

Original Article - Year 2014 - Volume 29 -
Quantitative evaluation of drain flow in lipoabdominoplasty - a comparative study
Avaliação quantitativa do débito do dreno na lipoabdominoplastia - estudo comparativo
ABSTRACT
INTRODUCTION: The importance of Scarpa's fascia in reducing both skin suture tension and seroma is a subject of great discussion in lipoabdominoplasty. This study evaluates drain flow in lipoabdominoplasty, with and without preservation of Scarpa's fascia, on postoperative days 1º, 3º, 5º, and 7º.
METHODS: This was a prospective, randomized, and serial study of 24 patients who underwent lipoabdominoplasty; procedures performed by seven different surgeons (residents) were evaluated between August and December 2013. The patients were divided into two groups according to whether Scarpa's fascia was preserved or removed. Drain flow was evaluated on postoperative days 1º, 3º, 5º, and 7º, and complications were assessed in the two groups.
RESULTS: Three patients developed epitheliosis on the umbilical scar, and two were smokers. There was less fluid drainage in Group 1 patients compared to Group 2, and this was less significant on postoperative day 1. One patient in Group 2 developed a seroma (40 ml), which was aspirated with a syringe on postoperative day 10, with no recurrence.
CONCLUSION: Lipoabdominoplasty with Scarpa's fascia preservation resulted in reduced serosanguinous drainage, both when taken as a whole (182.09 ml less for the seven day total), or measured daily.
Keywords: Lipoabdominoplasty; Abdominoplasty; Liposuction; Seroma.
RESUMO
INTRODUÇÃO: A importância da fáscia de Scarpa, tanto na diminuição da tensão da sutura da pele quando na diminuição do seroma, são assuntos de grande discussão sobre a lipoabdominoplastia. Este estudo tem o objetivo de avaliar o débito nos drenos, nos 1º, 3º, 5º e 7º dias de pós-operatórios, em procedimentos de lipoabdominoplastias com e sem preservação da fáscia de Scarpa.
MÉTODOS: Estudo prospectivo, randomizado e consecutivo, analizando 24 pacientes submetidas à lipo abdominoplastia por sete cirurgiões (residentes) diferentes, no período de agosto-dezembro de 2013. As pacientes foram divididos em 2 grupos, um com manutenção da fáscia de Scarpa e outro onde ela foi removida. Foi pesquisado o débito no dreno nos 1º, 3º, 5º e 7º dias de PO, assim como as complicações nos dois grupos.
RESULTADO: Três pacientes do grupo apresentaram epiteliólise na cicatriz umbilical, sendo duas delas tabagistas. Houve menor quantidade de líquido drenado no grupo 1 do que no grupo 2, sendo significância menor no 1º pós-operatório. Um paciente do grupo 2 apresentou seroma (40ml), aspirado com seringa no 10º PO, sem recidiva.
CONCLUSÃO: Ficou demonstrado que a lipoabdominoplastia com preservação da fáscia de Scarpa apresentou diminuição de drenagem sero-sanguinolenta, tanto nas medições como um todo (182,09ml a menos na somatória dos sete dias) quanto na medição de cada dia isoladamente.
Palavras-chave: Lipoabdominoplastia; Abdominoplastia; Lipoaspiração; Seroma.
Body shape may present with esthetic and functional deformities, mostly affecting the abdomen. These deformities are due to genetic and acquired causes, such as obesity, weight loss, and pregnancy, among others. In addition, these present with varying degrees of skin sagging, localized fat accumulation, and diastasis of the rectus abdominis muscles, which may result in loss of self-esteem1.
The history of abdominoplasty documents progressive flap detachment, which attained maximal extent in 1957, with the goal of transplantation of the umbilicus, otherwise resected by most techniques2. This led to great advances in use of flaps for abdominal plastic surgery, which also standardized the low and definitive suprapubic scar location in the 1960s3,4.
Liposuction accelerated the development of abdominal plastic surgery, and encouraged many surgeons to develop different procedures and technical details to improve esthetic results, especially in the abdomen5.
In 1996, Lockwood6 described the importance of Scarpa's fascia in abdominal plastic surgery, suggesting it could decrease suprapubic skin suture tension.
Costa-Ferreira et al7, Di Marino et al8, and Louam9 drew attention to the importance of Scarpa's fascia in reducing seroma.
Developed in 2000 by Saldanha10,11,12, and published for the first time in 2001, lipoabdominoplasty is a safe option for correction of abdominal esthetic and functional deformities, by standardizing the selective detachment of the internal borders of the rectus abdominis muscles. By combining two traditional techniques, liposuction and abdominoplasty, the conservative concept of this procedure is based on the preservation of perforating vessels (subcutaneous pedicle), i.e. branches of the deep epigastric vessels, and Scarpa's fascia.
Other authors perform lipoabdominoplasty without preservation of Scarpa's fascia, but use adhesive sutures13,14,5.
OBJECTIVE
This study measured drain flow in lipoabdominoplasty, with and without preservation of Scarpa's fascia, on postoperative days 1, 3, 5, and 7.
METHOD
This is a prospective, randomized, and serial study of 24 patients who underwent lipoabdominoplasty; procedures performed by seven different surgeons (residents) at Santos Day Hospital were analyzed between August and December 2013. The patients underwent preanesthesia evaluation, and were classified according to the American Society of Anesthesiologists (ASA) system. The patients also underwent abdominal ultrasound, to avoid surgery in asymptomatic individuals with abdominal hernias.
The patients were divided into two groups of 12 individuals each:
Group 1(G1), with preservation of Scarpa's fascia in the infraumbilical abdomen; Group 2 (G2), without preservation of Scarpa's fascia in the same region, removed en bloc with dermal adipose tissue.
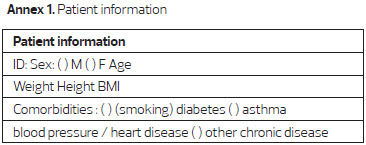
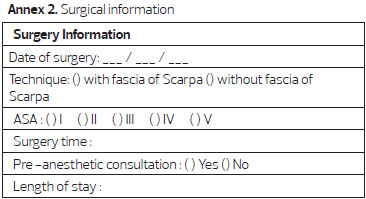
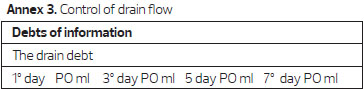
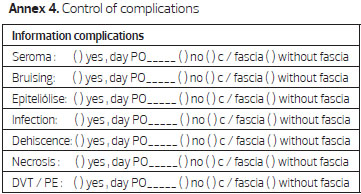
According to the protocol, we evaluated the patient's medical history, surgical information, and drain flow on postoperative days 1, 3, 5, and 7, and assessed possible complications (Appendices 1-4).
Randomization of the patients was based on the chronological order in which they underwent lipoabdominoplasty by a resident at Santos Day Hospital. In odd-numbered patients, Scarpa's fascia was preserved, and in even-numbered patients, it was not preserved.
The inclusion criteria for the study were as follows: female gender, age 26-58 (average, 42) years, BMI less than 30, good general health, ASA score 1 or 2, and complaints of sagging, lipodystrophy, or diastasis of the rectus abdominis.
The exclusion criteria were as follows: male gender, BMI greater than 30, abdominal hernia, eventration, abdominal malformation, and postoperative bariatric surgery.
Smokers were not excluded. All patients gave written informed consent.
The procedure was lipoabdominoplasty with preservation of Scarpa's fascia in the lower abdomen in Group 1, and without preservation in Group 2.
In both groups, 2000 ml of 0.9% saline solution containing epinephrine 1:1000 was infiltrated in the superficial and deep fat planes.
All patients were hospitalized for 24 hours, ambulated early (at night), and remained in the hospital until discharge.
Drain flow was evaluated in all patients by the same observer (the author) on postoperative days 1, 3, 5, and 7.
Alternate and remaining sutures were removed on postoperative days 8 and 12, respectively. The patients were monitored for 30 days for the appearance of seroma.
RESULTS
Group 1 (Scarpa's fascia preserved)
Group 1 included three smokers, none was menopausal, four used contraceptives, one was on hormone replacement, two had hypertension, and one had hypothyroidism (Figure 1).
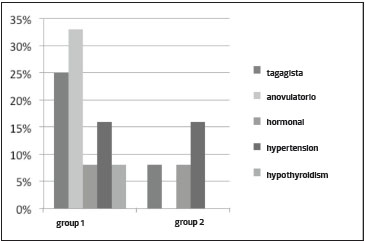
Figure 1. Patient information.
Surgical information: nine patients were ASA score 1 and three were ASA score 2; in six patients, surgery lasted up to 4 hours, and in the other six, between 4 and 5 hours, with an average of 4.34 hours; all patients underwent preanesthesia evaluation, and remained in the hospital for 24 hours.
Three patients developed epitheliosis on the umbilical scar, and two of these were smokers. No other complications were observed, such as necrosis, wound dehiscence, or deep vein thrombosis/pulmonary embolism (DVT/PE).
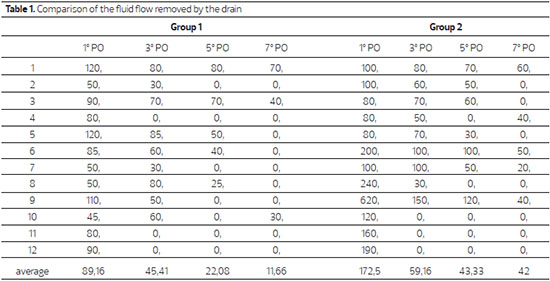
Drain flow in group 1 (Figure 2):
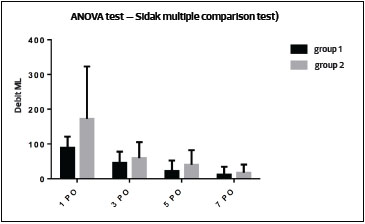
Figure 2. The graph illustrates drain flow in the two groups on postoperative (PO) days 1, 3, 5, and 7 (analysis of variance.
PO day 1 - varied between 45 and 150ml, with an average of 89.16ml
PO day 3 - varied between 30 and 85ml, with an average of 45.41ml
PO day 5 - varied between 25 and 80ml, with an average of 22.08ml
PO day 7 - varied between 30 and 70ml, with an average of 11.66ml
In three patients, drainage could be performed on postoperative day 3, and in seven patients, on day 5; only three patients had fluid accumulation on day 7.
Group 2 (without Scarpa's fascia)
Group 2 included one current smoker and two ex-smokers, two were menopausal, none used contraceptives one was on hormone replacement therapy, and two had hypertension (Figure 5).
Surgical information: nine patients were ASA score 1 and three were ASA score 2; in five patients, surgery lasted up to 4 hours, and in other seven, between 4 and 5 hours, with an average of 4.30 hours, all patients underwent preanesthesia evaluation, and remained in the hospital for 24 hours.
Epitheliosis was observed in one patient, a smoker. No other complication was detected, such as necrosis, wound dehiscence, or DVT/PE.
Drain flow in group 2: (Figure 2):
PO day 1 - varied between 80 and 620ml, with an average of 172.5ml
PO day 3 - varied between 30 and 150ml, with an average of 59.16ml
PO day 5 - varied between 30 and 120ml, with an average of 43.33ml
PO day 7 - varied between 20 and 60ml, with an average of 42ml
During this period, both groups showed a reduction in drain flow. When compared by day using ANOVA and the Sidak multiple comparison test, the amount of fluid drained in group 1 was less than in group 2, and significantly less on postoperative day 1 (Table 1).
The drainage was performed on postoperative day 7 in all patients.
One patient in group 2 developed a seroma (40ml), which was aspirated with a syringe on postoperative day 10, without recurrence. None of the patients required readmission.
DISCUSSION
The possible complications of abdominal plastic surgery remain much debated in the specialized literature16.
The development of seromas was highlighted in the late 1990s, with publications noting the importance of preserving Scarpa's fascia in preventing this complication. Although still controversial, authors increasingly report this finding6,7,8,9.
Several advantages are noted regarding postoperative and long-term outcomes: low morbidity due to the preservation of perforating vessels, absence of dead space under the flap, low rate of complications, and preserved suprapubic sensation17.
Many studies on lipoabdominoplasty confirmed a decreased incidence of seroma with the preservation of Scarpa's fascia, in addition to aspects related to less intraoperative bleeding12,13,14. The deep membranous layer of the subcutaneous abdominal tissue contains several yellow elastic fibers. The areolar tissue is weakly linked to the aponeurosis of the external oblique, although the medial aspect is closely adherent to the linea alba and symphysis pubis. This connective tissue plays a role in providing support and mobility to nerves, blood, and lymphatic vessels crossing through it. Removal of this anatomical structure may thus damage these components. The preservation of inferior perforating vessels, and lymphatic vessels, in particular, may facilitate greater fluid drainage in the immediate postoperative period, thus ensuring greater adhesion between flap and deep planes.
The most common complications observed in abdominoplasty and described in the literature are seroma, epitheliosis, dehiscence, necrosis, and hematoma16,17. In lipoabdominoplasty a significant decrease in the incidence of seromas and epitheliosis was observed, in addition to fewer dehiscences, necroses, and hematomas18. These were attributed to minor trauma, and to vascular, lymphatic, and nerve preservation19.
The documentation regarding a decreased number of complications, mainly seroma formation, is related to the preservation of the lymphatic vessels and nerves, which contributes to a reduction in the surgical drainage9.
In this study, we noted decreased fluid flow in patients with preserved Scarpa's fascia at all four measurement times. Group 1 had an average of 83.34ml, 47.16ml, 21.25ml and 30.34ml less drainage than group 2, on postoperative days 1, 3, 5, and 7, respectively (the average difference in drainage for the four measures taken was 182.09ml and was most significant on postoperative day 1). This result is in agreement with literature reporting that decreased seroma incidence is related to the preservation of the fascia. Moreover, the number of patients in whom early drainage was performed was greater in Group 1 (with Scarpa's fascia preserved). Although not significant, the only seroma observed was in Group 2 (without Scarpa's fascia preserved).
In both groups, there were no significant differences in comorbidities or surgical history and data
Further studies are needed, with particular attention to the relationship of serosanguinous drainage in the first seven postoperative days with the possible development of seromas.
CONCLUSION
Average drain flow in lipoabdominoplasty-as the total of four measurements or as separate daily totals-was lower in the group of patients in whom Scarpa's fascia was preserved and was most significant on postoperative day 1.
REFERENCES
1. Castro CC, Salema R, Atias P, et al. T abdominoplasty to remove multiple scars from the abdomen. Ann Plast Surg. 1984;12:369.
2. Vernon S. Umbilical transplantation upward and abdominal contouring in lipectomy. Am J Surg. 1957;94:490-2.
3. Callia WEP. Dermolipectomia abdominal. São Paulo (Brazil): Carlo Erb; 1963.
4. Pitanguy I. Abdominoplasty: classification and surgical techniques. Rev Bras Cir. 1995;85:23-44.5.
5. Illouz YG. A new safe and aesthetic approach to suction abdominoplasty. Aesthetic Plast Surg. 1992;16:237-45.
6. Lockwood T. Fegli-lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;9:603-8.
7. Costa-Ferreira A, Rebelo M, Vásconez LO, Amarante JA. Scarpa fascia preservation during abdominoplasty: A prospective study. Plast Reconstr Surg. 2010;125:1232-9.
8. Di Martino M, Nahas FX, Barbosa MV, et al. Seroma in LAP and abdominoplasty: A comparative study using ultrasound. Plast Reconstr Surg. 2010;126:1742-51.
9. Le Louarn C. Partial subfascial abdominoplasty. Aesth Plast Surg. 1996;20:123-7.
10. Saldanha OR, Souza Pinto EB, Matos WN Jr, et al. Lipoabdominoplasty without undermining. Aesthet Surg J. 2001;21:518-26.
11. Saldanha OR. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;22(4):322-7.
12. Saldanha OR, Salles AG, Ferreira MC, Llaverias F, Morelli LH, Saldanha Filho OR, et al. Aesthetic evaluation of lipoabdominoplasty in overweight patients. Plast Reconst Surg. 2013;132(5):1103-12.
13. Graf R, de Araújo LRR, Rippel R, Graça Neto L, Pace DR, Cruz GA. Lipoabdominoplasty: Liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;30:1.
14. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1988;18:439.
15. Pollock H, Pollock T. Progressive tension sutures: A technique to reduce local complications in abdominoplasty. Plast Reconst Surg. 2000;105(7):2583-6.
16. Stewart KJ, Stewart DA, Coghlan B, Harrison DH, Jones BM, Waterhouse N. Complications of 278 consecutive abdominoplasties. J Plast Reconstr Aesthet Surg. 2006;59:1152-55.
17. Dillerud E. Abdominoplasty combined with suction lipoplasty: A study of complications, revisions, and risk factors in 487 cases. Ann Plast Surg. 1990;25:333-38; discussion 339.
18. Heller JB, Teng E, Knoll BI, Persing J. Outcome analysis of combined lipoabdominoplasty versus conventional abdominoplasty. Plast Reconstr Surg. 2008;121:1821-9.
19. Fels KW, Cunha MS, Sturtz GP, Gemperli R, Ferreira MC. Evaluation of cutaneous abdominal wall sensibility after abdominoplasty. Aesthetic Plast Surg. 2005;29:78-82.
1 - Specialist in Plastic Surgery, Brazilian Society of Plastic Surgery (BSPS)
2 - PhD - President of BSPS 2006-7, Director of DESC, Regent of the Plastic Surgery Service of the Unisanta Division of Plastic Surgery of Unimes
3 - MD - Resident on the Plastic Surgery Service of Unisanta
4 - MD - General Surgery Resident at Santa Casa de Santos
5 - MD - Teaching Preceptor of the Plastic Surgery Service of Unisanta
6 - MD - Resident on the Plastic Surgery Service of Unisanta
Institution: Plastic Surgery Service of Unisanta.
Corresponding author:
Osvaldo Saldanha Filho
Av. Wasghington Luiz, 142
Santos, São Paulo, Brazil. ZIP: 11.050-200
E-mail: osvaldinhosaldanha@hotmail.com
Article Submitted: December 11, 2013
Article Accepted: March 4, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter