

Original Article - Year 2014 - Volume 29 -
Oncologic evaluation after breast reconstruction with fat grafting
Avaliação oncológica após reconstrução mamária com lipoenxertia
ABSTRACT
INTRODUCTION: Breast reconstruction is an essential step in the treatment of patients with breast cancer. Fat grafting is an important resource for improved esthetic results. Recently, however, some authors have questioned the safety of fat grafting, suggesting that this technique can increase the risk of local tumor recurrence.
METHODS: A retrospective, cross-sectional cohort study was conducted through a review of medical records of patients who underwent breast reconstruction with fat grafting by the Plastic Surgery Division of the Clinical Hospital of the Ribeirão Preto Faculty of Medicine of the University of São Paulo (FMRP-USP), from 2006 to 2010.
RESULTS: We selected 18 patients, of whom eight (44%) had ductal carcinoma by histology. Three patients (17%) underwent neoadjuvant chemotherapy, and of these, two (11%) were also subjected to adjuvant chemotherapy. Nine (50%) received only adjuvant chemotherapy. Eleven patients (61%) underwent adjuvant radiotherapy, and thirteen (72%) had hormonal therapy. For breast reconstruction, eight patients (44.4%) underwent a transverse rectus abdominis myocutaneous (TRAM) flap procedure, six (33.3%) had an expander and prostheses, and four (22.2%) underwent a procedure with the latissimus dorsi muscle flap and prostheses. The number of fat grafting sessions ranged from one to four. No cases of locoregional recurrence of breast cancer were identified.
CONCLUSION: There has been no evidence of locoregional recurrence to date, demonstrating that fat grafting is a reliable and safe procedure for improving the results of breast reconstruction after cancer treatment.
Keywords: Breast reconstruction; Breast cancer; Fat grafting; Tumor recurrence.
RESUMO
INTRODUÇÃO: A reconstrução mamária é etapa fundamental no tratamento de pacientes com câncer de mama, sendo a lipoenxertia um importante recurso para melhora no resultado estético. Todavia, recentemente, alguns autores têm questionado a segurança da lipoenxertia, sugerindo que essa técnica possa aumentar o risco de recidiva tumoral local.
MÉTODOS: Estudo retrospectivo, tipo coorte transversal, realizado por meio de revisão de prontuários médicos de pacientes submetidas a reconstrução mamária com lipoenxertia pela Divisão de Cirurgia Plástica do Hospital das Clínicas da FMRP-USP, no período de 2006 a 2010.
RESULTADOS: Foram selecionadas 18 pacientes, sendo que oito (44%) apresentaram tumor do tipo histológico ductal. Três pacientes (17%) foram submetidas a quimioterapia neoadjuvante, sendo que destas, duas (11%) foram submetidas também a quimioterapia adjuvante; nove (50%) foram submetidas apenas a quimioterapia adjuvante. Onze pacientes (61%) foram submetidas a radioterapia adjuvante, e treze (72%) fizeram tratamento hormonal. Quanto à reconstrução da mama, oito pacientes (44,4%) realizaram TRAM, seis (33,3%), expansor mais prótese e quatro (22,2%), grande dorsal mais prótese. O número de sessões de lipoenxertia variou entre um e quatro. Não foi identificado nenhum caso de recidiva tumoral locorregional.
CONCLUSÃO: Não foi evidenciado nenhum caso de recidiva tumoral locorregional, o que acrescenta, até o momento, confiabilidade e segurança à lipoenxertia como arsenal para os procedimentos que visam melhorar os resultados da reconstrução mamária após o tratamento oncológico.
Palavras-chave: Reconstrução de Mama; Câncer de Mama; Lipoenxertia; Recidiva Tumoral.
The treatment of breast cancer has greatly evolved in the last three decades due to technological advances and the development of new therapies. At the same time, breast reconstruction has become an essential part of cancer treatment, due to the recognition that it alleviates psychological issues caused by mastectomy, including a sense of loss of femininity, anxiety, depression, and changes in patient self-image and self-esteem1,2.
Currently, breast reconstruction is considered part of the treatment of breast cancer and is guaranteed by law. According to Article 1 of the Resolution of the Federal Council of Medicine of Brazil No. 1483/97, breast reconstruction, when indicated in order to correct deformity resulting from partial or total mastectomy, is an integral part of the treatment of the disease for which mastectomy was indicated.
Fat grafting has been used for many years in cosmetic surgery. The first reported use of the fat graft was in 1995, when Czerny described the transplantation of a lipoma of the lumbar region for the reconstruction of a breast defect3. With the development of liposuction techniques in the 1980s, the use of fat as a graft has spread, and it is now being used increasingly in patients with breast cancer to improve the results of breast reconstruction4,5.
Most published studies on fat grafting in breast reconstruction focus on technical issues, complications, esthetic results, and the effect on the radiological diagnosis of new tumors4,6,7. However, some recent studies have questioned the safety of fat grafting, suggesting that it may increase the risk of local tumor recurrence8-11. In addition, experimental studies have reported that adipose tissue can stimulate angiogenesis and tumor progression12-15.
OBJECTIVE
In light of this recent discussion, this study evaluated the recurrence rate of breast cancer in women undergoing fat grafting at this institution.
METHOD
A retrospective, cross-sectional cohort study wasconducted of patients who underwent delayed breast reconstruction after mastectomy. The patients were operated on by the Division of Plastic Surgery of the Ribeirão Preto Clinical Hospital-University of São Paulo (HCRP-USP), from 2006 to 2010. All selected patients underwent mastectomy, breast reconstruction, and fat grafting as one of the steps of treatment. Patients with recurrences, metastases or bilateral cancer, prior fat grafting, or who had less than two years of follow-up after the date of initial fat grafting, were excluded from the study.
The following data were evaluated: age of the patients; date of cancer surgery; date of reconstructive surgery; interval between surgeries; type of restorative surgery performed; characteristics of the tumor (histological type and presence of hormone receptors); whether the patient underwent chemotherapy, radiotherapy, and hormone therapy; number of fat grafting sessions; interval between reconstructive surgery and initial fat grafting; and diagnosis of locoregional tumor recurrence.
RESULTS
Eighteen patients who underwent breast reconstruction with complementary fat grafting after mastectomy were selected. Only six patients (33%) underwent mastectomy at the HCRP. All other reconstructions were delayed.
The mean age was 55 years (44-70 years). The cancer surgeries were performed between 1990 and 2008, and breast reconstruction occurred from 3 months to 8 years after the mastectomy (average of 3 years and 9 months).
Eight tumors were of ductal histological type(44%); the evaluation of the other 10 cases was compromised due to oncological treatment elsewhere, or due to failure to complete the medical record. Thirteen patients (72%) had hormone receptor-positive cancer (Table 1).
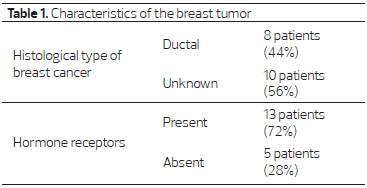
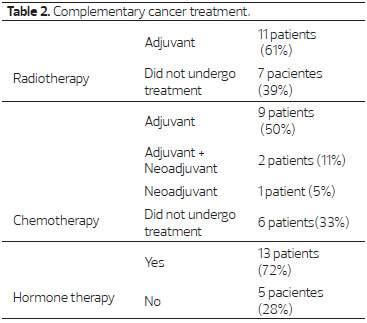
As complementary treatment to surgery, three patients (17%) underwent neoadjuvant chemotherapy, and of these, two (11%) were also subjected to adjuvant chemotherapy. Nine (50%) had only adjuvant chemotherapy. Eleven patients (61%) underwent adjuvant radiotherapy, and thirteen (72%) had hormonal therapy (Table 2).
Reconstruction with a transverse rectus abdominis myocutaneous (TRAM) flap was the most frequently performed surgery, totaling 8 patients (44.4%), followed by the use of an expander and prosthesis in 6 patients (33.3%), and reconstruction with a latissimus dorsi muscle flap and prosthesis in 4 patients (22.2%) (Figure 1).
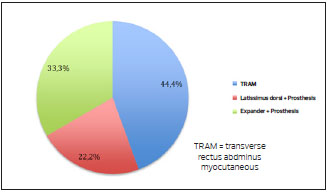
Figure 1. Type of reconstructive surgery performed on patients.
The number of fat grafting sessions varied from one to four (mean 1.6), and the time between the main reconstructive surgery and the first fat grafting ranged from six months to eight years (average of two years and three months) (Figure 2).
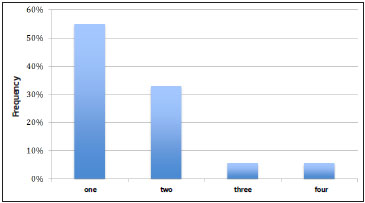
Figure 2. Number of fat grafting sessions performed on patients.
The time of follow-up after the last fat grafting session ranged from two to seven years (average of three years), and no cases of recurrence were observed in the eighteen patients evaluated.
DISCUSSION
Fat grafting has been used for many years in plastic surgery, and its use is becoming more widespread in breast reconstruction surgery3. Fat grafting improves the breast volume and the refinement of contours, optimizing the esthetic result of the previous reconstruction. There are many studies published on this topic, mostly on the technical issues, complications, cosmetic results and the effect of the procedure on the radiological diagnosis of new tumors4,5,7.
However, some recent studies have investigated the safety of fat grafting in patients undergoing cancer surgery, questioning whether it is a risk factor for an increase in locoregional recurrence. Lohsiriwat et al10. reported that adipocytes, preadipocytes, and progenitor cells can induce angiogenesis and cell growth, and also emphasized that the "tumor-stroma" interaction can potentially induce the reappearance of cancer by "fueling" dormant cancer cells. In 2012, Martin-Pandura et al12. noted the importance of understanding the role of different cells derived from adipose tissue, used for fat grafting, in post-surgery breast reconstruction.
More recently, Petit et al. published two studies that further explored this new field of discussion by posing questions and presenting important data. Petit et al.'s first study9 evaluated 321 patients who underwent breast cancer surgery associated with fat grafting, comparing them to a control group consisting of 642 patients who did not undergo fat grafting. The authors concluded that fat grafting appears to be a safe procedure for patients with breast cancer. However, when patients with intraepithelial tumor types (ductal or lobular) were specifically evaluated, there was a statistically significant increased risk of local recurrence in the group undergoing fat grafting.
Based on this observation, Petit led a new study in 20138, in which 59 patients with intraepithelial neoplasia submitted to fat grafting were evaluated, comparing them to a control group of 118 patients with the same characteristics of the study group, but who were not subjected to fat grafting. The study reported an increased risk of locoregional recurrence in patients with intraepithelial neoplasia submitted to fat grafting (18% had tumor recurrence, compared to 3% of controls).
Both of Petit's reports highlight the importance of new studies to evaluate the possibility that fat grafting increases the risk of tumor recurrence in women treated for breast cancer.
In this study, the mean follow-up time after the last fat grafting session was three years, which is sufficient to make a diagnosis of tumor recurrence; in Petit's last study, the average time between fat grafting and diagnosis of tumor recurrence was 12 months.
On our service, fat grafting has become an important tool, and its use has become increasingly common in breast reconstruction of patients with cancer; it is mainly indicated for refinement of the results achieved with other reconstruction techniques.
The profile of the patients included in this study is similar to that found in the literature. However, multiple factors adversely affect the profile, including the fact that many women started treatment elsewhere and were referred for follow-up at a late phase, the small number of patients analyzed, lack of information about the patients, lack of detailed documentation of their cancer treatment, and the characteristics of retrospective studies themselves. Nonetheless, all the patients studied had follow-up for cancer, reliably ensuring the absence of evidence for locoregional tumor recurrence.
In view of the recent published studies and due to the widespread use of fat grafting in breast reconstruction in cancer patients, further studies are required to reach safer conclusions. However, based on personal experience to date, fat grafting, appears to be a reliable and safe tool for treatments to improve the outcome of breast reconstruction after cancer treatment.
CONCLUSION
There have been no cases of locoregional recurrence in our series thus far, indicating the reliability and safety of fat grafting as a tool to improve the outcome of breast reconstruction after cancer treatment. However, recent reports suggest the need for further prospective and randomized studies to reach more definitive conclusions.
REFERENCES
1. Aston SJ, Beasley RW, Thorne CH. Grabb and Smith's Plastic Surgery, 5th ed. Lippincott-Raven Publishers, 1997.
2. Bostwick J. Breast reconstruction after mastectomy-recent advances. Cancer. 1990;66:1402-11.
3. Petit JY, Lohsiriwat V, Clough KB, Sarfati I, Ihrai T, Rietjens M, et al. The oncologic outcome and immediate surgical complications of lipofiling in breast cancer patients: a multicenter study - Milan - Paris - Lyon experience of 646 lipofilling procedures. Plast Reconstr Surg. 2011;128:341-6.
4. Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119(3):775-85.
5. Rosing JH, Wong G, Wong MS, Sahar D, Stevenson TR, Pu LL. Autologous fat grafting for primary breast augmentation: a systematic review. Aesth Plast Surg. 2011;35:882-90.
6. Rietjens M, De Lorenzi F, Rossetto F, Brenelli F, Manconi A, Martella S. Safety of fat grafting in secondary breast reconstruction after cancer. J Plast Reconstr Aesthet Surg. 2011;64:477-83.
7. Petit JY, Clough K, Sarfati I, Lohsiriwat V, Lorenzi F, Rietjens M. Lipofilling in breast cancer patients: from surgical technique to oncologic point of view. Plast Reconstr Surg. 2010;126:262e-3e.
8. Petit JY, Rietjens M, Botteri E, Rotmensz N, Bertolini F, Curigliano G et al. Evaluation of fat grafting safety in patients with intra-epithelial neoplasia: a matched-cohort study. Ann Oncol. 2013;24:1479-84.
9. Petit JY, Botteri E, Lohsiriwat V, Rietjens M, De Lorenzi F, Garusi C et al. Locoregional recurrence risk after lipofilling in breast cancer patients. Ann Oncol. 2012;23:582-8.
10. Lohsiriwat V, Curigliano G, Rietjens M, Goldhirsch A, Petit JY. Autologous fat transplantation in patients with breast cancer: "silencing" or "fueling" cancer recurrence? Breast. 2011;20:351-7.
11. Semprini G, Cattin F, Lazzaro L, Cedolini C, Parodi PC. About locoregional recurrence risk after lipofilling in breast cancer patients. Ann Oncol. 2012;23:802-3.
12. Martin-Pandura I, Gregato G, Marighetti P, Mancuso P, Calleri A, Corsini C et al. The white adipose tissue used in lipotransfer procedures is a rich reservoir of CD34 progenitors able to promote cancer progression. Cancer Res. 2012; 72(1):325-34.
13. Bertolini F, Lohsiriwat V, Petit JY, Kolonin MG. Adipose tissue cells, lipotransfer and cancer: a challenge for scientists, oncologists and surgeons. Biochim Biophys Acta. 2012;18(26):209-14.
14. Chandler EM, Seo BR, Califano JP, Eguiluz RCA, Lee JS, Yoon CJ et al. Implanted adipose progenitor cells as physicochemical regulators of breast cancer. Proc Natl Acad Sci USA. 2012;109:9786-91.
15. Espina V, Mariani BD, Gallagher RI, Tran K, Banks S, Wiedemann J et al. Malignant precursor cells pre-exist in human breast DCIS and require autophagy for survival. PLoS One. 2010;5:e10240.
1 - Resident Physician - Resident Physician of the Plastic Surgery Division, Department of Surgery and Anatomy of the Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
2 - Resident Physician - Resident Physician of the Plastic Surgery Division, Department of Surgery and Anatomy of the Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
3 - Visiting Physician - Visiting Physician of the Plastic Surgery Division, Department of Surgery and Anatomy of the Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
4 - Resident Physician - Resident Physician of the Plastic Surgery Division, Department of Surgery and Anatomy of the Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
5 - Professor- Professor of the Obstetrics and Gynecology Department of the Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
6 - Professor - Professor of the Department of Clinical Medicine of the da Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
7 - Attending Physician - Attending Physician of the Plastic Surgery Division, Department of Surgery and Anatomy of the Ribeirão Preto Faculty of Medicine, University of São Paulo, Brazil
8 - Physician, Titular member of the SBCP and SBQ - Chief of the Plastic Surgery Division of the HCFMRP-USP
Institution: Clinical Hospital of the Ribeirão Preto Faculty of Medicine of the University of São Paulo.
Corresponding author
Professor Jayme Adriano Farina Junior
Department of Surgery and Anatomy, Plastic Surgery Division, Ribeirão Preto Faculty of Medicine, University of São Paulo
Avenida Bandeirantes, 3900, 9º andar, Bairro Monte Alegre
14048-900 - Ribeirão Preto - SP, Brasil
Tel.: (55) (16) 3602-2593
E-mail: jafarinajr@fmrp.usp.br
Article submitted: December 9, 2013.
Article accepted: June 1, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter