

Original Article - Year 2014 - Volume 29 -
Follicular unit extraction: hair transplant without linear scar
Extração de unidades foliculares: transplante capilar sem cicatriz linear
ABSTRACT
INTRODUCTION: Follicular unit extraction (FUE), which involves harvesting a follicular unit containing between one and three hair follicles, prevents the need for donor area resection in the occipitotemporal region for hair transplantation. This method also avoids the need to dissect the material acquired into follicular units. In this method, the follicular units are directly obtained and extracted using small hollow cylinders (punches) with a diameter of 0.8-1 mm through a circular incision around each follicular unit on the scalp.
METHOD: Over 24 months, we evaluated 77 patients with various forms of alopecia (including androgenic and scarring hair loss, eyebrow loss, and small bald areas) who underwent follicular unit transplant. Twelve patients were women and 65 men, with ages ranging from 19 to 65 years. Seven patients underwent the procedure to correct unsightly and extended scars caused by previous hair transplants performed by conventional techniques. This method requires greater intraoperative care in handling the follicular units to avoid damaging them.
RESULTS: Although the surgical time was increased, no linear scarring was observed, and the donor areas were less visible due to being masked by adjacent hairs from 3 to 5 days after surgery. This was the case even with shaved hair.
CONCLUSION: Although this procedure requires greater care in handling and obtaining follicular units, FUE enables hair transplants without a linear scar. As such, this method has many clinical indications.
Keywords: Alopecia; Follicular Unit Extraction; Donor area without linear scar; FUE; Hair transplant without linear scar.
RESUMO
INTRODUÇÃO: A técnica de extração de unidades foliculares (FUE, do inglês follicular unit extraction), de um a três folículos capilares, dispensa a necessidade de ressecção da área doadora na região occipitotemporal e de outros envolvimentos táticos e técnicos para transformar o material adquirido nessas unidades. Estas são obtidas diretamente, sendo extraídas por meio de pequenos cilindros ocos (punches), com diâmetro variando de 0,8 mm a 1mm, mediante incisão circular ao redor de cada unidade folicular no couro cabeludo e, subsequente, extração.
MÉTODO: Foram avaliados e acompanhados, durante 24 meses, 77 pacientes submetidos a transplante de unidades foliculares, aplicado na correção de áreas de alopecia dos mais diversos tipos (androgênica, em cicatrizes de áreas pilosas, transplantes em supercílios, em pequenas áreas de calvície). Destes, 12 eram do sexo feminino e 65 do masculino, com idades que variavam de 19 a 65 anos; sete pacientes foram operados para correção de cicatrizes inestéticas e alargadas, decorrentes de transplantes capilares anteriores, realizados por técnicas convencionais. Os cuidados transoperatórios na manipulação das unidades foliculares são mais acurados, dada a sutileza de suas estruturas.
RESULTADOS: Apesar do tempo cirúrgico aumentado, não existe cicatriz linear e as áreas doadoras são menos visíveis e totalmente camufláveis pelos cabelos adjacentes no período de 3 a 5 dias de pós-operatório, mesmo com os cabelos raspados.
CONCLUSÃO: O método exige maiores cuidados quanto aos procedimentos táticos e técnicos de manipulação e à obtenção das unidades foliculares.
Palavras-chave: Alopecia; Unidade de Extração Folicular; Área doadora sem Cicatriz Linear. FUE; Transplante capilar sem cicatriz linear.
In obtaining hair follicles for the treatment of alopecia, the occipitotemporal region is often used as the donor area for strip harvesting, which is performed by excising a transverse strip of scalp. The scars left after this procedure vary in appearance and are not always inconspicuous. These scars, even satisfactory and very thin scars, may be seen due to scar keratosis, reduced follicular density in the region, technical limitations, or when the patient has very short or shaved hair. Follicular unit extraction (FUE) was introduced in 20021, as a method of transplanting glabrous areas without the need to perform a strip resection of the donor area of scalp, avoiding subsequent scarring. This procedure has been improved over the years 2-7, through the development of new hollow cylinder "punches" and extraction devices to incise and dissect the tissue from the epidermis. These devices affect only the dermis and subcutaneous tissue, thus isolating and maintaining the integrity of the hair unit.
OBJECTIVE
The aim of this study was to evaluate the outcomes of this technique by analyzing the following parameters: surgical time, appearance of the donor area, and outcomes of the hair transplant in the recipient area.
METHOD
Case selection
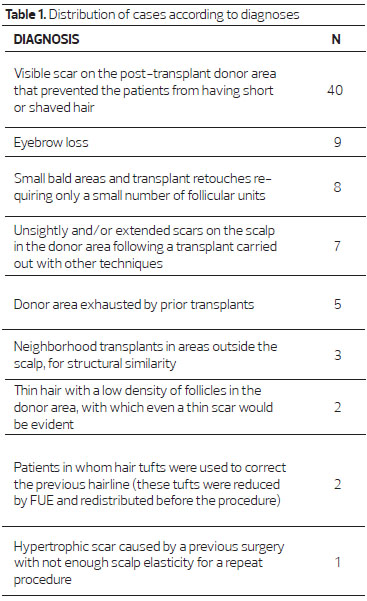
Over 24 months, we evaluated 77 patients who underwent FUE hair transplantation in our clinic, in São Paulo, Brazil. Of these, 12 were women and 65 were men, aged between 19 and 65 years. The patients were divided into nine groups according to the recipient areas, which were all in the cephalic segment. Indications for treatment are illustrated in table 1.
Extractor device and follicular unit
In this study, two types of extraction devices were used, one manual and one electric 1-4, to obtain follicular units of between one and three hair follicles in a single incision.
The FUE procedure involves inserting the free end of the cylinder into the skin, parallel to the hair growth. This penetrates the dermis and subcutaneous tissue to about 1mm beyond the hair bulb. Subsequent removal of the unit is performed with fine forceps. In the manual model, the punch, consisting of a hollow metal cylinder, measuring between 0.8mm and 1mm in diameter with a free cutting edge (Figure 1), is attached to a handle (Figure 1). The electric model has the same body as the manual device, coupled to an adaptor connecting the punch to an electrical supply(Figure 2). In the electric model, punches with free cutting or semi-cutting edges can be used. The semi-cutting punch (blunt system) 4 has the advantage of being able to dissect the subcutaneous tissue, minimizing the rate of injury and graft transection 4,5. It is particularly useful for surgeons who are less experienced at this technique. The electric model works in exactly the same manner as the manual model regarding the three maneuvers described. The electric model rotates as it is inserted, gradually slowing down when it reaches the level of the hair bulb without the need for manual rotation to allow release.

Figure 1. Different diameters of punches used in the follicular unit extraction procedure (left) and large punches used in older techniques (right). In the follicular unit extraction procedure punches with diameters ranging from 0.7mm to 1 mm are used, whereas those used in older techniques have a diameter of 3mm or more.

Figure 2. (A), An unsightly scar aspect and poor aesthetic appearance of the donor area 1 year after follicular unit removal with punches of 3mm in diameter. (B) and (C), Compromising and unsightly outcomes, referred to as "doll hair."
Although apparently uniform, each hair, even in the same area of the same patient, is morphologically different. Between one and three follicles can exit from the same unit on the surface, although they have separate capillary bulbs, are at different depths in the dermis and subcutaneous tissue, and have different stem inclination with respect to the intracutaneous segment (Figure 3). The angle of inclination varies compared to the intracutaneous direction where the hair exits the skin.

Figure 3. (A) and (B), unsatisfactory outcomes and enlarged scars from donor areas subjected to spindle resection and suture.
Therefore, for every one to three follicular units removed, at least one or two follicles should remain intact (Figure 4). As the hair exit varies, it is important to leave the follicles around those that are extracted intact (Figure 5). The smaller the exit angle, that is, the closer the hair is to the skin, the larger the angle of inclination with which the punch penetrates and the bigger the resulting hole (Figure 6).

Figure 4. (A), Patient 1 year after a conventional hair transplant surgery (with strip harvesting of donor area) and satisfactory scar when the hair is 3mm in length. (B), The same patient with hair shaved to 1mm in length, showing the scar.

Figure 5. (A), A patient who underwent a follicular unit extraction procedure with 1,200 follicular units removed, with hair shaved to 1 mm in length, 6 months post-transplant. (B), The same patient with hair shaved close to the scalp and hypochromic points.
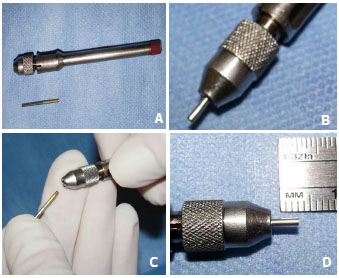
Figure 6. A manual extraction device used for the follicular unit extraction procedure. The punch is connected to a handle and the depth can be adjusted according to the depth of the follicular unit. (A), Handle; (B), Punch of 1 mm; (C), Inserting the punch into the handle; (D), Adjusting the penetration depth.
These details should be considered by the specialist to avoid excessive thinning of the donor area and to reduce the transection rate of the hair bulbs to maximize the number of follicular units extracted and increase the successful integration rate.
Surgical technique
The patients were operated on under mild sedation and local anesthetic with 2% lidocaine and epinephrine 1:200.000. The donor area in the occipital and temporal regions is shaved with an electric razor, leaving residual hairs of 1 mm to 1.5 mm long. The size of the area to be shaved was estimated by the number of follicular units to be used (Figure 7).
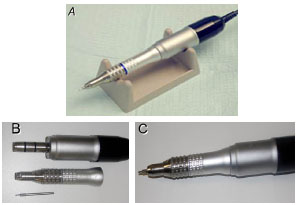
Figure 7. (A), Model of the electric extraction device * used for the follicular unit extraction procedure. (B), Disassembled device showing the punch and the adapter. (C), The assembled extraction device. (* The Safe System, one of the motorized devices used for the extraction of follicular unities, uses a blind (blunt) punch and decelerates when this punch penetrates the dermis).
Lenses with a 5-10× magnification and a powerful light source were used for magnification. Obtaining the follicular units to be transplanted into the recipient bed is then carried out according to the following steps:
I: The tip of the follicular extraction device is positioned parallel to the angle of inclination, aligned with the hair exit point, and pressed against the skin.
II: The free cutting edge is pressed into the skin, penetrating the epidermis, dermis, and part of the depth of the subcutaneous tissue. This is followed by rotation around the follicular unit and removal of the extraction device (Figure 8).
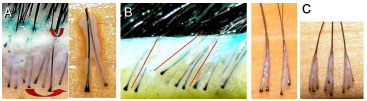
Figure 8. (A), Follicular units in bundles on the surface of the skin showing their distribution in the subcutaneous tissue. (B), The red lines indicate the variation of the inclination angles of the exit of the hair follicle through the skin. (C), Different positions and depths of the roots within the same follicular unit.
III: Extraction of the follicular unit with fine forceps (Figure 9).
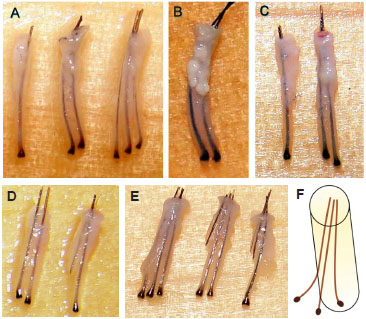
Figure 9. (A) and (B), Intact follicular units (without root transection) removed by follicular unit extraction with a punch 1 mm in diameter. (C), Intact follicular units (without root transection) removed by follicular unit extraction with a punch 0.8 mm in diameter. The punch diameter is gradually decreased, according to the improving skill of the surgeon. (D) and (E), Intact units on the left and transected units in the middle and right. F, Mode of transection by the punch.
Inserting the punch to its full depth should be avoided, as this significantly increases the rate of root transection. The first two or three follicles extracted are used as depth parameters and only partial penetration of the punch up to the depth measured is allowed (Figure 10). Under the microscope, only excess epidermis is removed from the units, which are subsequently maintained in saline solution at 4ºC until transplant into the receiving areas (Figure 11). The removal should be carried out within a safety area, that is, only the hair follicles that do not have the genetic code for baldness should be removed. Due to this predisposition, follicles near to the crown will fail in the future and cause hypochromic punctate scars in all the bald areas. Occlusive dressings are not used, and only antibiotic ointment is applied to the donor area. Once the FUE procedure is completed, the transplant proceeds conventionally, with the follicular units transplanted into bald areas with the aid of blades measuring from 0.7mm to 0.9mm in diameter (Figures 12 and 13). The patient is then discharged approximately 30 min after surgery.

Figure 10. In (A, B and C), the safety region for follicular unit extraction is shown within the demarcated area. The areas outside these zones can include follicles with the genetic code for baldness, which, therefore, may fall out in the future and generate hypochromic scars on glabrous areas.
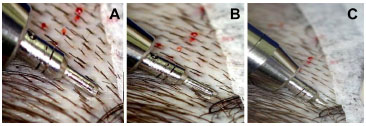
Figure 11. A, Sequence showing the correct alignment of the punch (A), engagement of the punch (B) and partial penetration of the punch around the follicular unit (C). The punch should be aligned with the angle of hair exit and penetrate only partially.
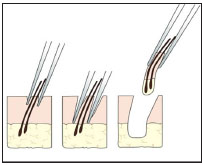
Figure 12. Schematic appearance showing follicular unit extraction with fine forceps and traction in the same direction of hair exit, after partial penetration of the punch.
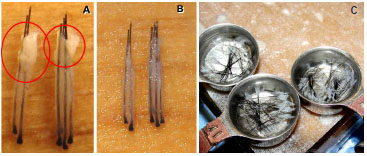
Figure 13. (A), Follicular units removed with the follicular unit extraction procedure. (B), Follicular units after removing the excess epidermis. (C), Units containing one, two, and three strands, placed in saline and cooled to 4ºC.
Care and postoperative management
The first head washing is carried out the day after the transplant at the clinic, using degerming shampoo. The patient is advised to wash the head once a day for the next few days, and to avoid rubbing too hard and removing the transplanted units. The holes caused by FUE are already smaller the day after the procedure and are closed completely 3 or 4 days post-transplant. On the fifth postoperative day, the adjacent hairs already fully camouflage the donor areas. Postoperative follow up is scheduled for the day after the procedure, after 15 days, and after 6 months to evaluate the partial outcome and after 1 year to assess the final result. When necessary, further implants should be carried out 9-12 months after the first procedure, using units removed from the donor area between the punctate scars.
Approval by an ethics committee (CEP) was not needed because the study was carried out at a private clinic. However, it is worth noting that in this study all ethical standards were respected.
RESULTS
The surgery lasts between 6 and 8h, with an average of 7 h, depending on the number of transplanted units. The donor areas leave no visible scars, as there is no need for resection of the scalp segment or sutures in the donor area. No complications were observed compared with conventional resection technique and scalp suture. However, cysts occurred in 1% of patients, and were spontaneously reabsorbed. The integration rate of the grafts was 100%. The losses reported occurred only in cases in which the surgery lasted more than 8h and were caused by bulb dehydration of the follicular units and trauma in the implantation. The final outcome was considered satisfactory in all cases, with a satisfactory outcome determined as one that was in line with the realistic expectations of the patient according to the accurate information previously provided on the limitations and possibilities of this technique. The number of patients who had unrealistic expectations for hair density was not statistically significant. In this series, 90% of the patients underwent a second surgery and 3% a third procedure.
DISCUSSION
FUE requires high precision and the use of powerful magnifying lenses. This technique differs from those that use caliber punches with diameters between 2mm and 3mm (Figure 14), which cause scarring to the donor area as well as an artificial appearance to the transplanted regions. It also removes the unsightly appearance of a scar in the donor area as is seen following strip harvesting (Figure 15), which is generally fusiform and transversely positioned, causing a scar of variable length and width according to the size of the glabrous area to be transplanted (Figure 16). When the technique is performed carefully, this scar can be completely camouflaged between the longer hairs. However, it becomes eventually evident when the hair is shaved closed to the scalp (Figure 17).

Figure 14. (A), Immediate postoperative appearance of the occipital region after removal of 1,561 follicular units with a punch 0.9mm in diameter. (B) and (C), First and seventh days after surgery, respectively. (D), Immediate postoperative appearance of the left occipitotemporal region and in (E), fifth postoperative day. In both cases, a punch 0.8mm in diameter was used.

Figure 15. Donor areas exhausted by multiple previous transplants.
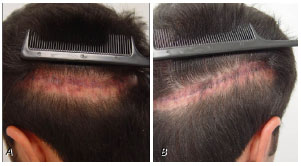
Figure 16. Patient with a donor area without elasticity, which generated a hypertrophic scar 1 year after a transplant surgery by conventional technique. We plan to treat the scar and, if necessary, perform a new hair transplant, in which the follicular unit extraction procedure will be used.

Figure 17. Follicular unit extraction procedure of beard, as an example of the use of hair follicles from other parts of the body when the donor area is exhausted. In this case, 917 follicular units were removed from the beard. Courtesy of Dr. Robert True. In the detail, beard vs. scalp follicle. Notice the difference in thickness.
The main advantage of FUE is the absence of a linear scar in the donor area. It is therefore indicated for those who want to have their hair shaved or for those who have an aversion to having a scar, no matter how thin, imperceptible, and camouflaged by hairs (Figure 18). It is important to notice that, even in the absence of a linear scar, every extraction generates a punctuated hypochromic scar, varying from 0.5mm to 0.7mm in diameter. These scars are easily camouflaged even when the hair is shaved to only 1mm long. Even if hair was shaved close to the scalp, the hypochromic points are visible only on very close inspection (Figure 19).
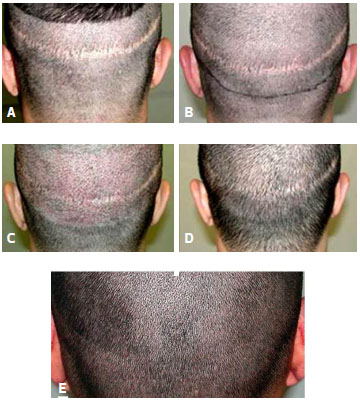
Figure 18. (A) and (B), Images before correction of the donor area. (C), First postoperative day. (D), Sixth postoperative day. (E), One year after surgery, with two transplant sessions, for a total of 927 follicular units.
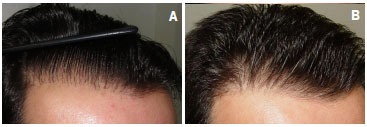
Figure 19. A 42-year-old patient who had undergone two previous surgeries and was dissatisfied with the naturalness of the front line. (A), Figure before the correction of the previous hairline. This was treated with transplantation of 1,025 follicular units, removed by follicular unit extraction procedure, in a single surgical step. (B), One year after corrective surgery.
The indications for this procedure are multiple, including a donor area that is exhausted by multiple previous transplants and unable to undergo new fusiform resection (Figure 20), donor areas with fine hair or low follicular density (Figure 21), and donor areas without elasticity or prone to hypertrophic scars. The possibility of using hair units from other areas of the body when the first area is exhausted (for example, beard and chest) is another considerable advantage. It is also suitable for the treatment of small areas of baldness that require a reduced number of follicular units, such as the eyebrows. The camouflage of scars resulting from previous hair transplants for patients wishing to have very short or shaved hair can be included among the best indications, even when scars are thin, unsightly, or hypertrophic. Due to the exclusivity of this method, our statistics account for almost 30% of performed transplants. There are specific indications for the use of this technique in small areas with alopecia or as a complementary technique due to the poor quality of previous results.

Figure 20. Before and 1 year after surgery by the FUE procedure. A 33-year-old patient, a military personnel, required to have very short hair. Option by FUE procedure with 2,127 transplanted units.

Figure 21. A 32-year-old patient who underwent transplant of 220 follicular units to the eyebrow on both sides. The units were removed by the follicular unit extraction procedure. (A), Preoperative image. (B), Outcome 6 months after surgery showing increased follicular density of the outer tail of the eyebrows.
Among the disadvantages, we reported increased surgical time and fewer follicles removed. These observations restrict the procedure to the indications previously specified.
The follicular units differ in the number of follicles (from one to three), levels and separation between them, and the inclination angle of the outer hair stem with respect to the intracutaneous segment. When using the extraction device, the surgeon needs to be familiar with the appearance of the first hair follicles removed and follow a similar method for the other units to reduce the incidence of loss of viability caused by transection. A decreased damage rate is linked to correctly surrounding the follicular unit with the cutting cylinder, the correct control of the depth of the punch, and the delicate extraction of the capillary unit with a forceps without compromising the vitality of the follicle or, at least, with low incidence of this occurrence, given the variation in inclination of the hairs.
The usual recommendation is the removal of 2-3 initial units that serve as a model to evaluate the depth of the remaining follicular units in their respective donor areas. It must be noted that there is a greater risk of dehydration of follicular units than in the traditional method. As these units are extracted, usually the subcutaneous cellular tissue around the bulbs is scarcer and therefore more prone to dehydration. We therefore need to consider the long time that these units remain outside the scalp and the risk of microtrauma. These problems are reduced by the maintenance of follicular units by immersion in cold saline solution and care in handling these structures.
Hair unit extraction with a forceps can result in its partial or total retention in the dissected area and epithelial layer, with or without the dermis separated from the subcutaneous tissue. This type of occurrence does not exceed 2% of the units removed. They are left in the region to heal naturally. Rarely, isolated cysts were identified and subsequently removed.
The variation in the follicular units described determines the rate of follicular bulb transection. Bulb transection is more likely where there is a greater distance between the hair and the bulb, a drastic change of the angle of hair exit related to its intracutaneous segment, depth differences between the bulbs (in the flattest follicles, around 3mm), white hair, and, in particular, curly hair, which, due to the curve morphology, have higher rates of root transection.
Our initial experiences, using a manual extraction device followed by the electric extraction device, had a bulb transection rate of between 20% and 30% in the first 20 cases, dropping to 10% since then 5. Although several types of electric extraction devices are commercialized, it is necessary to take into account the familiarity of the surgeon with the instrument as well as their skill. Already available in the United States is a robot that performs the FUE procedure. However, in our opinion, it cannot replace the human hand. Despite an apparent uniformity in the deployment and withdrawal of the extraction device as well as qualification of the surgeon, there are still no case studies and insufficient data showing that the percentage of integration of transplanted units is the same compared to that in conventional techniques. However, this case series has shown that this might be the case. More specific and conclusive studies on this subject are in progress.
CONCLUSION
The FUE procedure, using manual or electric devices, is indicated in any case of hair transplant, being more appropriate in cases in which the patient would like to avoid a linear scar or cover an existing scar or in cases where follicles are obtained from other parts of the body. The method of obtaining follicles from skin regions 0.8mm to 1mm in diameter allows the avoidance of donor area resection and scarring. The remaining spaces between the follicles taken can be used to supplement a new transplant in this area or in another receiving area.
REFERENCES
1. Rassman WR, Bernstein RM, McClellan R, Jones R, Worton E, Uyttendaele H. Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28:720-8.
2. Harris JA. New methodology and instrumentation for follicular unit extraction: lower follicle transaction and expanded patient candidacy. Dermatol Surg. 2006;32:56-62.
3. Onda M, Igawa HH, Inoue K, Tanino R. Novel technique of follicular unit hair transplantation with a powered punching device. Dermatol Surg. 2008;34:1683-8.
4. Harris JA. Follicular unit extraction: the SAFE System. Hair Transplant Forum Internat. 2004;14:157-63.
5. Ruston A. FUE learning curve: 19th International Society of Hair Restoration Surgery Annual Meeting - Anchorage, Alaska - October 2011.
6. Ruston A. Small details can make a great difference in hair transplant surgery. Hair Transplant Forum International. 2010;(20):146-1.
7. Ruston A. FUE: Ideas to Improve Efficiency, Speed and Integration: 22nd International Society of Hair Restoration Surgery Annual Meeting - Kuala Lumpur, Malaysia -October 2014
1 - Specialist Member of the Brazilian Society of Plastic Surgery. Member of the International Society of Hair Restoration Surgery. Member of the American Society of Aesthetic Plastic Surgery. Member of the Brazilian Society of Hair Restoration Surgery
2 - Member of the Brazilian Society of Plastic Surgery - BSPS
3 - Member of the Brazilian Society of Plastic Surgery - BSPS
Institution: Ruston Clinic.
Corresponding author:
Antonio Ruston
Alameda Jau, 796 - 400
São Paulo - SP - Brazil
Fone: 55 - 11 - 3031-1221
E.mail: info@ruston.com.br
Article submitted: July 23, 2013
Article accepted: March 4, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter