

Original Article - Year 2014 - Volume 29 -
Epidemiology of facial trauma at the plastic surgery and burns service of the Santa Casa de Misericórdia de São José do Rio Preto
Epidemiologia dos traumas de face do serviço de cirurgia plástica e queimados da Santa Casa de Misericórdia de São José do Rio Preto
ABSTRACT
INTRODUCTION: Trauma is a major public health problem in all countries, and injuries involving the facial region are very common. This study aims to assess the epidemiological data of patients who suffered facial trauma with fracture.
METHODS: Epidemiological study conducted on 92 patient records. Individuals with facial trauma of any intensity presenting between January 2009 and January 2013 were selected and grouped according to the etiology and location of fractures. Data were presented as absolute values and percentages.
RESULTS: There was a higher prevalence of male patients. The most frequent cause of facial trauma was interpersonal violence in most groups, except for those over 45 years old, for whom the predominant causes were falls and car accidents. The frequency of the causes varied according to age: <18 years, 19-25 years old, 26-35 years old, 36-45 years and> 45 years. Seventy-five percent of mandibular fractures were unilateral and 25% bilateral. Surgical fixation with plates was the most common treatment. In our study, fourteen patients had postoperative complications.
CONCLUSION: There is a need for systemized care for facial trauma. The variation in the age range found among the studied patients demonstrates that facial trauma includes individuals of any age, although it is more common among young people. We believe that this epidemiological study will enable the improvement of the quality of care for patients with facial trauma.
Keywords: Epidemiology; Facial Bones/injuries; Maxillofacial Fractures; Nasal fracture; Facial Trauma.
RESUMO
INTRODUÇÃO: O trauma é um dos principais problemas de saúde pública em todos os países, sendo os que acometem a região facial muito frequentes. O presente trabalho objetiva avaliar dados epidemiológicos de pacientes que sofreram trauma de face com fratura.
MÉTODOS: Estudo epidemiológico realizado por meio dos prontuários de 92 pacientes. Foram selecionados indivíduos com trauma facial de qualquer intensidade, no período de janeiro de 2009 a janeiro de 2013, e agrupados de acordo com a etiologia e a localização das fraturas. Os dados coletados foram apresentados em valores absolutos e porcentagens.
RESULTADOS: Houve prevalência de pacientes do sexo masculino. A etiologia do trauma de face mais encontrada foi a violência interpessoal, observada na maioria dos grupos, exceto naquele acima de 45 anos, cuja predominância etiológica foi de queda e acidente de automóvel. A incidência das causas variou de acordo com a faixa etária: < 18 anos, de 19 a 25 anos, de 26 a 35 anos, de 36 a 45 anos e > 45 anos. Setenta e cinco por cento das fraturas de mandíbula foram unilaterais e 25%, bilaterais. O tratamento cirúrgico de fixação com placas foi o mais utilizado. No nosso estudo, catorze pacientes apresentaram complicação pós-cirúrgica.
CONCLUSÃO: Há necessidade de um atendimento sistematizado para os traumas faciais. A variação na faixa etária encontrada entre os pacientes estudados demonstra que o trauma facial abrange indivíduos em qualquer idade, embora seja maior entre os jovens. Acreditamos que o presente estudo epidemiológico possibilitará a melhora da qualidade no atendimento aos pacientes com trauma facial.
Palavras-chave: Epidemiologia; Ossos Faciais/Lesões; Fratura Maxilomandibular; Fratura Nasal; Trauma de Face.
Trauma is a major public health problem in all countries, regardless of their socio-economic development. It is the third most common cause of death in the world, surpassed only by cancer and cardiovascular disease. Approximately 60 million people suffer from some type of trauma per year, accounting for one in six hospital admissions1,2.
Injuries from external causes occupy the third position as a mortality factor, representing 15.1% of death causes worldwide, with traffic accidents the ninth specific cause of disability and premature death3,4.
Even when it does not kill, trauma can cause devastating injuries, and generate emotional consequences and deformities. As such, trauma has a significant economic impact on healthcare systems 5,6. Treatment mainly involves the specialties of trauma, ophthalmology, plastic surgery, maxillofacial surgery, and neurosurgery. A delay in treating patients with severe craniofacial involvement can lead to permanent damage or death5.
Facial trauma is among the most frequent diagnosis in patients of a general emergency service, either alone or associated with multiple trauma7.
The management of individuals affected by facial trauma should be systematic and multidisciplinary in order to provide a correct sequence of treatment in severe cases and reduce the possibility of fractures being overlooked in cases of mild trauma7.
In big cities, and especially in services related to educational institutions, the diagnosis and management of these lesions are always discussed among health professionals in order to prevent late sequelae that are often difficult to treat. The data available on facial trauma also comes from these institutions7.
Knowledge of facial trauma data, regarding the prevalence according to sex, cause of trauma, treatment methods used and complications, is of paramount importance for a better understanding of the problem in order to contribute to the implementation of preventive, educational and technical measures, which are still considered scarce in Brazil7,15. Facial trauma is especially relevant as there is a high rate of traumatic facial lesions compared to injuries in other body areas, because this region of the body is usually exposed without external protection16.
OBJECTIVE
This study aimed to evaluate the epidemiological data, gathered through outpatient records and the SAME (Medical File and Statistics Service) database, of patients who suffered facial trauma with fracture, and who underwent surgical treatment by Plastic Surgery and Burns team of the Santa Casa de Misericórdia de São José do Rio Preto, from January 2009 to January 2013, in order to propose prevention policies to the governing bodies involved.
METHOD
This epidemiological study was conducted with data from 92 patients treated as outpatients by the Plastic Surgery and Burns team, Santa Casa de Misericordia de São José do Rio Preto. Individuals with facial trauma of any intensity who underwent surgery were selected between January 2009 and January 2013, regardless of sex, age, or ethnicity. These data were collected by accessing the SAME records of the institution and evaluating the examinations performed in each case.
A protocol was developed to collect information on age, sex, ethnicity, injury etiology, length of stay, identified fractures, treatment given, and complications. Patients were grouped according to etiology: 1- interpersonal violence; 2- falls; 3- motorcycle accident; 4- car accident; 5- bicycle accident; 6- sports; 7- trampling; 8- firearm; 9- others. The term "fall" in this study refers to sports accidents, simple fall or falls from ladders and scaffolding.
Fractures were classified as: mandibular (ramus, body, coronoid process, condylar, symphysis, parasymphysis, angle of mandible), zygomatic, malar, nasal, alveolar process, frontal and orbital; unilateral or bilateral; compound or simple. Fractures were considered single-site when there was only one bone involved and multiple where two or more bones were involved.
Following preoperative tests, the patients in the study underwent surgery in the operating room under general anesthesia, according to the service protocol. In cases that required rigid internal fixation, titanium miniplates and screws were used, with or without maxillomandibular blocks and Erich arch bars.
All patients with facial trauma who refused the surgical procedure or who received conservative treatment were excluded from the survey.
This study was approved by the Research Ethics Committee of the hospital.
Data were analyzed using the Epi Info (version 3.5.4) and Microsoft Excel 2007 software, and are presented in absolute numbers and percentages.
RESULTS
The analysis of the medical charts revealed that 76% of patients were male (Figure 1), with a mean age of 34.34 years and range 8-69 years. There was predominance (72%) of Caucasian patients.
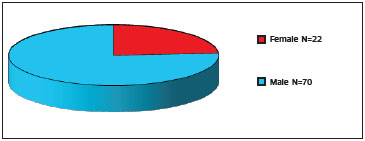
Figure 1. Distribution of patients according to sex
The etiology of facial trauma found was classified into the following: interpersonal violence (31.52%), fall (20.65%), motorcycle accident (19.57%), car accidents (16.3%), bicycle accident (7.61%), firearms (1.09%), other (3.26%) (Table 1). We found no cases related to trampling.

The frequency of the causes cited varied according to age. Patients were divided into five age groups: <18 years (N = 10, 10.87%), 19-25 years (N = 25, 27.17%), 26-35 years (N = 16, 17.39%), 36-45 (N = 21, 22.83%) and > 45 years old (n = 20, 21.74%). Interpersonal violence was a major cause found in all groups, except for the > 45 group, in which the major causes of trauma were falls and car accidents, in equal proportion. It was noted that the percentage of trauma cases caused by motorbike in the 19-25 group was equivalent to victims of interpersonal violence (Table 2).

The length of hospital stay ranged from 1 to 9 days, and the majority of hospitalized patients (94.6%) were in the hospital for between 24 and 72 hours.
Surgical treatment using fixation plates was the most frequently used method (52.17%), followed by nasal fracture reduction (30.77%). In our study, 14 patients had postoperative complications.
75% of the mandibular fractures found were unilateral and 25% bilateral. The most commonly affected mandibular fracture locations were the body, condyle and parasymphysis (Figure 2). In the presence of violence-associated facial trauma, fractures mainly affected the malar and the orbit, observed in 8 patients (30.77%). Mandibular, violence-associated and nasal fractures made up the majority of cases and affected a total of 78 patients (Table 3).

Figure 2. Type of mandibular fracture (%)


DISCUSSION
When treating facial trauma, there is a need for systematic care in order to avoid complications that are often difficult to treat and cause unnecessary additional cost. There is a strong prevalence of these injuries among patients in any emergency; in large cities, the diagnosis of facial fractures appears to be rarely missed, while in the small emergency rooms of Brazil due importance is not always given to this type of fracture, particularly in low intensity trauma and when the middle third of the face is affected. In such cases, the changes are discrete and there is often a greater concern with soft tissue lesions than with skeletal ones7. This study sought to assess facial trauma in a service in the interior of the country through the evaluation of epidemiological data and treatment regimens, which has not been previously reported in the literature.
Patients were predominantly male, corroborating the findings in other studies7-14.
Studies show that when the main cause of trauma is a car accident, there is generally a higher rate of mandibular fractures, while in trauma cases related to interpersonal violence, fractures of the zygomaticomaxillary complex predominate7.
There is a global trend towards an increase of female victims of facial trauma, because of the increase in risk factors related to this type of trauma. Greater involvement in physical activity, the increase in the number of female drivers and the rise in the number of assaults in cities, together with the growing participation of women in extra-domiciliary activities, are increasing their risk to that of men 14.
The variation in the age range found among the studied patients reveals that facial trauma may include individuals at any age. However, one can observe an increased prevalence of trauma in the group aged 19 to 25 years, due to increased exposure of these patients to risk factors. The literature indicates that the peak incidence is between 21 and 30 years due to the higher propensity for urban violence and the psychosocioeconomic conflicts experienced by young individuals14,16,17. This group accounted for 32.61% of our sample.
Regarding the etiologies found in our study, trauma related to traffic accidents make up the majority of cases, as the sum of events involving motorcycles (19.57%) and automobiles (16.3%). We observed that 31.52% of patients experienced interpersonal violence, which alone was the most frequent cause of trauma. Some studies have shown a predominance of trauma related to traffic accidents, followed by interpersonal violence 14. However, there is evidence that interpersonal violence is currently leading in these statistics14. This is mainly due to public policies aimed at greater control of excess speed on the roads and promoting the use of seat belts. In addition, the prohibition of drunk driving and the introduction of "air bags" and side protection bars have decreased the incidence of facial fractures, as well as the complexity of these lesions14. As trauma caused by car accidents has been reduced, motorcycle accidents are now a major cause of trauma in the 19-25 and 36-45 years age groups. The majority of patients aged 45 years suffered trauma due to falls or car accidents, which in this study affected the same number of individuals in this group. Some authors associate the low incidence of trauma in the elderly with the reduced social or sports activities undertaken by the elderly, as well as the lower extra-domiciliary exposure of older persons14,16. The most frequent causes of trauma among patients under 18 were interpersonal violence and falls. According to Silva et al.14 and Rodrigues et al.16, the low incidence of childhood trauma (when this group is compared to young adults, for example) is due to the attention of family members, the increase in the amount of time spent at home and the increased care received in childhood.
When looking at which facial regions were injured in trauma, we found that most of the cases were mandibular fractures followed by associated lesions and nasal fractures. The associated lesions in most cases involved malar and orbital fractures (8 cases). Further fractures involved were: malar, orbit and zygoma (N=5); zygoma and orbit (N=3); malar and zygoma (N=2). The most common fracture site reported varies in the literature, but several studies point to the mandible as the most affected bone in facial trauma7,14,16,17, besides the zygomaticomaxillary complex and nose7,16,17. The fact that the mandible is the anatomical region that appears to be affected more often is possibly because this is the only mobile bone of the face, so it would be more vulnerable when receiving strong impacts and fracture14.
As to the various causes of mandibular fractures, 12 patients in the study had trauma due to car or motorcycle accidents, which represented 13.04% of the cases studied.
There are studies that report the same male to female ratio among patients with facial trauma, such as the study by Pereira et al.19 in the São Paulo Hospital.
Filho et al.20, evaluated 166 patients with mandibular fractures in São Paulo, and observed a predominance of mandibular body fractures (28.5%), followed by condyle fractures (26.6%). These data are in agreement with our findings, which also indicated a predominance of lesions of the mandibular body (34.21%) and condyle (23.68%). We did not observe fractures of the mandible coronoid process in our study.
The most common treatment method was internal fixation with plates and screws, which was used in 52.17% of cases.
The overall complication rate was 14.13%, affecting 13 patients.The leading cause of complication was deviation following closed reduction of nasal fractures, which was observed in 4 individuals. The complication rate was equivalent to that found by Filho et al.20, 15.6%. Other complications observed in our sample were three patients with abscess in the mandibular region, all of which were subsequently drained; two with fibrosis in the nasal dorsum region after fracture reduction; one who presented with a surgical wound infection in the mandibular region; one who developed epiphora after orbital fracture reduction surgery; another who developed paresthesia within the fracture, following poor postoperative closure; and one with extrusion of the fixation material.
CONCLUSION
Based on the epidemiological data obtained in this study, men between 19 and 25 years of age are the most affected by maxillofacial trauma. This is due to greater exposure to risk factors such as urban violence, psychosocial conflicts, and sporting activities. These epidemiological data are important for an institution that seeks an improvement in prevention measures, education and service systematization.
REFERENCES
1. Batista SE, Baccani JG, Silva RA, Gualda KP, Vianna Jr R. Analise comparativa entre os mecanismos de trauma, as lesões e o perfil de gravidade das vitimas, em Catanduva-SP. Rev Col Bras Cir. 2006;33(1):6-10.
2. Hoyt DB, Coimbra R, Winchell RJ. Tratamento de trauma agudo. In: Townsend Jr CM, editores. Sabinston tratado de cirurgia: as bases biológicas da prática cirúrgica moderna. 16º ed. Rio de Janeiro: Guanabara Koogan; 2003. p. 339-40.
3. Costa CD, Scarpelini S. Avaliação da qualidade do atendimento ao traumatizado através do estudo das mortes em um hospital terciário. Rev Col Bras Cir. 2012;39(4):249-254.
4. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349(9063):1436-42.
5. Sastry SM, Sastry CM, PAUL BK, Champion HR. Leading causes of facial trauma in the major trauma outcome study. Plast Reconstr Surg. 1995;95(1):196-7.
6. Wulkan M, Parreira Junior JG, Botter DA. Epidemiologia do Trauma facial. Rev Assoc Med Bras. 2005;51(5):290-5.
7. Motta MM. Análise epidemiológica das fraturas faciais em um hospital secundário. Rev Bras Cir Plast. 2009;24(2):162-9.
8. Montovani JC, Campos LM, Gomes MA, Moraes VR, Ferreira FD, Nogueira EA. Etiologia e incidência das fraturas faciais em adultos e crianças: experiência em 513 casos. Rev Bras Otorrinolaringol. 2006;72(2):235-41.
9. Silva CJ, Ferreira EF, Paula LP, Naves MD, Vargas AM, Zarzar PM. A violência urbana contra crianças e adolescentes em Belo Horizonte: uma história contada através dos traumas maxilofaciais. Physis Rev Saúde Coletiva. 2011;21(3):1103-20.
10. Andrade Filho EF, Fadul JrR, Azevedo RA, Rocha MA, Santos RA, Toledo SR, Cappucci A, Toledo CS, Ferreira LM. Fraturas de Mandíbula: analise de 166 casos. Rev Ass Med Brasil. 2000;46(3):272-6.
11. Scariot R, Oliveira IA, Passeri LA, Rebellato NL, Muller PR. Maxillofacial injuries in a group of Brazilian subjects under 18 years of age. J Appl Oral Sci. 2009;17(3):195-8.
12. Franciozi CE, Tamaoki MJ, Araujo EF, Dobashi ET, Utumi CE, Pinto JA, Ishida A. Trauma na infância e adolescência: epidemiologia, tratamento e aspectos econômicos em um hospital público. Acta Ortop Bras. 2008;16(5):261-5.
13. Morano FG, Sampaio MM, Freitas RS, Alonso N, Ferreira MC. Analise de 126 fraturas de face em crianças menores de 12 anos. Rev Col Bras Cir. 1997;25(03):201-204.
14. Silva, JJL, Aurélio AA, Lima S, Melo IF, Maia RC, Filho TR. Trauma facial: análise de 194 casos. Rev Bras Cir Plast. 2011;26(1):37-41.
15. Borghese B, Calderoni DR, Passeri LA. Estudo retrospectivo da abordagem das fraturas nasais no Hospital de Clínicas da Unicamp. Rev Bras Cir Plast. 2011;26(4):608-12.
16. Rodrigues, FH, Miranda ES, Souza VE, Castro VM, Oliveira DR, Leão CE. Avaliação do trauma bucomaxilofacial no Hospital Maria Amélia Lins da Fundação hospitalar do estado de Minas Gerais. Rev Bras Cir Plast. 2006;21(4):211-6.
17. Silva JJ, Lima AA, Dantas TB, Frota MHA, Parente RV, Lucena AL. Fratura de mandíbula: estudo epidemiológico de 70 casos. Rev Bras Cir Plast. 2011;26(4):645-8.
18. Macedo JL, Camargo LM, Almeida PF, Rosa SC. Mudança etiológica do trauma de face de pacientes atendidos no pronto socorro de cirurgia plástica do Distrito Federal. Rev Bras Cir Plast. 2007;22(4):209-12.
19. Pereira MD, Kreninski T, Santos RA et al. Trauma Craniofacial: Perfil epidemiológico de 1223 fraturas atendidas entre 1999 e 2005 no Hospital São Paulo - UNIFESP-EPM. Rev Soc Bras Cir Craniomaxilofac. 2008;11(2):47-50.
20. Filho EF, Fadul Jr.R, Azevedo RA et al. Fraturas de mandíbula: análise de 166 casos. Rev Assoc Med Bras. 2000;46(3):272-6.
1 - Specialist Member of the Plastic Surgery and Burns Service, Santa Casa de isericordia de São José do Rio Preto, SP; Ex - Resident of Plastic Surgery and Burns, Santa Casa de Misericordia de São José do Rio Preto, SP
2 - Specialist Member of the Plastic Surgery and Burns Service, Santa Casa de isericordia de São José do Rio Preto, SP;- Preceptor of the Plastic Surgery and Burns Service, Santa Casa de Misericórdia de São José do Rio Preto, SP
3 - Specialist Member of the Plastic Surgery and Burns Service, Santa Casa de isericordia de São José do Rio Preto, SP;- Preceptor of the Plastic Surgery and Burns Service, Santa Casa de Misericórdia de São José do Rio Preto, SP
4 - Full member and Regent of the Plastic Surgery and Burns Service, Santa Casa de Misericórdia de São José do Rio Preto, SP - Regent of the Plastic Surgery and Burns Service, Santa Casa de Misericordia de São José do Rio Preto
5 - Full member and Head of the Plastic Surgery and Burns Service, Santa Casa de Misericórdia de São José do Rio Preto, SP - Head of the Plastic Surgery and Burns Service, Santa Casa de Misericórdia de São José do Rio Preto, SP
Institution: Santa Casa de Misericórdia de São José do Rio Preto.
Corresponding author:
Pâmela Daniela da Silva Massuia
Street João de Laet, n° 415 - Apt. 84 - Santana
CEP: 02410-010 - São Paulo/SP
E-mail: pamidaniela@yahoo.com.br
Article received: December 10, 2013
Article accepted: June 1, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter