

Original Article - Year 2014 - Volume 29 -
Aesthetic and reconstructive application of mammoplasty with the inferior dermal pedicle technique
Aplicação estética e reconstrutora da mamoplastia com pedículo areolado
ABSTRACT
INTRODUCTION: Reduction mammaplasty is one of the most common surgeries performed in the field of plastic surgery, and several techniques have been described. The inferior dermal pedicle technique, which is relatively unknown in Brazil, may have applications in both aesthetic and reconstructive surgery. The aim of the current study was to analyze the results of mammaplasty performed with this technique.
METHODS: Data were collected from a retrospective analysis of medical records. Study data also included data obtained through telephone contact with patients, photographic analysis, and patient profiles, as well as data on the purpose of the surgery, complications, satisfaction with results, and degree of sensitivity of the nipple-areolar complex (NAC).
RESULTS: During the study period, 74 patients underwent mammaplasty with the inferior pedicle technique (42 aesthetic reduction mammaplasties, 13 mammaplasties for immediate breast reconstruction following segmental resections, and 19 post-reconstruction symmetrization mammaplasties with other techniques). Complications occurred in 20 patients. Regarding the assessment of satisfaction by the patients, the outcome was rated as excellent in 62.16% of cases, good in 25.67%, and fair in 12.17%. In terms of the sensitivity of the NAC, 72.97% of patients reported no loss of sensitivity, 20.27% reported a small loss, 6.76% reported significant loss, and no patients reported a total loss of sensitivity.
CONCLUSIONS: The inferior pedicle reduction mammaplasty technique has good applicability both in aesthetic reconstructive surgeries and in immediate reconstructions (upper quadrantectomies) or symmetrizations, especially after the use of a transverse rectus abdominis myocutaneous flap. The technique offers a high degree of satisfaction with the results, a low rate of complications, a high degree of preservation of the sensitivity of the NAC, and good maintenance of the results.
Keywords: Mammaplasty; Reduction mammaplasty; Breast reconstruction; Inferior pedicle technique.
RESUMO
INTRODUÇÃO: A mamoplastia redutora é uma das mais frequentes cirurgias realizadas no âmbito da cirurgia plástica, sendo que diversas técnicas são descritas. A técnica do pedículo inferior areolado é uma técnica pouco difundida no Brasil, que pode ter aplicação tanto em cirurgias estéticas quanto reconstrutoras. O objetivo deste estudo foi analisar os resultados de mamoplastias realizadas com esta técnica.
MÉTODOS: Análise retrospectiva de prontuários, contato telefônico com as pacientes e análise fotográfica, identificando perfil das pacientes, finalidade da cirurgia, complicações, grau de satisfação e grau de sensibilidade do complexo aréolo-papilar (CAP).
RESULTADOS: No período analisado, 74 pacientes foram submetidas à mamoplastia com a técnica do pedículo inferior areolado (42 mamoplastias redutoras estéticas, 13 mamoplastias para reconstrução imediata de mama pós-ressecções segmentares, e 19 mamoplastias de simetrização pós-reconstrução com outras técnicas). Complicações ocorreram em 20 pacientes. Em relação à avaliação da satisfação pelas pacientes, o resultado foi considerado ótimo em 62,16% dos casos, bom em 25,67%, e regular em 12,17%. Quanto à sensibilidade do CAP, 72,97% das pacientes referiram não haver perda da sensibilidade, 20,27% referiram pequena diminuição, 6,76% referiram diminuição significativa e nenhuma relatou perda total da sensibilidade.
CONCLUSÕES: A técnica de mamoplastia redutora com pedículo inferior areolado apresenta boa aplicabilidade, tanto em cirurgias estéticas quanto reconstrutoras, seja em reconstruções imediatas (quadrantectomias superiores) ou em simetrizações, principalmente pós TRAM. Apresenta alto grau de satisfação com o resultado, baixa taxa de complicações, alta preservação da sensibilidade do CAP e boa manutenção do resultado.
Palavras-chave: Mamoplastia; Mamoplastia redutora; Reconstrução mamária; Técnica do pedículo inferior.
Excess breast tissue is usually associated with both physical and psychological discomfort. In addition to back pain, neck pain, and dermatitis, patients with macromastia also experience limitations regarding physical activity and describe considerable social inconvenience due to excess breast volume1.
Reduction mammaplasty is one of the most common surgeries performed in the field of plastic surgery. There is considerable debate regarding the optimal technique combining both safety and good functional and aesthetic results, and this continues to be a challenge for plastic surgeons.
Several surgical techniques have been described; the anatomical factors that influence the choice of technique include the volume of the breasts and the migration distance of the nipple-areola complex (NAC)2. In cases of reconstructive mammaplasty, tumor location and size are decisive factors in the selection of the technique3. The major concern in surgeries in which large volumes are reduced is the restriction of blood supply to the areola.
The blood supply to the NAC has long been understood. While the vascular supply of the NAC was initially attributed to the subdermal plexus, later studies showed that the vessels of the subdermal plexus are small and inadequate to perfuse the areola and that parenchymal perforating vessels are also required4,5. Preservation of the blood supply to the NAC in surgery thus requires preservation of an intact portion of the parenchyma.
Doubts about the viability of the NAC led some surgeons to prefer free nipple grafting instead of large transpositions6,7. Although preserving a natural looking pigmentation, amputation and grafting of the NAC lead to loss of projection, sensitivity, and lactation capability7. To avoid these complications, the inferior pedicle technique may be employed. Since its description by Ribeiro in 1973 and its presentation by Jurado in 1976, mammaplasty with the lower dermal pedicle technique has been widely used in North America, although the technique is not well known in Brazil1, 8-10.
Several studies have shown that with the maintenance of the NAC in the inferior dermoglandular pedicle, it may be possible to perform migration over a significant distance and still preserve a large number of perforating vessels, allowing their continued viability and improving overall postoperative sensitivity. In addition, this technique has proven to be safe and reproducible 1,10,11.
The inferior pedicle technique can also be used for breast reconstruction in resections of tumors in the lateral and medial upper quadrants when the residual breast tissue is used to fill the defects left following resection. Based on the size of the defect after partial mastectomy, careful handling of the proportions of the inferior pedicle allows it to fill the space left without much difficulty. However, when a large amount of skin needs to be resected, many advantages of conservative surgery are lost12.
OBJECTIVE
The objective of the current study was to analyze cases of mammaplasty performed by the author M.C.C. in the last 8 years in which the inferior pedicle technique was used, and to identify the age of patients, purpose of the surgery (cosmetic, reconstructive, or symmetrization), weight of resected tissue, complications, sensitivity of the NAC following surgery, and aesthetic satisfaction ratings assigned by patients and surgeons.
METHOD
A retrospective analysis of medical records was performed, identifying the patients who underwent breast reduction with the inferior dermal pedicle technique between January 2005 and January 2013. From the medical records, data related to patient age, purpose of the surgery (aesthetic breast reconstruction or breast symmetrization), occurrence and type of complications, need for refinements (outpatient procedures) and need for reoperation (hospital procedures) were collected. The weight of the surgical specimens was assessed through the pathology reports. A patient questionnaire was administered by telephone at least 6 months postoperatively, identifying the degree of satisfaction with the cosmetic results (excellent, good, fair, and poor) and the degree of sensitivity of the NAC (increase, maintenance, small loss, large loss, total loss). The aesthetic results (excellent, good, fair, and poor) were also evaluated by participating surgeons, through pre- and postoperative photographic records; the description of symmetry, the maintenance of the results, and the maintenance of the position of the NAC were taken into account in the medical analysis.
Preoperative Evaluation: All patients underwent a complete preoperative evaluation, including clinical history and physical examination, laboratory and cardiac examinations, and radiological breast exams (ultrasound and mammography). The inferior pedicle technique was indicated for patients with large breasts and severe ptosis, in whom there was a need for a considerable lift of the NAC, with a risk of vascular damage.
Operative Technique: The marking of Pitanguy points A, B, and C was done as originally described. Subsequently, a long inferior pedicle covering the NAC was marked in the central portion of the breast, extending points B and C inferiorly to the inframammary crease. A solution of saline and epinephrine (1:300,000) was infiltrated at the base of the breasts. A periareolar incision was made with decortication of the entire area of the pedicle. This was followed up with an incision surrounding the pedicle in the anteroposterior direction, to the fascia. It is important at this point to preserve the posterior base of the pedicle and maintain its attachment to the pectoral fascia, preserving the maximum amount of perforating vessels. The next step in the surgery was to fix the pedicle areolate on the sides of its lower base, close to the inframammary crease. The upper pedicle containing the NAC should be free in order to facilitate positioning of the areola to confer volume and projection to the breast mound. The next steps were to model the breast with resection of dermoglandular excesses of the lateral and medial poles, mount the breast, suture the NAC in its new position, and place other sutures, with placement of a drain in the lateral portion of the breast, with the outlet in the lateral portion of the incision (Figure 1). Liposuction was performed for aesthetic refinement in the lateral region of the breasts when needed.
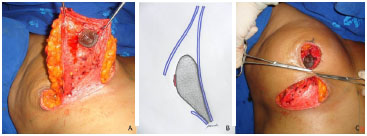
Figure 1. Surgical Technique: In A, isolated inferior pedicle; B, schematic showing the inferior pedicle with its base attached to the pectoral fascia; C, inferior pedicle with its fixed side portions and construction of the breast.
In reconstructive surgery, markup and programming of the reconstruction were performed previously, according to the location of the tumor, with the participation of all professionals involved. Partial mastectomy was performed in all cases by the mastology team. The construction of the affected breast and contralateral breast symmetrization were performed using the inferior pedicle technique.
RESULTS
In the reporting period (January 2005 to January 2013), of a total of 227 patients who underwent reduction mammaplasty (aesthetic, breast reconstruction, or symmetrization), the inferior pedicle technique was used in 74 (32.59%). The average age of the patients was 44.19 years (range, 22-68 years) and the average weight of the resected tissue was 559.47 g per breast (range, 84-1200g). The minimum follow-up period was 6 months.
Regarding the purpose of the surgery, 42 were aesthetic reduction mammaplasties (bilateral) (Figure 2). Treze were mammaplasties for immediate breast reconstruction, following segmental resection of localized tumors (bilateral, either due to bilateral tumors or as a result of unilateral tumors, with contralateral breast symmetrizations performed using the same technique) (Figure 3); and 19 were post-reconstruction symmetrization mammaplasties performed using other techniques (unilateral) (Figure 4), completed after adjuvant treatments. The total number of breasts operated on in the study was 129.
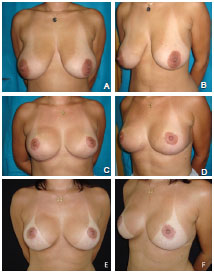
Figure 2. A case of aesthetic reduction mammaplasty using the inferior pedicle technique. In A and B, preoperative aspect. In C and D, 6-month postoperative aspect. In E and F, 18-month postoperative aspect.
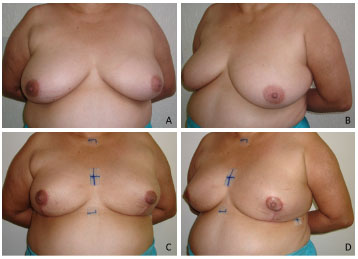
Figure 3. A case of an immediate reconstructive mammaplasty using the inferior pedicle technique (partial mastectomy due to breast cancer). In A and B, preoperative aspect. In C and D, 2-month postoperative aspect.
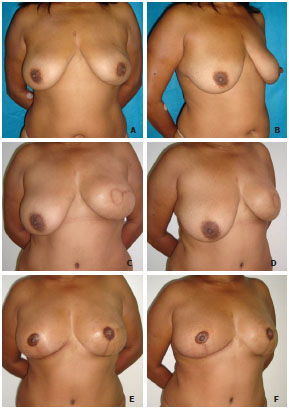
Figure 4. Case of symmetrization mammaplasty. In A and B, preoperative aspect. In C and D, aspect 3 years after left mastectomy and immediate reconstruction with myocutaneous rectus abdominis muscle flap. In E and F, aspect 3 months after symmetrization mammaplasty using the inferior pedicle technique to the right and mammaplasty in the left neobreast with reconstruction of the nipple-areola complex.
Complications occurred in 20 patients (27.02%), with a total number of 27 complications. The most common was suture dehiscence of the vertical scar or the inverted T, which occurred in 12 patients, followed by unsightly scar and "dog ear" (7 patients), seroma (5 patients), asymmetry (2 patients), and partial necrosis of the NAC (1 patient). Refinement surgeries were performed in 14 patients, 7 due to dehiscence and 7 due to unsightly scars and "dog ear." Reoperation was performed on a patient who had undergone unilateral post-reconstruction symmetrization with a rectus abdominis muscle flap, which resulted in significant asymmetry. No cases of infection or systemic complications occurred. In addition, no case of worsening due to complications of the immediate reconstruction was observed on oncological follow-up.
Regarding the assessment of satisfaction, the questionnaire completed by the patients indicated the outcome as excellent in 62.16% (46) of cases, good in 25.67% (19), and fair in 12.17% (9) (Figure 5A). In the assessment of surgeons, the result was excellent in 55.40% (41) of cases, good in 32.43% (24), fair in 9.46% (7), and poor in 2.71% (2) (Figure 5B). The maintenance of the NAC positioning at the apex of the breast mound was observed in 95.95% of patients.
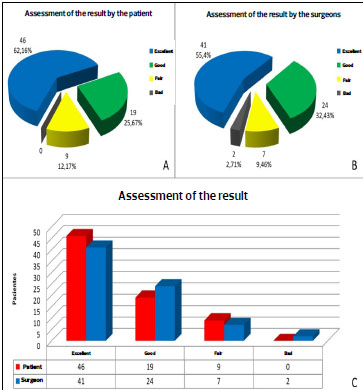
Figure 5. Assessment of the outcome by the patients. In B, outcome evaluation by surgeons. In C, chart comparing the evaluation of the results given by the patient and the surgeons.
As for the sensitivity of the NAC, 72.97% (54) of patients reported no loss of sensitivity, 20.27% (15) reported a slight loss, 6.76% (5) reported a significant loss, and no patients reported a total loss of sensitivity (Figure 6).
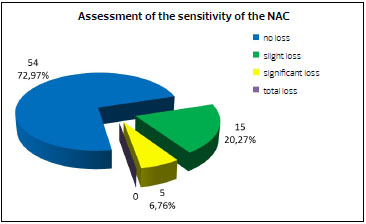
Figure 6. Graph illustrating the assessment of the sensitivity of the nipple-areolar complex (NAC) by patients.
DISCUSSION
The debate regarding the best among the various breast reduction techniques reflects the difficulty in creating the ideal breast, and also demonstrates the need for various techniques to provide the best treatment for each particular case1.
Due to dissatisfaction with cosmetic results, particularly with extensive scarring, some surgeons have chosen to use techniques that employ smaller incisions. The periareolar reduction technique, which only results in a periareolar scar, is the most widely accepted among the various proposed techniques. However, it is difficult to remove a large amount of tissue to be resected at risk of compromised vascular supply to the NAC13. These techniques are more laborious, have a higher complication rates, require a long learning curve, and in many cases generate irreproducible results1.
On the other hand, a technical option for very large breasts with significant ptosis would be free nipple graft, initially described by Thorek14, but this option implies loss of projection, sensitivity, and lactation capacity 7.
The inferior pedicle technique is easily reproducible without a significant increase in surgical time, can be employed in breasts of varying shapes and sizes, has a low complication rate, allows the important maintenance of sensitivity and nipple erection, and is coupled with high patient satisfaction10.
According to a study published by Rohrich in 2004, the inferior pedicle technique was the most frequently used by 44.1% of the surgeons participating in the study1. In the present study, 32.59% of the reduction mammaplasties performed by the author M.C.C. were performed using the inferior pedicle technique.
In this analysis, 43.24% of the surgeries were performed for a reconstructive purpose, either for immediate breast reconstruction following segmental resections or unilateral post-reconstruction breast symmetrization. In localized tumor resections, especially those in the medial and upper lateral quadrants of the breast, the inferior pedicle technique offered good versatility3,12. In cases of unilateral flap reconstruction, we observed that the contralateral symmetrization mammaplasty should not be performed at the same time as the first surgery and should be considered after analysis of the long-term results of the reconstructed breast. The effects of radiotherapy in one breast vary from an increase in volume due to chronic edema to size reduction as a result of tissue atrophy12. In all cases of symmetrization, the initial breast reconstruction was performed with a transverse rectus abdominis myocutaneous (TRAM) flap. The main objective of symmetrization using this technique was an attempt to maintain the NAC on the front of the breast to preserve symmetry. The other mammaplasty techniques have a tendency to allow the NAC to drop over the years. Mammaplasty for reconstructive purposes has not been found to result in impairment in patients, and on the contrary, attenuation of the feeling of mutilation following mastectomy leaves them more motivated to pursue adjuvant treatment3.
Complications in inferior pedicle mammaplasty occur in 22.1-59% of cases, varying with the criteria of each surgery6,11,15. In the current series, the complication rate was 27.02%, with an altered scar (dehiscence, unsightly scar) being the most common, as also found by O'Grady15. We observed dehiscence as a consequence of breast closure using thin skin flaps. There was an improvement in the incidence of this complication following the use of thicker lateral and medial subcutaneous flaps. One of the most feared complications in mammaplasty, necrosis of the NAC, partially occurred in one breast (0.77%) in the present study and was attributed to excessive compression of the breast in the immediate postoperative period; total necrosis of the NAC has a low incidence when the inferior pedicle technique is used6,15,16. This low occurrence of necrosis is probably related to the fact that there is no rotation or compression of the vascular pedicle. Moreover, both dermal and glandular preservation occurs with perforating vessels.
Regarding the satisfaction with the surgical results in the current study, there was an excellent or good degree of satisfaction in 87.83% of cases, both in the evaluation by the patients and the surgeons, showing a similarity in ratings (Figure 5C). When referring to their satisfaction, patients also take into account the improvement in quality of life provided by the operation, given the existing discomfort caused by the volume and breast ptosis or the psychological stress of mastectomy; however, later analysis, as performed, favors the aesthetic point of view. Surgeons, in turn, make a judgment based on what they know to be an achievable result in each case. According to Boechat et al., techniques that use the inferior pedicle evolve with a substantial increase in the vertical component of the scar, although the authors do not describe in detail its position/fixation to the pedicle17. With the technique used in the present study, the fixation of the pedicle in its lower portion is held with some tension, spreading and pulling the pedicle upwardly so that there would be no excess tissue in the lower quadrant of the breast. This may explain why a good maintenance of long-term outcomes was observed, in addition to the maintenance of the position of the NAC (in the breast cone apex), although no objective analysis was performed through measurements, as was done in the report by Boechat et al.
The loss of sensitivity and erectile function of the NAC can be dramatic for some patients. Techniques that use a superior pedicle, with the requirement for tissue resection at the base of the breast, have higher rates of permanent reduction in the sensitivity of the NAC18. Several studies have shown that the use of an inferior pedicle provides a quick recovery of the sensitivity of the NAC, attaining preoperative levels18-20. Among the patients in the present study, there was complete maintenance of NAC sensitivity in 72.97% of cases, and in no case was there complete loss of sensitivity (Figure 6).
CONCLUSION
The inferior pedicle breast reduction technique has good applicability in aesthetic and reconstructive surgeries, both in immediate reconstructions (upper quadrantectomies) and symmetrizations, especially after TRAM flap use. The high degree of satisfaction with the cosmetic results observed both by patients and by surgeons certifies the acceptability of the technique and the proper maintenance of the results. The low rate of complications and the good preservation of the sensitivity of the NAC demonstrate the safety of the technique. Thus, the nipple free graft should be reserved for cases in which intraoperative vascular involvement is clearly observed.
REFERENCES
1. Rohrich RJ, Gosman AA, Brown SA, Tonadapu P, Foster B. Current preferences for breast reduction techniques: a survey of board-certified plastic surgeons 2002. Plast Reconstr Surg. 2004;114(7):1724-33.
2. Hammond DC, Loffredo M. Breast eeduction. Plast Reconstr Surg. 2012;129(5):829e-39e.
3. Munhoz AM, Montag E, Arruda E, Aldrighi C, Filassi JR, de Barros AC, Piato JR, et al. Reliability of inferior dermoglandular pedicle reduction mammaplasty in reconstruction of partial mastectomy defects: surgical planning and outcome. Breast. 2007;16(6):577-89.
4. Palmer JH. The vascular territories of the anterior chest wall. Br J Plast Surg. 1986;39:287-99.
5. Makajima O, Imanishi N, Aiso S. Arterial anatomy of the nipple areola complex. Plast Reconstr Surg. 1995;843-845.
6. Gerzenshtein J, Oswald T, McCluskey P, Caplan J, Angel MF. Avoiding free nipple grafting with the inferior pedicle technique. Ann Plast Surg. 2005;55(3):245-9.
7. Lacerna M, Spears J, Mitra A, Medina C, McCampbell E, Kiran R, et al. Avoiding free nipple grafts during reduction mammaplasty in patients with gigantomastia. Ann Plast Surg. 2005;55(1):21-24
8. Ribeiro L, Backer E. Mastoplastia com pedículo de seguridad. Rev Esp Cir Plast 1973;16:223-34.
9. Jurado J. Plásticas mamárias de redução baseadas em retalho dérmico vertical monopediculado. Anais XII - Congresso Brasileiro de Cirurgia Plástica 1976;p29.
10. Bezerra FJF, Moura, RMG, Silva Júnior VV. Mamoplastia redutora e simetrização de mama aposta em reconstrução mamária utilizando a técnica de pedículo inferior. Rev Bras Cir Plást. 2007;22(1):52-59.
11. Scott GR, Carson CL, Borah GL. Maximizing outcomes in breast reduction surgery: a review of 518 consecutive patients. Plast Reconstr Surg. 2005;116(6):1633-41.
12. Kronowitz SJ, Hunt KK, Kuerer HM, Strom EA, Buchholz TA, Ensor JE, et al. Practical guidelines for repair of partial mastectomy defects using the breast reduction technique in patients undergoing breast conservation therapy. Plast Reconstr Surg. 2007;120(7):1755-68.
13. Lee TJ, Eom JS. Periareolar reduction mammaplasty utilizing the inferior dermal pedicle. Aesthetic Plast Surg. 1999;23(5):331-6.
14. Thorek M. Possibilities in the reconstruction of the human form. N Y Med J. 1922;116:572.
15. O'Grady KF, Thoma A, Dal Cin A. A comparison of complication rates in Large and small inferior pedicle reduction mammaplasty. Plast Reconstr Surg. 2005;115(3):736-42.
16. Zambacos GJ, Mandrekas AD. Complication rates in inferior pedicle reduction mammoplasty. Plast Reconstr Surg. 2006;118(1):274-5.
17. Boechat HR, Rodrigues FH, Miranda ES, Castro VM, Souza VE, Leão CE. Evolução da posição do complexo aréolo-mamilar e da extensão das cicatrizes após mamoplastia redutora com retalho de pedículo inferior areolado. Rev Bras Cir Plást. 2008;23(3):167-172.
18. Schlenz I, Rigel S, Schemper M, Kuzbari R. Alteration of nipple and areola sensitivity by reduction mammaplasty: a prospective comparison of five techniques. Plast Reconstr Surg. 2005;115(3):743-751.
19. Mofid MM, Dellon AL, Elias JJ, Nahabedian MY. Quantitation of breast sensibility following reduction mammoplasty: A comparison of inferior and medial pedicle techniques. Plast Reconstr Surg. 2002;109(7):2283-8.
20. Nahabedian MY, Mofid MM. Viability and sensation of the nipple-areolar complex after reduction mammaplasty. Ann Plast Surg. 2002;49(1):24-31.
1 - Plastic surgeon, Full member of the BSPS - Preceptor of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
2 - Resident of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
3 - Plastic surgeon, Full member of the BSPS - Regent of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
4 - Plastic surgeon, Full member of the BSPS - Preceptor of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
5 - Plastic surgeon, Full member of the BSPS - Preceptor of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
6 - Resident of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
7 - Resident of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
8 - Resident of the Plastic Surgery Department, Hospital Daher Lago Sul, Brasilia, DF, Brazil
Institution: Clínica Dra. Marcela Cammarota.
Corresponding author:
Marcela Caetano Cammarota
SMHN, Quadra 2, Bloco C, Edifício Dr. Crispim, sala 1314 e 1315 - Asa Norte
Brasília, DF, Brazil CEP 72000-000
Telefone: (61) 3425-3340
E-mail: marcelacammarota@yahoo.com.br
Article received: January 13, 2014
Article accepted: June 1, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter