. Depending on the location and size of the tumor, there can be a compression of adjacent structures, with functional consequences. Lesions in the cervical vertebrae, for example, can obstruct the airways and cause respiratory insufficiency. Typically, imaging examinations show a well-circumscribed tumor of the soft tissues, with a density similar to that of adipose tissue. Although useful for the preoperative evaluation, to determine disease extension, and to plan the resection, those radiological examinations have limitations in discriminating between the various tumors2. Diagnosis is important, as the treatment of these tumors is different from the management of lipomas and liposarcomas2. Ultrasound can be useful to detect the presence, or absence, of fluids, and Doppler ultrasound to determine the irrigation of the tumor. Computed tomography examinations usually show low Hounsfield density, which suggests the presence of adipose tissue. In magnetic resonance imaging (MRI), low-density T1 images can be associated with lipoblastomas, compared with lipomatosis, owing to increased cell content, which allows the distinction between lipoblastoma and subcutaneous tissue or lipoma. Currently, there are no pathognomonic imaging findings that can be associated with lipoblastoma, and hence MRI alone is not enough to establish the diagnosis. Radiological monitoring is thus particularly useful during the follow-up and for detecting tumor relapse3,4.
Owing to the limitations associated with radiological examinations, an accurate diagnosis in the preoperative period is rarely achieved. Lipoblastoma is usually mistaken for a lipoma or hemangioma3,4. Occasionally, diagnosis can be obtained from fine-needle aspiration biopsy, as previously reported2,5,6.
Macroscopically, the tumors are lobulated and soft. The final diagnosis is established on the basis of the histopathological results. The tumors are made of lipoblasts that continue to proliferate after birth, in addition to a mixed matrix and fibrous trabeculae (Figure 8). Lipoblasts are usually made of multiple fat vacuoles, although often there are cells with single vacuoles (signet ring cell)7. The cytological examination does not show anaplasia or pleomorphisms. Recently, cytogenetic abnormalities were identified in cases of lipomatosis. A clonal rearrangement in the chromosomal region 8q11-13 was identified in a lipoblastoma, whereas the t(12;16) translocation can be observed in mixed-type liposarcomas8. Because the clinical findings of the lipoblastoma can mimic those of the liposarcoma, these findings are relevant for the final diagnosis2, especially for difficult cases or those with borderline pathology results4.
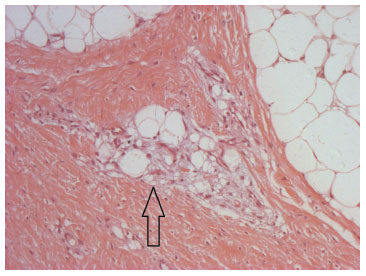
Figure 8. Optical microscopy image (magnification 100×; hematoxylin and eosin stain), showing the lipoblast clusters (immature adipocytes, arrow). In the upper left and right corners, mature adipocytes can be seen.
Because of the progressive and slow growth of these tumors, as well as considering their local invasion, the treatment of choice is total surgical excision, with conservative measures to avoid compromising the structures functionally7,8. In cases of total resection, the reported relapse rate varies from 14% to 25%.
CONCLUSION
Lipoblastoma is a rare and benign mesenchymal tumor with rapid growth that occurs primarily in pediatric patients; however, a few cases have also been reported in adults9. The extremities are more often affected, and the tumors can reach considerable sizes. Preoperative imaging techniques are used for disease evaluation and to guide the excision. MRI is, possibly, the most adequate technique for this purpose10. Currently, there are no pathognomonic findings for this lesion; thus, the presurgical diagnosis is often difficult. It is important to distinguish this lesion from other lipomatosis (lipoma, liposarcoma), as the management and the prognosis are frequently distinct11.
REFERENCES
1. Weiss SW, Goldbllum JR. Enziger and Weiss's soft tissue tumors. 4th ed. St. Louis: Mosby; 2001.
2. Kok KYY, Telisinghe PU. Lipoblastoma: clinical features, treatment, and outcome. World J Surg. 2010;34(7):1517-22. http://dx.doi.org/10.1007/s00268-010-0466-8. PMid:20151124
3. McVay MR, Keller JE, Wagner CW, Jackson RJ, Smith SD. Surgical management of lipoblastoma. J Pediatr Surg. 2006;41(6):1067-71. http://dx.doi.org/10.1016/j.jpedsurg.2006.02.025. PMid:16769336
4. Speer AL, Schofield DE, Wang KS, Shin CE, Stein JE, Shaul DB, et al. Contemporary management of lipoblastoma. J Pediatr Surg. 2008;43(7):1295-300. http://dx.doi.org/10.1016/j.jpedsurg.2007.10.068. PMid:18639685
5. Kloboves-Prevodnik VV, Us-Krasovec M, Gale N, Lamovec J. Cytological features of lipoblastoma: a report of three cases. Diagn Cytopathol. 2005;33(3):195-200. http://dx.doi.org/10.1002/dc.20322. PMid:16078242
6. López-Ferrer P, Jiménez-Heffernan JA, Yébenes L, Vicandi B, Viguer JM. Fine-needle aspiration cytology of lipoblastoma: a report of two cases. Diagn Cytopathol. 2005;32(1):32-4. http://dx.doi.org/10.1002/dc.20073. PMid:15584040
7. Dilley AV, Patel DL, Hicks MJ, Brandt ML. Lipoblastoma: pathophysiology and surgical management. J Pediatr Surg. 2001;36(1):229-31. http://dx.doi.org/10.1053/jpsu.2001.20060. PMid:11150471
8. Mognato G, Cecchetto G, Carli M, Talenti E, D'Amore ESG, Pederzini F, et al. Is surgical treatment of lipoblastoma always necessary? J Pediatr Surg. 2000;35(10):1511-3. http://dx.doi.org/10.1053/jpsu.2000.16428. PMid:11051165
9. Estrella EP, Lee EY. Lipoblastoma of the hand treated with excision and ligament reconstruction: a case report. Hand Surg. 2008;13(2):103-6. http://dx.doi.org/10.1142/S0218810408003840. PMid:19054842
10. Chen CW, Chang WC, Lee HS, Ko KH, Chang CC, Huang GS. MRI features of lipoblastoma: differentiating from other palpable lipomatous tumor in pediatric patients. Clin Imaging. 2010;34(6):453-7. http://dx.doi.org/10.1016/j.clinimag.2009.11.009. PMid:21092875
11. Morerio C, Nozza P, Tassano E, Rosanda C, Granata C, Conte M, et al. Differential diagnosis of lipoma-like lipoblastoma. Pediatr Blood Cancer. 2009;52(1):132-4. http://dx.doi.org/10.1002/pbc.21747. PMid:18798558
1. Plastic Surgeon by the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Specialist Member of the Brazilian Society of Plastic Surgery (SBCP), Member of the Clinical Staff of the Circulo Operário Caxiense Hospital (COC), Pompéia Hospital and Healh Hospital, Plastic Surgeon at the Pro-Face Program of the COC Hospital, Caxias do Sul, RS, Brazil
2. Plastic Surgeon by the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Specialist Member of the Brazilian Society of Plastic Surgery (SBCP), PhD Student of Medicine and Health Sciences at the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Plastic Surgeon at the MOB Clinic, Porto Alegre, RS, Brazil
3. Plastic Surgeon by the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Specialist Member of the Brazilian Society of Plastic Surgery (SBCP), Caxias do Sul, RS, Brazil
4. Full Professor at the Federal University of São Paulo (UNIFESP), Lecturer in the Department of Surgery of the Faculty of Medicine (FAMED) of the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Chief of Service at the Hand and Reconstructive Microsurgery Service at the São Lucas Hospital of the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Former President of the Brazilian Society for Hand Surgery (SBCM), Director of the Faculty of Medicine (FAMED) of the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Caxias do Sul, RS, Brazil
Institution: Work performed at the Hand and Reconstructive Microsurgery Service at the São Lucas Hospital of the PUCRS, Porto Alegre, RS, Brazil.
Corresponding author:
Jefferson Braga Silva
Pontifícia Universidade Católica do Rio Grande do Sul, Faculty of Medicine, Department of Surgery
Av. Ipiranga, 6690, conj:216, Centro Clínico PUCRS - Jardim Botânico
Porto Alegre, RS, Brazil CEP 90610-000
Phone: +55 (51) 3315-6277
E-mail: jeffmao@terra.com.br
Article received: July 8, 2011.
Article accepted: July 29, 2011.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter