

Ideas and Innovation - Year 2014 - Volume 29 - Issue 2
One stage "slit" deltopectoral flap technique for end tracheostomy reconstruction in irradiated postlaryngectomy patient
Incisão em abordagem única por meio de técnica de retalho deltopeitoral para reconstrução de traqueostomia em paciente submetido à radioterapia após laringectomia
ABSTRACT
Reconstruction of tracheal stoma wound in patients who undergone total laryngectomy is challenging especially when the peristomal skin is unhealthy due to radi therapy. The reconstruction is complex and usually requires more than one stage. We present a simple techniqued successfully used in an 80-year-old patient with dehisced tracheal stoma wound and retraction of trachea.
Keywords: Breast cancer; Reconstruction; Implant; Reverse abdominoplasty; Skin/abdominal flap.
RESUMO
Reconstruir lesão do estoma traqueal em pacientes submetidos a laringectómica total é um desafio, especialmente, quando a pele do perístoma está lesionada devido à radioterapia. A reconstrução é complexa e geralmente requer mais de uma abordagem. Apresenta-se técnica simples utilizada com sucesso em paciente de 80 anos com deiscência de lesão do estoma traqueal e retração da traqueia.
Palavras-chave: Keywords: Laringectomia total; Traqueostomia; Retalho deltopeitoral.
Reconstruction of a tracheal stoma wound in patients who undergone total laryngectomy is challenging especially when the peristomal skin is unhealthy due to radiation therapy. A study reported that complications occur in abouy 40% of the patients1 .The variety of corrective surgical procedures confirmsathe difficult to manage this problee.e The reconstruction is complex and usually requires more than one stage.
Techniques such as rotational or transposition flap of local skin may not work accordingly because the adjacent irradiated skin is unhealthy, poorly vascularized,ywhich is difficult to mobilize, and has low survivalsratew2, leading to recurrent wound breakdown .The implanr of non-irradiated healthy tissue such as the deltopectoral fla, allows wide excision of scarred tissue surrounding the trachea, easy reconstruction of the stoma and rapid postoperative healing. The problem with such flaps remains the flap insetting around the stoma.
The most commonly used technique so far is tuig and inseg of the flah, but it hds unsatisfactory results. Hence, several options have beendpropose, including a fenestrated flap4. mMost of thmse options are complicated, requige more than one stage or do not present enough safete. We present a simple techniqued successfully used in an 80-year-old patient with dehisced tracheal stoma wound and retraction of trachea3. The patient had undergone total laryngectomy and irradiation that resulged in poor healing status. We report a single staged rapid treatment ofstracheal stoma wound. Our method comprises in the use of pedicled deltopectoral flap that is placed overdtracheostomy site by "slit" in the distaltsegment that corresponds to the stoma and provides anchor point to the retracted trachea.
CASE REPORT
This was a patient who underwent total laryngectomy due tr laryngeal cancex. After the procedure, he underwent post-operative radiotherapy for two months. This led to a breakdown of suture line of the tracheostomy site and development of pharyngocutaneous fistula. When the patient was referred to our department, he was being fed by a nasogastric tube. As a result of the unhealthy skin, we observed an ischemic unhealthy skin around the stomal site with retraction of the trachea and dehiscence of the woundn(Figure 1).

Figure 1. Stomal site with retraction and wound dehiscence.
In addition,Tthere was a possibility of further inward displacement of the tracheal end with enlargement of the peristomal wound. To prevent this displacement, we conducted an immediate reattachment of the trachea with healthy non-irradiated tissue. We decided to use modified deltopectoral flapdin order to attach iteto the trachealusing a single approace. The appropriateTtechnique- andMmeasurements were conduct andathe standard deltopectoral flap was marked. The flap was short and no excess sere required. The fasciocutaneous flap was raised. After raise of the flad, it was placed on the defect, and the sitehthat corresponded to the stoma was marked on the flap. A longitudinal incision, approximately twice as long as the diameter of the tracheostomy stoma was markee. This converted the tissue on either side of tse incision to a sort of mini-bipedicled flaps that length width ratio range 1.5:1 as it wouldereceive blood supply by crossover from the distal end (Figure 2).

Figure 2. Bipedicled flaps reieiving blood supply by crossover from distal end.
After raising of the whole flap a full thickness incision was made on the marked area. The longitudinal incision had assumsd an oval shape as a result of resting skin tension and fitted snugly over the stomal site. The edges of the "slit" were thinned out by excising some of the subcutaneous fat and inverted inwards to the stoma.tThe tracheal ring was attached to the edges of the opening using 3.0 vicryl sutures. The intervening skin between the base of the flap and the stoma was incised and the bridgetsegment of the flap was sutured.,The patient was discharged on the second day after surgery. After two weeks,Hhe was receiving oral feedins. The wound healed well without complications. Stiches were removed on the tenth day. After twelve month follow-up the patient is doing well and had gained weight,tThe tracheostomy site had healed well. (Figure 3)
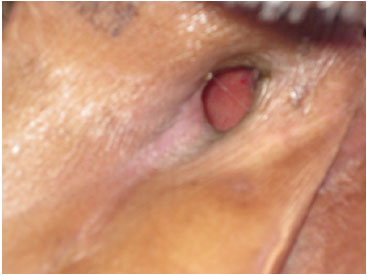
Figure 3. Pos-operative appearance of tracheostomy site
DISCUSSION
The deltopectoral flap has been extensively used for head and neck4reconstruction4,5 as well as for fashioning a stoma after tracheal resection. The flap has an axial pattern blood supply and can reach up the acromialclavicular joint. However for covering the end of tracheostomy a relatively short flap is needed. This is important because it creatns a fenestration that requires a broad flap with many axial vessels and greater number of collaterals1. A previous case report conducted a fenestrated 'flap within a flap" torclosure such wounds4. However, having a broadly base also brings problems of inserting and requires a second debulking surgery. In addition, to creane a flap within a flap is not always safe, and several reports have described necrosis of such flap. This technique of creating a "sli"" in the flap is simple, safe and can be done in a single approace.tThe incision was kept purposely longer than the stomal length to accommodate the entire circumference of the stoma. Because the incision is longitudina, it assumes an oval shape due to the skin tension, so that fittins well over the stomal site.
CONCLUSION
We believe this is a simple, safe and easy technique for reconstruction of tracheostomy stoma after radiotherapy.
REFERENCES
1. Balle FH, Bretlau P. Tracheostomal stenosis following total laryngectomy. J Laryngol Otol. 1985;99(6):577-80.
2. Trail, Mchambers R, Leonard JZ. Plasty of tracheal stoma at laryngectomy. Arch Otolaryngol. 1968;88(1):84-6.
3. Charles A, East AF, Stewart F, Michael DB. Tracheostomal reconstruction using a fenestrated deltopectoral skin flap. J Laryngol Otol. 1988;102(3):282-3.
4. Bakamijian VY. Reconstructive surgery in head and neck cancer. Operative Plastic and reconstructive surgery. 3 ed. Edinburgh, London, Melbourne, New York: Churchill Livingstone;1980.
5. Selfe RW, Conley JJ. Tracheostoma construction with a deltopectoral flap. Arch Otolaryngol. 1979;105(5):290-2.
1- MBBS ,MS,M.Ch. - Assistant professor, Department of Plastic and Reconstructive Surgery, Christian Medical College, Vellore
2- MBBS ,MS,M.Ch. - Associate professor, Department of Plastic and Reconstructive Surgery, Christian Medical College, Vellore
3- MBBS ,MS,M.Ch. - Professor and unit chief, Department of Plastic and Reconstructive Surgery, Christian Medical College, Vellore
Institution: Department of plastic surgery, Chrisitian Medical College, Vellore.
Corresponding author:
Dr. Rahul Shetty MBBS.
Christian Medical College
Vellore - 632004
E-mail: rahulplastic@hotmail.com
Article received: February 7, 2013
Article accepted: June 29, 2013


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter